Abstract
In the past 10 years, there has been a growing interest in self-injurious behavior (SIB) among adolescents. The lifetime prevalence of SIB is between 16 and 22% in community sample with females more likely to engage in SIB. There are conflicting results about the global distribution of the prevalence of SIB and whether the SIB has increased in the 21st century. Our aim in the current study was to conduct a systematic search of and meta-analysis on the prevalence of SIB in adolescents over the past 5 years’ worth of published papers and to examine gender, continental, and year differences. We conducted a systematic search in June 2020 of six databases (PubMed, Scopus, Web of Science, OVID Medline, PsycINFO, EBSCO) with three main search terms: “self-injurious behavior,” “prevalence,” and “adolescence.” Article inclusion criteria were (a) written in English; (b) published between January 1, 2015, and June 18, 2020; and (c) focused on a community sample. Titles and abstracts of the articles were screened first. Then, the relevant full texts were read, and those that met the inclusion criteria were collected. We used Comprehensive Meta-Analysis software was used to conduct the analyses. After the screening process 97, articles were included in the meta-analysis. The age of the samples ranged from 11.00 to 18.53 years. The overall average prevalence of nonsuicidal self-injury in the studies was 16%. There was a significant gender difference: females reported a higher prevalence than males (19.4% and 12.9%, respectively). A significantly higher prevalence was found among Asian articles than those from other continents (19.5% and 14.7%, respectively). The prevalence of SIB did not change significantly between 2013 and 2018. The current research draws attention to the high prevalence of SIB among adolescents, especially among females and those living in Asia. It is important to address this behavior, both in terms of prevention and intervention.
Similar content being viewed by others
Background
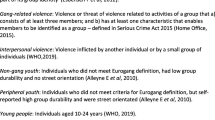
Self-injurious behavior (SIB) is a phenomenon whereby a person directly and deliberately damage themselves [1]. Various terms are used in the literature, such as, nonsuicidal self-injury (NSSI), deliberate self-harm (DSH), self-cutting, and self-harm [2,3,4,5,6]. SIB can be considered as a class of behaviors on a spectrum from NSSI—in which the person has no intent to die—to suicidal attempt (SA), which is a form of suicidal behavior [1]. Although NSSI and SA are two distinct behaviors, it is not always easy to decide whether there was a suicidal intent behind SIB, and in this case, it is difficult to separate them [1, 3]. Moreover, the comorbidity between NSSI and suicidal behaviors is approximately 50% in traditional and 70% in clinical populations [1, 7, 8]. Previous research has indicated that the higher risk of SA is associated with the following in regard to NSSI: greater frequency, more methods, and longer duration [1].
Several meta-analyses conducted in the past 20 years have focused on the prevalence of SIB [6, 9,10,11,12]; see Table 1).
Based on the previous meta-analyses, the prevalence of SIB shows a significant increase in the 1990s, but then a stagnation from 2005 [9, 10]. Gillies et al. (2018) found that the lifetime prevalence increased over time from 1990 to 2015, and Muehlenkamp et al. (2012) found no significant difference in the prevalence of NSSI and DSH between 2005 and 2011 [6, 10]. According to previous meta-analyses, between 1990 and 2015, the average lifetime prevalence of SIB among adolescents is between 16.9 and 19.7% [6, 9,10,11,12].
There are conflicting results about the gender differences in the prevalence of SIB [6, 9,10,11,12]. Some research has indicated that females have a lifetime prevalence of SIB that is two to three times higher than males [11], whereas other studies have found that the gender difference does not appear at all or, if it does, to a lesser extent [9, 10].
As shown in Table 1 the results are conflicting in regard to whether there is a difference in the prevalence of NSSI and DSH [6, 10, 12]. Muehlenkamp et al. (2012) did not find any significant difference between the two phenomena, however Gillies et al. (2018) and Lim et al. (2019) found a significantly higher prevalence of NSSI than DSH [6, 10, 12]. The lowest lifetime prevalence of NSSI was 18%, while the highest was 22.9% [6, 9,10,11,12]. At the same time, the lowest lifetime prevalence of DSH was 11.4%, while the highest was 16.1% [6, 9,10,11,12]. As mentioned above, unlike NSSI, DSH can be suicidal and nonsuicidal as well, but it must be a non-fatal self-harm [6, 12].
There are also conflicting results about the continental differences in the prevalence of SIB. While Swannell et al. (2014) didn’t find any significant continental differences in the prevalence of SIB, Gillies et al. (2018) did: Sweden had the highest, Norway had the lowest prevalence of self-harm in the meta-analysis [6, 9]. Lim et al. found that the lifetime prevalence of both NSSI and DSH were higher in non-Western countries than Western countries [12].
The above described previous meta-analyses highlight that these conflicting results can be due to the large differences among the included studies in methodological factors (e.g., sampling method, measurement, mean age of the sample), in the definitions of SIB (e.g., with or without suicidal intent), or in the place of data collection [6, 9,10,11,12].
Aims
Because of the heretofore conflicting results, our aim in this study was to follow up previous meta-analyses on the prevalence of SIB in adolescent community samples [6, 11]. We focused on data published between 2015 and 2020.
