Abstract
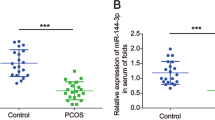
Polycystic ovary syndrome (PCOS) is a common endocrinopathy related to female infertility. We investigated the function of the microRNA-98-3p (miR-98-3p)/Yin-Yang-1 (YY1) axis to the pathophysiological processes in PCOS mice. A mouse model of PCOS was established using dehydroepiandrosterone (DHEA). Hematoxylin and eosin (HE) staining was used to assess morphologic changes of the ovaries. Hormonal serum levels were measured by ELISA. Estrogen synthesis in OGCs was measured using chemiluminescence immunoassay. The viability, cell cycle, and apoptosis of ovarian granulosa cells (OGCs) were assessed by CCK-8, flow cytometry, and western blot. Luciferase reporter assays were conducted to examine the binding of miR-98-3p to YY1. YY1 was upregulated, while miR-98-3p was downregulated both in the ovarian tissues of PCOS mice and OGCs separated from PCOS mice and patients. YY1 Knockdown promoted OGC proliferation and inhibited apoptosis as well as increased estrogen production in OGCs. YY1 was verified to be targeted by miR-98-3p. Additionally, YY1 overexpression prevented the effects of miR-98-3p overexpression on the proliferation and apoptosis of OGCs. Importantly, miR-98-3p attenuated ovarian injury in PCOS mice. MiR-98-3p targets and downregulates YY1 expression, thereby affecting the proliferation and apoptosis of OGCs in PCOS.






Similar content being viewed by others
References
Azziz R, Carmina E, Chen Z, Dunaif A, Laven JS, Legro RS, Lizneva D, Natterson-Horowtiz B, Teede HJ, Yildiz BO (2016) Polycystic ovary syndrome. Nat Rev Dis Primers 2:16057. https://doi.org/10.1038/nrdp.2016.57
Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, Carmina E, Chang J, Yildiz BO, Laven JS, Boivin J, Petraglia F, Wijeyeratne CN, Norman RJ, Dunaif A, Franks S, Wild RA, Dumesic D, Barnhart K (2012) Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril 97(1):28-38.e25. https://doi.org/10.1016/j.fertnstert.2011.09.024
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ (2018) Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril 110(3):364–379. https://doi.org/10.1016/j.fertnstert.2018.05.004
Burghen GA, Givens JR, Kitabchi AE (1980) Correlation of hyperandrogenism with hyperinsulinism in polycystic ovarian disease. J Clin Endocrinol Metab 50(1):113–116. https://doi.org/10.1210/jcem-50-1-113
Diamanti-Kandarakis E, Dunaif A (2012) Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev 33(6):981–1030. https://doi.org/10.1210/er.2011-1034
Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, Welt CK (2013) Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 98(12):4565–4592. https://doi.org/10.1210/jc.2013-2350
de Medeiros SF, Rodgers RJ, Norman RJ (2021) Adipocyte and steroidogenic cell cross-talk in polycystic ovary syndrome. Hum Reprod Update. https://doi.org/10.1093/humupd/dmab004
Palko L, Bass HW, Beyrouthy MJ, Hurt MM (2004) The Yin Yang-1 (YY1) protein undergoes a DNA-replication-associated switch in localization from the cytoplasm to the nucleus at the onset of S phase. J Cell Sci 117(Pt 3):465–476. https://doi.org/10.1242/jcs.00870
Du J, Zhang P, Luo J, Shen L, Zhang S, Gu H, He J, Wang L, Zhao X, Gan M, Yang L, Niu L, Zhao Y, Tang Q, Tang G, Jiang D, Jiang Y, Li M, Jiang A, Jin L, Ma J, Shuai S, Bai L, Wang J, Zeng B, Wu D, Li X, Zhu L (2021) Dietary betaine prevents obesity through gut microbiota-drived microRNA-378a family. Gut Microbes 13(1):1–19. https://doi.org/10.1080/19490976.2020.1862612
Santiago FS, Li Y, Zhong L, Raftery MJ, Lins L, Khachigian LM (2021) Truncated YY1 interacts with BASP1 through a 339KLK341 motif in YY1 and suppresses vascular smooth muscle cell growth and intimal hyperplasia after vascular injury. Cardiovasc Res. https://doi.org/10.1093/cvr/cvab021
Gao P, Li L, Yang L, Gui D, Zhang J, Han J, Wang J, Wang N, Lu J, Chen S, Hou L, Sun H, Xie L, Zhou J, Peng C, Lu Y, Peng X, Wang C, Miao J, Ozcan U, Huang Y, Jia W, Liu J (2019) Yin Yang 1 protein ameliorates diabetic nephropathy pathology through transcriptional repression of TGFβ1. Sci Trans Med. https://doi.org/10.1126/scitranslmed.aaw2050
Bhaskar Rao D, Panneerpandian P, Balakrishnan K, Ganesan K (2021) YY1 regulated transcription-based stratification of gastric tumors and identification of potential therapeutic candidates. J Cell Commun Sig 15(2):251–267. https://doi.org/10.1007/s12079-021-00608-4
