Abstract
Purpose
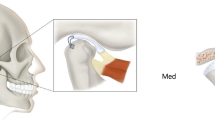
The aim of this study was to determine the efficacy of arthroscopic lysis and lavage on pain in patients with unilateral Wilkes stage III derangement of the temporomandibular joint. Authors retrospectively evaluated whether the arthroscopic lysis and lavage has an impact on pain decrease in patients with moderate osteoarthritis.
Methods
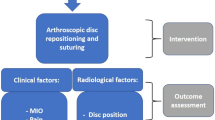
Patients with unilateral Wilkes III of temporomandibular joint were included in this study. All patients underwent arthroscopic lysis and lavage (ASC-L), assessed pain before and after the procedure (primary outcome variable), maximal interincisal opening (MIO) was recorded as secondary outcome variable. The patients also subjectively assessed whether they were satisfied with the outcome of the arthroscopy or whether their condition required further interventions. The disc position was evaluated by magnetic resonance imaging (MRI) 24 months after the arthroscopy and compared with the disc position on the MRI prior to the arthroscopy. The R Project for Statistical Computing 3.4.1 and the Gretl Pro programs were used for statistical analysis. In addition to the descriptive statistics methods, the Shapiro-Wilk normality test was used to verify data normality and the two sample t test used to test the hypotheses themselves.
Results
The sample consisted of 62 patients who underwent arthroscopic lysis and lavage (ASC-L) in 2015 and 2016. It included 6 men and 56 women with an average age of 34.37. Pain and MIO were recorded during regular check-ups 1, 3, 6, 12, and 24 months. A therapeutic effect (MIO over 34 mm, VAS score 0–1) was recorded in 69% of cases 24 months after the ASC-L. Nonetheless, the work demonstrated the importance of subjective assessment, as 87% of patients perceived their condition as satisfactory after 24 months and not requiring further intervention, while 8 patients (13%) perceived it as unsatisfactory. Disc reposition 24 months following the ASC-L was recorded in only 44% of patients who assessed their condition as satisfactory. Patients with persistent disc dislocation 24 months after the arthroscopy were older, had a lower average maximal interincisal opening value before the ASC-L and a longer duration of mandibular movement restriction before the ASC-L (evaluated as a statistically significant difference).
Conclusion
In this study, the authors confirmed that ASC-L is an effective therapeutic method in patients with WIII, from both clinical and subjective perspectives. This work demonstrated that improvement in patients with Wilkes stage III is not related to disc reposition. Postoperative physiotherapy is an integral component of ASC-L and is reflected in the final results.


Similar content being viewed by others
References
Wilkes CH (1989) Internal derangement of the temporomandibular joint: pathological variations. Arch Otolaryngol Head Neck Surg 115:469–477
Martins-Júnior RL, Palma AJ, Marquardt EJ, Gondin TM, Kerber FC (2010) Temporomandibular disorders: a report of 124 patients. J Contemp Dent Pract 11(5):071–078
Goncalves DA, Dal Fabbro AL, Campos JA, Bigal ME, Speciali JG (2010) Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain 24:270–278
Murphy MK, MacBarb RF, Wong ME, Athanasiou KA (2013) Temporomandibular joint disorders: a review of etiology, clinical management, and tissue engineering strategies. Int J Oral Maxillofac Implants 28(6):e393–e414
Dimitroulis G (2005) The prevalence of osteoarthrosis in cases of advanced internal derangement of the temporomandibular joint: a clinical, surgical and histological study. Int J Oral Maxillofac Surg 34:345–349
Ohnishi A (1975) Arthroscopy of the temporomandibular joint. J Jpn Stomatol Assoc 42:207–213
Sanders B (1986) Arthroscopic surgery of the temporomandibular joint: treatment of internal derangement with persistent closed lock. Oral Surg Oral Med Oral Pathol 62:361–372
Machon V, Sedy J, Klima K, Hirjak D, Foltan R (2012) Arthroscopic lysis and lavage in patients with temporomandibular anterior disc displacement without reduction. Int J Oral Maxillofac Surg 41(1):109–113
Dimitroulis G (2002) A review of 56 cases of chronic closed lock treated with temporomandibular joint arthroscopy. J Oral Maxillofac Surg 60(5):519–524
Holmlund A, Gynther G, Axelsson S (1994) Efficacy of arthroscopic lysis and lavage in patients with chronic locking of the temporomandibular joint. Int J Oral Maxillofac Surg 23(5):262–265
McCain JP, Sanders B, Koslin MG, Quinn JH, Peters PB, Indresano AT (1992) Temporomandibular joint arthroscopy: a 6-year multicenter retrospective study of 4,831 joints. J Oral Maxillofac Surg 50(9):926–930