Our first hypothesis was that the prevalence of SIB did not change over time between the examined period (2015 and 2020) for both females and males. Our second hypothesis was that females reported a higher prevalence of a history of SIB than males.
Before addressing these hypotheses, we investigated the following questions: (a) What kinds of definitions of SIB are used? (b) What kinds of assessments are used to measure SIB? (c) What was the sampling method? (d) Where were the data of the included studies collected? (e) What was the mean age of the sample? (f) Was suicidal intent excluded from the definition of SIB?
Method
Literature search
We conducted a systematic literature search on June 18, 2020. We used six computerized literature databases: PubMed, Scopus, Web of Science, OVID Medline, PsycINFO, and EBSCO Discovery Service for Semmelweis University. Search terms were the following: “non-suicidal” OR nonsuicidal OR “self-injur*” OR “self-harm” OR “self harm” OR parasuic* OR “self-mutilation” AND prevalence AND adolescen* NOT “clinical trial” OR “case report” OR review. Two filters were added: (a) date between January 1, 2015, and June 18, 2020, and (b) English language. We used EndNote X9 software to remove duplicates and screen the 374 search hits.
Inclusion and exclusion criteria
To be included, studies had to report on the prevalence of SIB in adolescence in a community sample in a published article written in English. We used “adolescen*” among our search terms, and we included studies with an age range 11–18 years. However, in some articles this age range was wider (22 years being the oldest), so from these we included in the final analysis only those studies where the mean age of the sample was adolescence. For details, see Table 2.
When multiple studies reported on the same database, we included the ones with the largest sample size [13], the ones that provided data separately for males and females [14], and the ones that provided follow-up results [15, 16]. This led to the exclusion of six studies [17,18,19,20,21,22]. In addition, we contacted by email the authors of articles from which prevalence data could not be extracted. In case we did not receive sufficient statistics, we excluded the study (e.g., Carvalho et al., 2015). The methodology of this review follows the PRISMA guidelines [23].
Data extraction
Two authors (BFF, NK) coded the following information:
-
(1)
bibliographic information: authors, year of publication and data collection;
-
(2)
sample information: age range and mean age of sample, gender ratio, country, and continent the sample was recruited in, representativeness of the community sample, design;
-
(3)
measurement of SIB: measurement instrument, suicidal intent, terminology;
-
(4)
information for effect size: prevalence estimate and sample size.
Interrater reliability ranged from 73 and 100%. In case a consensus could not be reached between the two coders, the other two authors were consulted (ZKT, JB).
To test our hypotheses, we preferred to include the prevalence estimates separately for males and females if a study reported on those. For longitudinal studies, prevalence at all measurement points was coded; however, they were averaged to calculate an effect size for a study before we included the data in any analyses. We made an exception when prevalence estimates were available separately for males and females at one time point but not at another. In those cases, we chose to include only the estimates at the time point when they were reported separately for males and females.
During the coding, we had to impute some scores that were not reported in the primary studies. For studies that reported only the age range, we imputed the mean age as the geometric mean of the range. For studies that did not report the year of data collection, we subtracted 2 years from the year of publication (for a similar procedure, see Protzko et al., 2020) [24].
Statistical analyses
We used the Comprehensive Meta-Analysis software to conduct the analyses [25, 26]. We applied a random effects model. When a study reported results at more than one time point, we entered all in the software, which takes the average between multiple time points before entering a study in the grand average. We made an exception when conducting meta-regression analyses regarding the year of data collection and the mean age of the sample. In these cases, we only selected the first time point from these longitudinal studies to be included. In contrast, we considered estimates for males and females when reported separately in a study as independent effect sizes in all the analyses. Outliers were inspected based on a standardized residual exceeding ±3.29. We inspected the results according to several moderator variables. When inspecting results according to the different continents and suicidal intent, we conducted a subgroup analysis to statistically contrast them. We only included subgroups with at least four effect sizes in this analysis (for a similar procedure see Takacs and Kassai 2019) [27].
Results
Included studies
In sum, a total of 97 articles were included in this meta-analysis; we identified 178 effect sizes (see Figs 1, 2 and Table 2).
There were six outlying effect sizes that we excluded. Altogether, we had data from 439,818 participants. The overall average SIB prevalence in the studies was 16.0% (95% confidence interval [CI] [14.7, 17.4], k = 172). This was a heterogeneous effect, Q(171) = 30,136.96, p < 0.001, I2 = 99.43 τ2 = 0.44.
In our assessment of publication bias, Egger’s test showed significant asymmetry (intercept = −2.88, p = 0.046), but the funnel plot showed a symmetric distribution based on visual inspection, which was confirmed by no imputed studies in the Duval and Tweedie’s trim-and-fill procedure.
Among the 97 included articles, 74 reported prevalence data for females and males separately. There were 79 effect sizes reported for females. Two effect sizes were outliers and thus were excluded. We found an average prevalence of 19.4% for females, 95% CI [17.5, 21.4], k = 77. This effect was heterogeneous, Q(76) = 8,660.74, p < 0.001, I2 = 99.12 τ2 = 0.29. There were 75 effect sizes reported for males. One outlying effect size was excluded. We found an average prevalence of 12.9%, 95% CI [11.3, 14.8], k = 74. Again, this was a heterogeneous effect, Q(74) = 10,315.75, p < 0.001, I2 = 99.2 τ2 = 0.43.
