Abstract
Purpose
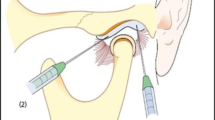
Arthrocentesis of the temporomandibular joint (TMJ) is a minimally invasive surgical procedure that provides good clinical results such as the improvement of jaw movements. It also helps to balance the synovial liquid viscosity and relieve TMJ pain by the washout of inflammatory components from the upper compartment. The purpose of this study is to report a case series of patients submitted to a clinical-based protocol of diagnosis of TMJ joint open lock and treatment with arthrocentesis.
Material and methods
Patients suffering from a recurrent unilateral open lock of the TMJ were submitted to one arthrocentesis of the affected TMJ and all of them reported that the open lock was caused by daily stomatognathic activities. To decide the arthrocentesis as the initial treatment of these patients, the authors followed a rational protocol of diagnosis.
Results
Ten patients were included in the present study. No complications occurred during arthrocentesis. Immediately, 1 week, 1 month, and 6 months after arthrocentesis, patients did not suffer from open lock or disc click anymore. They also reported no more pain because it was strictly related to the disc click.
Conclusions
All patients of the present study improved from the open lock and disc click of the affected TMJ for 6 months after arthrocentesis. The clinical-based protocol of diagnosis of TMJ open lock reported in the present study, followed by the treatment with arthrocentesis is a reasonable, low-cost, and safe method to treat patients with the acute open lock.


Similar content being viewed by others
References
Sembronio S, Albiero AM, Toro C, Robiony M, Politi M (2008) Is there a role for arthrocentesis in recapturing the displaced disc in patients with closed lock of the temporomandibular joint? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:274–280. https://doi.org/10.1016/j.tripleo.2007.07.003
Carvajal WA, Laskin DM (2000) Long-term evaluation of arthrocentesis for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg 58:852–855
Nitzan DW (2002) Temporomandibular joint “open lock” versus condylar dislocation: signs and symptoms, imaging, treatment, and pathogenesis. J Oral Maxillofac Surg 60:506–511. https://doi.org/10.1053/joms.2002.31846
Kai S, Kai H, Nakayama E, Tabata O, Tashiro H, Miyajima T, Sasaguri M (1992) Clinical symptoms of open lock position of the condyle. Relation to anterior dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 74:143–148. https://doi.org/10.1016/0030-4220(92)90372-W
Barkin S, Weinberg S (2000) Internal derangements of the temporomandibular joint: the role of arthroscopic surgery and arthrocentesis. J Can Dent Assoc 66:199–203
Ziccardi VB, Nizam SA II (2018) Arthrocentesis of the temporomandibular joint. In: Fonseca RJ (ed) Oral and maxillofacial surgery, volume 2. 3rd ed. Elsevier, Riverport Ln, pp 883–891
da Silva YS, Grillo R (2011) Injeções intra-articulares de corticosteróides versus hialuronato de sódio para tratamento de desarranjos internos da articulação temporomandibular. Odonto 19:105–114. https://doi.org/10.15603/2176-1000/odonto.v19n38p105-114
Emshoff R, Rudisch A, Bösch R, Strobl H (2003) Prognostic indicators of the outcome of arthrocentesis: a short-term follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96:12–18. https://doi.org/10.1016/S1079-2104(03)00219-1
Nitzan DW (2001) The process of lubrication impairment and its involvement in temporomandibular joint disc displacement: a theoretical concept. J Oral Maxillofac Surg 59:36–45. https://doi.org/10.1053/joms.2001.19278
Emshoff R (2005) Clinical factors affecting the outcome of arthrocentesis and hydraulic distension of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100:409–414. https://doi.org/10.1016/j.tripleo.2004.12.024
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Informed consent
It is not possible to recognize the patient of the present study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Slusarenko da Silva, Y., Borba, A.M. & Naclério-Homem, M. A clinical-based protocol of diagnosis of temporomandibular joint open lock and treatment with arthrocentesis. Oral Maxillofac Surg 24, 211–215 (2020). https://doi.org/10.1007/s10006-020-00844-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-020-00844-9