Murakami K, Segami N, Okamoto M, Yamamura I, Takahashi K, Tsuboi Y (2000) Outcome of arthroscopic surgery for internal derangement of the temporomandibular joint: long-term results covering 10 years. J Craniomaxillofac Surg 28(5):264–271
Breik O, Devrukhkar V, Dimitroulis G (2016) Temporomandibular joint (TMJ) arthroscopic lysis and lavage: outcomes and rate of progression to open surgery. J Craniomaxillofac Surg 44(12):1988–1995
Manfredini D (2009) Etiopathogenesis of disc displacement of the temporomandibular joint: a review of the mechanism Ind. J Dent Res 20:212–221
Tenenbaum HC, Freeman BV, Psutka DJ, Baker GI (1999) Temporomandibular disorders: disc displacement. J Orofac Pain 13:285–290
McCain JP, Hassameldin RH, Srouji S, Maher A (2015) Arthroscopic discopexy is effective in managing temporomandibular joint internal derangement in patients with Wilkes stage II and III. Anesth/Facial Pain 73(3):391–401
Randolph CS, Greene CS, Moretti R, Forbes D, Perry HT (1990) Conservative management of temporomandibular disorders: a post treatment comparison between patients from a university clinic and from private practice. Am J Orthod Dentofac Orthop 98:77
Machon V (2017) Manual of TMJ Surgery; the Prague approach. Business Media Praha, Prague
McCain JP (1988) Arthroscopy of the human temporomandibular joint. J Oral Maxillofac Surg 46(8):648–655
Abboud WA, Yarom N, Yahalom R, Joachim M, Reiter S, Koren O, Elishoov H (2018) Comparison of two physiotherapy programmes for rehabilitation after temporomandibular joint arthroscopy. Int J Oral Maxillofac Surg 47(6):755–761
Holmlund AB, Axelsson S (1996) Temporomandibular arthropathy: correlation between clinical signs and symptoms and arthroscopic findings. Int J Oral Maxillofac Surg 25(3):178–181
Zhang S, Liu X, Yang C, Cai X, Chen M, Haddad MS, Yun B, Chen Z (2009) Intra-articular adhesions of the temporomandibular joint: relation between arthroscopic findings and clinical symptoms. BMC Muskuloskelet Disord 17:10–17
González-García R, Rodríguez-Campo FJ, Monje F, Sastre-Pérez J, Gil-Díez Usandizaga JL (2008) Operative versus simple arthroscopic surgery for chronic closed lock of the temporomandibular joint: a clinical study of 344 arthroscopic procedures. Int J Oral Maxillofac Surg 37(9):790–796
Al-Moraissi EA (2015) Open versus arthroscopic surgery for the management of internal derangement of the temporomandibular joint: a meta-analysis of the literature. Int J Oral Maxillofac Surg 44(6):763–770
Sato J, Segami N, Nishimura M, Yoshimura H, Demura N, Yoshitake Y, Nishikawa K (2003) Correlation between the arthroscopic diagnosis of synovitis and microvessel density in synovial tissues in patients with internal derangement of the temporomandibular joint. J Craniomaxillofac Surg 31:101–106
Hamada Y, Kondoh T, Holmlund AB, Nakajima T, Horie A, Saito T, Nomura Y, Seto K (2006) One-year clinical course following visually guided irrigation for chronic closed lock of the temporomandibular joint Oral. Surg Oral Med Oral Pathol Oral Radiol Endod 101:170–174
Ulmner M, KrugerWeiner C, Lund B (2017) Predictive factors in temporomandibular joint arthroscopy: a prospective cohort short-term outcome study. J Oral Maxillofac Surg 75:1643e1–1643e7
Smolka W, Yanai C, Smolka K, Iizuka T (2008) Efficiency of arthroscopic lysis and lavage for internal derangement of the temporomandibular joint correlated with Wilkes classification. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:317–323
Hossameldin RH, McCain JP (2018) Outcomes of office-based temporomandibular joint arthroscopy: a 5-year retrospective study. Int J Oral Maxillofac Surg 47(1):90–97
Murakami KI, Tsuboi K, Bessho K, Yokoe Y, Nishida M, Iizuka T (1998) Outcome of arthroscopic surgery to the temporomandibular joint correlates with stage of internal derangement: five-year follow-up study. Br J Oral Maxillofac Surg 36:30–34
Ahmed N, Sidebottom A, O’Connor M, Kerr HL (2012) Prospective outcome assessment of the therapeutic benefits of arthroscopy and arthrocentesis of the temporomandibular joint. Br J Oral Maxillofac Surg 50(8):745–748
Moses JJ, Poker ID (1989) TMJ arthroscopic surgery: an analysis of 237 patients. J Oral Maxillofac Surg 47(8):790–794
Okeson JP (2008) Management of temporomandibular disorders and occlusion, 6th edn. Mosby Elsevier, p 631
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Machoň, V., Levorová, J., Hirjak, D. et al. Does arthroscopic lysis and lavage in subjects with Wilkes III internal derangement reduce pain?. Oral Maxillofac Surg 25, 463–470 (2021). https://doi.org/10.1007/s10006-020-00935-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-020-00935-7