Terms and definitions of SIB in the included studies
The terminology of SIB was not uniform across the included studies. All the studies defined SIB as a deliberate damage to oneself, but not all of them defined it as a nonsuicidal intent. Seventy-two articles (73.5%) made a clear distinction between suicidal and nonsuicidal intent.
There were 11 different terms for SIB in the included 97 papers. The most frequently used term was NSSI; this expression appeared in 60 articles (see Table 3).
Measurements of SIB in the included studies
Among the included studies we found diagnostic interviews, self-reported questionnaires, and single-item questions to measure SIB. Two studies measured NSSI based on DSM-5 criteria [122]. The most frequently used questionnaire was the Deliberate Self-Harm Inventory [123], which was mentioned in 13 articles. The Inventory of Statements About Self-Injury [124] was used in five studies, and the Functional Assessment of Self-Mutilation [125] also was used in five. Effect sizes based on a single item to assess SIB found an average prevalence of 11.6%, 95% CI [9.3, 14.5], k = 31. We found of 14.8%, 95% CI [12.8, 17.2], k = 60, in studies that used nonvalidated questionnaires. Questionnaires that had been validated for other constructs showed an average prevalence of 14.7%, 95% CI [9.8, 21.5], k = 6. Finally, questionnaires that had been validated for SIB showed the highest average percentage: 18.9%, 95% CI [16.9, 21.1], k = 77. For results separately for males and females, see the Supplementary Materials. Only one study used a diagnostic interview and reported on two effect sizes. The average of these showed a similar estimate as the grand average (14.2% (95% CI [7.7, 24.8], k = 2), more specifically, 18.7% for females and 10.2% for males).
Sampling
Of the 172 effect sizes, 99 were based on convenience sampling. These showed an average prevalence of 15.2%, 95% CI [13.4, 17.2]. Eighteen effect sizes were based on samples that applied randomization, showing a prevalence of 24.7%, 95% CI [18.9, 31.6]. For 55 sample sizes, the sample was representative of the population. Representative samples showed a pooled prevalence of 15.1%, 95% CI [13.2, 17.4]. A similar pattern was noted for females and males (see the Supplementary Materials).
Place of data collection of the included studies
From the 98 included articles, we found three collaborations in which data were collected in multiple countries; for the rest, the data were collected in single countries. When we inspected the results over all the effect sizes, we noted differences according to the continent on which the data had been collected. There were three effect sizes in two publications from South America that showed an average prevalence of 33%, 95% CI [13.7, 60.3], and we found two effect sizes in one publication from Africa that showed an average prevalence of 24.4%, 95% CI [19.1, 30.7], and data for two effect sizes published in the same article were collected in North America and Australia and Oceania as part of an international cooperation that showed a prevalence of 2.6%, 95% CI [1.3, 4.9]. These categories were excluded from the subgroup analysis as they contained less than 4 effect sizes. After we excluded these, we noted a significant difference between the prevalence estimates from the different continents (see Table 4), Q(3) = 10.97, p = 0.012. More specifically, prevalence estimates from Asia (19.5%, 95% CI [17.1, 22.2], k = 51) were significantly larger than those from the other three continents (14.6%, 95% CI [13.1, 16.2], k = 114), Q(1) = 11.20, p = 0.001. As shown in Table 4, the effect of continent was similar when we inspected effect sizes for female and male samples separately.
Mean age of the included samples
For assessing the effects of the mean age of the samples, we chose to focus on the first measurement point in the 17 longitudinal studies. In this analysis, seven outliers appeared that were then excluded. For an additional six effect sizes we could not extract the sample’s age, and thus those were also excluded from this analysis. This resulted in 165 effect sizes. The mean age of the sample ranged from 11.00 to 18.53 years. The mean age of the sample did not have a significant effect on the effect size (coefficient = 0.067, p = 0.12). For results separately for males and females, see the Supplementary Materials.
To make sure that longitudinal studies from which we chose to include the first estimate in this analysis did not influence the results by possibly reporting on substantially younger samples, we also ran the regression model on the cross-sectional studies only as a sensitivity analysis. This resulted in 134 effect sizes to be included. Again, the mean age of the sample did not have a significant effect on these prevalence estimates (coefficient = 0.058, p = 0.24).
Suicidal intent
For 125 effect sizes, suicidal intent was excluded. Those showed a pooled estimate of 18.3%, 95% CI [16.7, 19.9]. This was significantly higher than what was found in studies that did not exclude suicidal intent (11.3%, 95% CI [9.3, 13.7], k = 47), Q(1) = 20.52, p < 0.001. This pattern was also confirmed in only-female and only-male samples. For results separately for males and females, see the Supplementary Materials.
Prevalence of SIB
We found 92 effect sizes reporting on lifetime prevalence of SIB, 72 effect sizes that estimated 1-year prevalence, and 17 that estimated 6-month prevalence. An average of 17.9%, 95% CI [16.3, 19.5], was found overall when lifetime prevalence was assessed. This estimate was 22.9 (95% CI [20.9, 25.0], k = 42) for females and 13.7% (95% CI [11.2, 16.8], k = 39) for males.