Griffith GJ, Trask MC, Hiller J, Walentuk M, Pawlak JB, Tremblay KD, Mager J (2011) Yin-yang1 is required in the mammalian oocyte for follicle expansion. Biol Reprod 84(4):654–663. https://doi.org/10.1095/biolreprod.110.087213
Jin L, Yang Q, Zhou C, Liu L, Wang H, Hou M, Wu Y, Shi F, Sheng J, Huang H (2018) Profiles for long non-coding RNAs in ovarian granulosa cells from women with PCOS with or without hyperandrogenism. Reprod Biomed Online 37(5):613–623. https://doi.org/10.1016/j.rbmo.2018.08.005
Krol J, Loedige I, Filipowicz W (2010) The widespread regulation of microRNA biogenesis, function and decay. Nat Rev Genet 11(9):597–610. https://doi.org/10.1038/nrg2843
Ghildiyal M, Zamore PD (2009) Small silencing RNAs: an expanding universe. Nat Rev Genet 10(2):94–108. https://doi.org/10.1038/nrg2504
Ha M, Kim VN (2014) Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol 15(8):509–524. https://doi.org/10.1038/nrm3838
Teague EM, Print CG, Hull ML (2010) The role of microRNAs in endometriosis and associated reproductive conditions. Hum Reprod Update 16(2):142–165. https://doi.org/10.1093/humupd/dmp034
McCallie B, Schoolcraft WB, Katz-Jaffe MG (2010) Aberration of blastocyst microRNA expression is associated with human infertility. Fertil Steril 93(7):2374–2382. https://doi.org/10.1016/j.fertnstert.2009.01.069
Das M, Djahanbakhch O, Hacihanefioglu B, Saridogan E, Ikram M, Ghali L, Raveendran M, Storey A (2008) Granulosa cell survival and proliferation are altered in polycystic ovary syndrome. J Clin Endocrinol Metab 93(3):881–887. https://doi.org/10.1210/jc.2007-1650
Jiang L, Huang J, Li L, Chen Y, Chen X, Zhao X, Yang D (2015) MicroRNA-93 promotes ovarian granulosa cells proliferation through targeting CDKN1A in polycystic ovarian syndrome. J Clin Endocrinol Metab 100(5):E729-738. https://doi.org/10.1210/jc.2014-3827
Wang M, Sun J, Xu B, Chrusciel M, Gao J, Bazert M, Stelmaszewska J, Xu Y, Zhang H, Pawelczyk L, Sun F, Tsang SY, Rahman N, Wolczynski S, Li X (2018) Functional characterization of MicroRNA-27a-3p expression in human polycystic ovary syndrome. Endocrinology 159(1):297–309. https://doi.org/10.1210/en.2017-00219
Brûlé S, Sayasith K, Sirois J, Silversides DW, Lussier JG (2007) Structure of the bovine VASAP-60/PRKCSH gene, functional analysis of the promoter, and gene expression analysis. Gene 391(1–2):63–75. https://doi.org/10.1016/j.gene.2006.12.012
Qian S, Wang W, Li M (2020) Transcriptional factor Yin Yang 1 facilitates the stemness of ovarian cancer via suppressing miR-99a activity through enhancing its deacetylation level. Biomed Pharmacother 126:110085. https://doi.org/10.1016/j.biopha.2020.110085
Dai J, Wei RJ, Li R, Feng JB, Yu YL, Liu PS (2016) A study of CCND1 with epithelial ovarian cancer cell proliferation and apoptosis. Eur Rev Med Pharmacol Sci 20(20):4230–4235
Kozar K, Ciemerych MA, Rebel VI, Shigematsu H, Zagozdzon A, Sicinska E, Geng Y, Yu Q, Bhattacharya S, Bronson RT, Akashi K, Sicinski P (2004) Mouse development and cell proliferation in the absence of D-cyclins. Cell 118(4):477–491. https://doi.org/10.1016/j.cell.2004.07.025
Chen LJ, Chuang L, Huang YH, Zhou J, Lim SH, Lee CI, Lin WW, Lin TE, Wang WL, Chen L, Chien S, Chiu JJ (2015) MicroRNA mediation of endothelial inflammatory response to smooth muscle cells and its inhibition by atheroprotective shear stress. Circ Res 116(7):1157–1169. https://doi.org/10.1161/circresaha.116.305987
Zhang G, Chen L, Guo X, Wang H, Chen W, Wu G, Gu B, Miao W, Kong J, Jin X, Yi G, You Y, Su X, Gu N (2018) Comparative analysis of microRNA expression profiles of exosomes derived from normal and hypoxic preconditioning human neural stem cells by next generation sequencing. J Biomed Nanotechnol 14(6):1075–1089. https://doi.org/10.1166/jbn.2018.2567
Wood SH, van Dam S, Craig T, Tacutu R, O’Toole A, Merry BJ, de Magalhães JP (2015) Transcriptome analysis in calorie-restricted rats implicates epigenetic and post-translational mechanisms in neuroprotection and aging. Genome Biol 16:285. https://doi.org/10.1186/s13059-015-0847-2
Funding
Demonstration and Application of Appropriate Techniques for Common Injuries in Typical Districts and Counties of Chongqing (No. cstc2016kjhmpt1001-3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no declarations of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, M., Gao, T. & Du, Y. MiR-98-3p regulates ovarian granulosa cell proliferation and apoptosis in polycystic ovary syndrome by targeting YY1. Med Mol Morphol 55, 47–59 (2022). https://doi.org/10.1007/s00795-021-00307-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00795-021-00307-4