An overall average prevalence of 13.4%, 95% CI [11.5, 15.6] was found when assessing prevalence in the last year. This estimate was 15.9% (95% CI [12.9, 19.4], k = 32) for females and 10.7% (95% CI [8.7, 13.2], k = 32) for males. An overall prevalence of 16.2%, 95% CI [11.0, 23.3] was estimated when we considered only the last 6 months, 18% (95% CI [8.9, 33.2], k = 7) for females and 13.8% (95% CI [6.2, 27.9], k = 7) for males.
Year of data collection
In regard to assessing the effects of the year of data collection, we chose to focus on the first measurement point in the 17 longitudinal studies. In this analysis, seven outliers appeared that were then excluded. Data for the primary studies were collected between 1998 and 2018. The year of data collection had a significant, positive effect on the 171 effect sizes (coefficient = 0.035, p = 0.008); that is, more recent studies found larger prevalence. For results presented separately for females and males, see the Supplementary Materials.
For further investigation, we restricted the year of data collection to 2013 and onward so we could assess the effect in the time constraints that corresponds to the time constraints of year of publication of the present meta-analysis (2015 and onward). Data for 119 effect sizes were collected in or after 2013. When we considered only these studies, the effect of year of data collection was not significant on the effect sizes (coefficient = −0.015, p = 0.72). The same was found for the 53 effect sizes for females (coefficient = −0.005, p = 0.92) and for the 51 effect sizes for males (coefficient = −0.05, p = 0.49). Scatterplots are shown in the Supplementary Materials.
Risk of bias
Risk-of-bias criteria was based on the Cochrane Risk of Bias Tool [126], adapted for the studies (cohort, cross-sectional, and longitudinal).
Discussion
Because previous meta-analyses have yielded conflicting results on the prevalence of SIB in community adolescent samples [6, 11], we found it important to complete a follow-up meta-analyses with clear methodology on recently published data. In the present meta-analysis, we found that the prevalence of SIB in adolescents was 16% in studies published between 2015 and 2020. This result is comparable to the estimate of 16.9% found in a previous meta-analysis [6]. Regarding methodological differences, as can be expected, a slightly higher estimate was found when considering lifetime prevalence (17.9%) as compared with the 1-year (13.4%) or 6-month prevalence (16.2%). We also noted a significantly higher prevalence when suicidal intent was excluded (18.3%) than when it was not excluded (11.3%), and the largest prevalence was found when measurement instruments were used that had been validated for self-injurious behaviors (18.8%). In addition, methodologically more rigorous studies that focused on representative samples found an average SIB prevalence of 15.1%. This is an interesting issue, while self-harm without suicidal intent should be a subgroup of self-harm covering forms both with and without suicidal intent. Hence the first number should always be lower than the second number. A possible explanation could be that the studies used the same term but actually employ different criteria. In addition, differences in the prevalence of NSSI and DSH may also result from measurement differences between the two types of SIB. Previous meta-analyses have reported higher prevalence rates for multi-item instruments [6, 10], and 65.5% of NSSI measurements consisted of multiple items, compared to 60% of DSH measurements consisting of a single item. In a meta-analysis made by Swannell et al. (2014), checklist versus single-item measurement explained the 41% of variance between studies [9]. Our review shows that, among adolescents, there are no significant changes in the prevalence between ages 11.0 and 18.5 years. This result is comparable to Lim’s meta-analysis [12] but does not align with Gillies and colleagues’ (2018) study. We found similar prevalence estimates among studies that used convenience and representative samples. However, and surprisingly, studies that used a random sample found larger estimates. This is puzzling and needs further research.
Our first hypothesis was only partially confirmed. When we considered all data that were published between 2015 and 2018, we found that there was a significant increase between 1998 and 2018 in the prevalence of SIB. However, when we restricted our analysis to the time frame between 2013 and 2018 (to reflect the publication time window of 2015 and 2018), we found no change in prevalence, as we had expected. Previous meta-analyses have found mixed results regarding this question. Muehlenkamp and colleagues (2012) did not find any significant difference in the prevalence of SIB between 2008 and 2015, whereas Gillies and colleagues (2018) found an increase between 1990 and 2018. Our results are in line with both previous findings in that they show an increase before 2013, but no change since then. This finding can be important to both decision makers and professionals for the appropriate planning of prevention programs.
Our second hypothesis was confirmed; we found a substantial difference between the estimates for females (19.4%) and males (12.9%), with nonoverlapping confidence intervals. A similar pattern was observed when we considered only lifetime prevalence, with 22.9% for females and 13.7% for males. These results are comparable to Bresin and Schoenleber’s (2015) meta-analysis, in which the prevalence was significantly higher among females. Studies that excluded suicidal intent found an average of 21% for females and 16.5% for males. Similarly, estimates based on measurement instruments that were validated for SIB showed 21.9% for females and 15.7% for males. On the other hand, studies with representative samples showed slightly lower estimates: 18.2% for females and 10.9% for males. Thus, the patterns were very similar for females and males when the effect of methodological differences in the primary studies were assessed. However, the cultural difference between countries in Asia and those on other continents was more articulated for males (Asia = 19.5% vs. other = 10.8%) than for females (Asia = 22.3% vs. other = 18.5%). Nock and Prinstein (2005) found that NSSI often is connected to psychological distress [127], and adolescent girls usually have more psychological distress than men [128]. These results highlight that it is necessary to pay more careful attention to NSSI by female adolescents and that perhaps further attention should be given to Asian male populations.
We found some differences in the prevalence estimate as a function of methodological differences among the primary studies; however, we should note that moderators might be confounded.
The pooled estimate from Asian countries (19.5%) was significantly higher than that from other continents (14.6%). Again, this confirms earlier meta-analytic results estimating a relatively large prevalence in Asian countries (Lim et al. 2019). This difference was even more articulated for males. So, it may be that the differences in SIB between Asian and non-Asian countries are somehow connected to gender. To understand this result, further research should focus on the transcultural aspects of SIB.
We did not find a difference between NSSI (18.7%) and DSH (15.1%), unlike Gillies’s results [6], but we found a substantial difference between NSSI (18.7%) and self-harm (12.7%). In contrast to females, we found a substantial difference between NSSI (17.1%) and DSH (6.3%), and between NSSI (17.1%) and self-harm (9%) among males.
Our review highlights that the highest prevalence rates were found when SIB was measured with a validated questionnaire as compared with studies that used single-item or nonvalidated questionnaires, a pattern that was also confirmed separately for male and female samples. This result is likely due to the fact that validated questionnaires are more sensitive than single-item measures [6, 10].
Our results are limited by the heterogeneity of the primary studies, that is, in regard to the sample and the measurement instruments and the conceptualization of SIBs. The findings of the present meta-analysis confirm that these differences among the primary studies have an important effect on the prevalence estimates. There is currently no consensus in the literature about the conceptualization of SIB [6, 10], which makes our work more difficult when evaluating the data. However, to provide the most precise estimate, we pooled the studies that used representative samples that reported on lifetime prevalence of SIBs excluding suicidal intent measured by a validated measurement instrument and found similar estimates. In addition, we did this to avoid a confound effect of these moderators. Moreover, although overall we found a relatively large number of studies that reported on prevalence of SIBs, it is questionable whether nonsignificant results in subgroup and meta-regression analyses are truly due to an absence of an effect or whether they are instead due to a lack of statistical power.
To our best knowledge, this is the most recent meta-analysis on the prevalence of SIB among adolescents. An overall prevalence of 16% was found, which means that one in six adolescents has a history of self-harm. Moreover, a larger estimate was found for females as compared with males: every fifth adolescent girl reported having conducted self-harm. It is interesting that estimates were largest in Asian countries with males, approaching a 20% prevalence. Further research should focus on the transcultural aspects of self-harm to understand this difference. All these results have public health importance in drawing the attention of clinicians and decision makers to adolescents who engage in SIB. Clinicians need to be aware of the high prevalence and risk factors (e.g., female gender, Asian populations) of SIB in adolescence. Prevention and intervention are very important in this age group.
Data availability
Not applicable.
Abbreviations
- DSH:
-
Deliberate self-harm
- D-SIB:
-
Deliberate self-injurious behavior
- DSM-5:
-
Diagnostic and statistical manual of mental disorders 5th edition
- NSSI:
-
Nonsuicidal self-injury
- SH:
-
Self-harm
- SHB:
-
Self-harm behavior
- SIB:
-
Self-injurious behavior
- SITB:
-
Self-injurious thoughts and behavior
References
Nock M et al (2006) Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res 144:65–72
Klonsky ED, Oltmanns TF, Turkheimer E (2003) Deliberate self-harm in a nonclinical population: prevalence and psychological correlates. Am J Psychiatry 160(8):1501–1508
Klonsky ED (2007) The functions of deliberate self-injury: a review of the evidence. Clin Psychol Rev 27(2):226–239
Nock M (2010) Self-injury. Annu Rev Clin Psychol 6(1):339–363
Whitlock J, Eckenrode J, Silverman D (2006) Self-injurious behaviors in a college population. Pediatrics 117(6):1939–1948
Gillies D et al (2018) Prevalence and characteristics of self-harm in adolescents: meta-analyses of community-based studies 1990–2015. J Am Acad Child Adolesc Psychiatry 57(10):733–741
Muehlenkamp JJ, Gutierrez PM (2007) Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Arch Suicide Res 11(1):69–82
Klonsky ED, Muehlenkamp JJ (2007) Self-injury: a research review for the practitioner. J Clin Psychol 63(11):1045–1056
Swannell S et al (2014) Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav 44: 273–303
Muehlenkamp JJ et al (2012) International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health 6(1):10
Bresin K, Schoenleber M (2015) Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev 38:55–64
Lim KS et al (2019) Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health 16(22): 4581
Victor SE et al (2019) Parent and peer relationships as longitudinal predictors of adolescent non-suicidal self-injury onset. Child Adolesc Psychiatry Ment Health 13:1
Gandhi A et al (2017) Age of onset of non-suicidal self-injury in Dutch-speaking adolescents and emerging adults: an event history analysis of pooled data. Compr Psychiatry 80:170–178
Huang YH et al (2017) Relationship between predictors of incident deliberate self-harm and suicide attempts among adolescents. J Adolesc Health 60(5):612–618
Doyle L (2015) Self-harm in young people: prevalence, associated factors and help-seeking in school-going adolescents. Int J Ment Health Nurs 24: 485–494
Gandhi A et al (2016) Non-suicidal self-injury and adolescents attachment with peers and mother: the mediating role of identity synthesis and confusion. J Child Fam Stud 25(6):1735–1745
Gandhi A et al (2016) Sociotropy, autonomy, and non-suicidal self-injury: the mediating role of identity confusion. Personality Individ Differ 99:272–277
Gandhi A et al (2016) Reactive and regulative temperament and non-suicidal self-injury in Flemish adolescents: the intervening role of identity formation. Personality Individ Differ 99:254–259
Doyle L, Sheridan A, Treacy MP (2017) Motivations for adolescent self-harm and the implications for mental health nurses. J Psychiatr Ment Health Nurs 24(2–3):134–142
Huang YH et al (2017) Correlation of impulsivity with self-harm and suicidal attempt: a community study of adolescents in Taiwan. BMJ Open 7(12): e017949
Scott LN et al (2015) Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: a multi-wave prospective study. Compr Psychiatry 58:1–10
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Protzko J (2020) Kids these days! Increasing delay of gratification ability over the past 50 years in children. Intelligence 80:101451
Borenstein M, Larry H, Higgins J, Rothstein H (2015) Manual to the comprehensive meta-analysis version 3 software. Biostat, Englewood, NJ
Borenstein M, Larry H, Higgins J, Rothstein H (2014) Comprehensive meta-analysis version 3. Biostat, Englewood, NJ
Takacs ZK, Kassai R (2019) The efficacy of different interventions to foster children’s executive function skills: a series of meta-analyses. Psychol Bull 145(7):653–697
Aldrich JT, Wielgus MD, Mezulis AH (2018) Low physiological arousal and high impulsivity as predictors of self-injurious thoughts and behaviors among adolescents. J Adolesc 62:55–60
Badoud D et al (2015) The French version of the reflective functioning questionnaire: validity data for adolescents and adults and its association with non-suicidal self-injury. PLoS ONE 10(12): e0145892
Baetens I et al (2015) The relationship between parental expressed emotions and non-suicidal self-injury: the mediating roles of self-criticism and depression. J Child Fam Stud 24(2):491–498
Barrocas AL et al (2015) Nonsuicidal self-injury in adolescence: longitudinal course, trajectories, and intrapersonal predictors. J Abnorm Child Psychol 43(2):369–380
Bhola P et al (2017) Predictors of non-suicidal and suicidal self-injurious behaviours, among adolescents and young adults in urban India. Asian J Psychiatr 29:123–128
Brausch AM, Woods SE (2019) Emotion regulation deficits and nonsuicidal self-injury prospectively predict suicide ideation in adolescents. Suicide Life Threat Behav 49(3):868–880
Buelens T et al (2020) Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J Affect Disord 260:314–322
Calvete E et al (2015) Prevalence and functions of non-suicidal self-injury in Spanish adolescents. Psicothema 27(3):223–228
Carvalho BC et al (2017) Biting myself so I don’t bite the dust: prevalence and predictors of deliberate self-harm and suicide ideation in Azorean youths. Braz J Psychiatry 39(3): 252–262
Cassels M et al (2018) Poor family functioning mediates the link between childhood adversity and adolescent nonsuicidal self-injury. J Child Psychol Psychiatry 59(8):881–887
Castro K, Kirchner T (2018) Coping and psychopathological profile in nonsuicidal self-injurious chilean adolescents. J Clin Psychol 74(1):147–160
Chen WL, Chun CC (2019) Association between emotion dysregulation and distinct groups of non-suicidal self-injury in Taiwanese female adolescents. Int J Environ Res Public Health 16(18): 3361
Cimen ID, Coskun A, Etiler N (2017) Non-suicidal self-injury behaviors’ features and relationship with adolescents’ daily life activities and mental status. Turk J Pediatr 59(2):113–121
Claes L et al (2015) Bullying and victimization, depressive mood, and non-suicidal self-injury in adolescents: the moderating role of parental support. J Child Fam Stud 24(11):3363–3371
Copeland M et al (2019) Social ties cut both ways: self-harm and adolescent peer networks. J Youth Adolesc 48(8):1506–1518
Donath C et al (2019) Epidemiology of suicidal ideation, suicide attempts, and direct self-injurious behavior in adolescents with a migration background: a representative study. BMC Pediatr 19(1):45
Duarte E, Gouveia-Pereira M, Gomes HS (2019) Development and factorial validation of the inventory of deliberate self-harm behaviours for portuguese adolescents. Psychiatr Q 90(4):761–776
Emerson E et al (2019) Emotional difficulties and self-harm among British adolescents with and without disabilities: cross sectional study. Disabil Health J 12(4):581–587
Emery AA, Heath NL, Rogers M (2017) Parents’ role in early adolescent self-injury: an application of self-determination theory. Sch Psychol Q 32(2):199–211
Endo K et al (2017) Preference for solitude, social isolation, suicidal ideation, and self-harm in adolescents. J Adolesc Health 61(2):187–191
Esposito C, Bacchini D, Affuso G (2019) Adolescent non-suicidal self-injury and its relationships with school bullying and peer rejection. Psychiatry Res 274:1–6
Farhat LC et al (2020) Self-injurious behavior and gambling-related attitudes, perceptions and behaviors in adolescents. J Psychiatr Res 124:77–84
Fraser G et al (2018) Non-suicidal self-injury, sexuality concerns, and emotion regulation among sexually diverse adolescents: a multiple mediation analysis. Arch Suicide Res 22(3):432–452
Gandhi A et al (2015) Non-suicidal self-injury and identity distress in Flemish adolescents: exploring gender differences and mediational pathways. Personality Individ Differ 82:215–220
Gandhi A et al (2017) Directionality of effects between non-suicidal self-injury and identity formation: a prospective study in adolescents. Personality Individ Differ 109:124–129
Gandhi A et al (2018) Age of onset of non-suicidal self-injury in Dutch-speaking adolescents and emerging adults: an event history analysis of pooled data. Compr Psychiatry 80:170–178
Gandhi A et al (2018) Association between non-suicidal self-injury, parents and peers related loneliness, and attitude towards aloneness in Flemish adolescents: an empirical note. Psychologica Belgica 58(1):3–12
Gandhi A et al (2019) Maternal and peer attachment, identity formation, and non-suicidal self-injury: a longitudinal mediation study. Child Adolesc Psychiatry Ment Health 13: 7
Garisch J, Wilson M (2015) Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: cross-sectional and longitudinal survey data. Child Adolesc Psychiatry Mental Health 9: 28
Gaspar S et al (2019) Non-suicidal self-injuries and adolescents high risk behaviours: highlights from the Portuguese HBSC study. Child Indic Res 12(6):2137–2149
Geulayov G et al (2018) Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study. Lancet Psychiatry 5(2):167–174
Gromatsky MA et al (2017) The role of parental psychopathology and personality in adolescent non-suicidal self-injury. J Psychiatr Res 85:15–23
Guerreiro DF et al (2017) Self-harm in adolescents: a self-report survey in schools from Lisbon. Portugal Arch Suicide Res 21(1):83–99
Hamada S et al (2018) Association between bullying behavior, perceived school safety, and self-cutting: a Japanese population-based school survey. Child Adolesc Mental Health 23(3):141–147
Han A et al (2018) A self-harm series and its relationship with childhood adversity among adolescents in mainland China: a cross-sectional study. BMC Psychiatry 18(1):28
Hanania JW et al (2015) Non-suicidal self-injury among adolescents in Amman. Jordan Arch Suicide Res 19(2):260–274
Heerde JA et al (2015) Incidence and course of adolescent deliberate self-harm in Victoria, Australia, and Washington state. J Adolesc Health 57(5):537–544
Horváth LO et al (2018) Direct self-injurious behavior (D-SIB) and life events among vocational school and high school students. Int J Environ Res Public Health 15(6): 1068
Horvath LO et al (2020) Nonsuicidal self-injury and suicide: the role of life events in clinical and non-clinical populations of adolescents. Front Psychiatry 11
Jantzer V et al (2015) Does parental monitoring moderate the relationship between bullying and adolescent nonsuicidal self-injury and suicidal behavior? A community-based self-report study of adolescents in Germany. BMC Public Health 15
Jiang YQ et al (2016) Buffering the effects of peer victimization on adolescent non-suicidal self-injury: the role of self-compassion and family cohesion. J Adolesc 53:107–115
Kadziela-Olech H et al (2015) The prevalence of non-suicidal self-injury (NSSI) among high school students in relation to age and sex. Psychiatr Pol 49(4):765–778
Kaess M et al (2020) Life events predicting the first onset of adolescent direct self-injurious behavior—a prospective multicenter study. J Adolesc Health 66(2):195–201
Kang N et al (2018) Distress intolerance mediates the relationship between child maltreatment and nonsuicidal self-injury among chinese adolescents: a three-wave longitudinal study. J Youth Adolesc 47: 2220
Kelada L, Hasking P, Melvin G (2016) The relationship between nonsuicidal self-injury and family functioning: adolescent and parent perspectives. J Marital Fam Ther 42(3):536–549
Kiekens G et al (2015) Non-suicidal self-injury among Dutch and Belgian adolescents: personality, stress and coping. Eur Psychiatry 30(6):743–749
Kitagawa Y et al (2017) Appetite loss as a potential predictor of suicidal ideation and self-harm in adolescents: a school-based study. Appetite 111:7–11
Klemera E et al (2017) Self-harm in adolescence: protective health assets in the family, school and community. Int J Public Health 62(6):631–638
Koenig J et al (2016) Prospective risk for suicidal thoughts and behaviour in adolescents with onset, maintenance or cessation of direct self-injurious behaviour. Eur Child Adolesc Psychiatry 26(3):345–354
Latina D, Stattin H (2017) Adolescents who self-harm: the patterns in their interpersonal and psychosocial difficulties. J Res Adolesc 28(4):824–838
Law BF, Shek DTL (2016) A 6-year longitudinal study of self-harm and suicidal behaviors among Chinese adolescents in Hong Kong. J Pediatr Adolesc Gynecol 29(1):S38–S48
Lee WK (2016) Psychological characteristics of self-harming behavior in Korean adolescents. Asian J Psychiatr 23:119–124
Li D et al (2019) Interaction of health literacy and problematic mobile phone use and their impact on non-suicidal self-injury among Chinese adolescents. Int J Environ Res Public Health 16(13): 2366
Lin M-P et al (2017) Prevalence of nonsuicidal self-injury and its risk and protective factors among adolescents in Taiwan. Psychiatry Res 255:119–127
Liu HC et al (2017) Self-harm and its association with internet addiction and internet exposure to suicidal thought in adolescents. J Formos Med Assoc 116(3):153–160
Liu X (2018) Understanding the mental distress that leads to NSSI among Chinese adolescents in Hong Kong: a three-wave longitudinal study. 2018: Dissertation abstracts international: section B: the sciences and engineering, vol 79(8-B(E))
Luyckx K et al (2015) Non-suicidal self-injury in female adolescents and psychiatric patients: a replication and extension of the role of identity formation. Personality Individ Differ 77:91–96
Lüdtke J et al (2017) The influence of personality traits and emotional and behavioral problems on repetitive nonsuicidal self-injury in a school sample. Compr Psychiatry 74:214–223
Madjar N et al (2019) Exploring particular facets of cognitive emotion regulation and their relationships with nonsuicidal self-injury among adolescents. Crisis J Crisis Intervent Suicide Prevent 40(4):280–286
Mars B et al (2019) Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry 6(4):327–337
Martinez-Ferrer B, Stattin H (2019) Self-harm, depressive mood, and belonging to a subculture in adolescence. J Adolesc 76:12–19
McManus S, Gunnell D (2020) Trends in mental health, non-suicidal self-harm and suicide attempts in 16–24-year old students and non-students in England, 2000–2014. Soc Psychiatry Psychiatr Epidemiol 55(1):125–128
Monto MA, McRee N, Deryck FS (2018) Nonsuicidal self-injury among a representative sample of US adolescents, 2015. Am J Public Health 108(8):1042–1048
Morey Y et al (2017) Adolescent self-harm in the community: an update on prevalence using a self-report survey of adolescents aged 13–18 in England. J Public Health 39(1):58–64
Nguyen HTL et al (2020) Relationships among cyberbullying, parental attitudes, self-harm and suicidal behavior among adolescents: results from a school-based survey in Vietnam. BMC Public Health 20(1)
Oktan V (2017) Self-harm behaviour in adolescents: body image and self-esteem. J Psychol Couns Sch 27(2):177–189
Pawłowska B et al (2015) Prevalence of self-injury, suicidal ideation, plans and attempts in adolescents aged 13 to 19 years of age. Polish J Public Health 125(1):55–59
Pawłowska B et al (2016) Prevalence of self-injury performed by adolescents aged 16–19 years. Psychiatr Pol 50(1):29–42
Peng Z et al (2019) Associations between Chinese adolescents subjected to traditional and cyber bullying and suicidal ideation, self-harm and suicide attempts. BMC Psychiatry 19(1):324
Pisinger VSC, Hawton K, Tolstrup JS (2019) School- and class-level variation in self-harm, suicide ideation and suicide attempts in Danish high schools. Scand J Public Health 47(2):146–156
Plener PL et al (2015) Immigration as risk factor for non-suicidal self-injury and suicide attempts in adolescents in Germany. Child Adolesc Psychiatry Mental Health 9
Plener PL et al (2016) The prevalence of nonsuicidal self-injury (NSSI) in a representative sample of the German population. BMC Psychiatry 16(1):353
Quarshie ENB, Waterman MG, House AO (2020) Prevalence of self-harm among lesbian, gay, bisexual, and transgender adolescents: a comparison of personal and social adversity with a heterosexual sample in Ghana. BMC Res Notes 13(1):271
Reigstad B, Kvernmo S (2017) Concurrent adversities and deliberate self-harm among indigenous Sami and majority Norwegian adolescents: the Norwegian Arctic Adolescent Health Study. Scand J Child Adolesc Psychiatry Psychol 5(3):92–103
Ren YX et al (2018) The mediating role of coping strategy in the association between family functioning and nonsuicidal self-injury among Taiwanese adolescents. J Clin Psychol 74(7):1246–1257
Schwartz-Mette RA, Lawrence HR (2019) Peer socialization of non-suicidal self-injury in adolescents’ close friendships. J Abnorm Child Psychol 47(11):1851–1862
Sigurdson JF et al (2018) The longitudinal association of being bullied and gender with suicide ideations, self-harm, and suicide attempts from adolescence to young adulthood: a cohort study. Suicide Life Threat Behav 48(2):169–182
Simioni AR et al (2017) Prevalence, clinical correlates and maternal psychopathology of deliberate self-harm in children and early adolescents: results from a large community study
Solis-Bravo MA et al (2019) Are tattoos an indicator of severity of non-suicidal self-injury behavior in adolescents? Psychiatry Investig 16(7):504–512
Somer O et al (2015) Prevalence of non-suicidal self-injury and distinct groups of self-injurers in a community sample of adolescents. Soc Psychiatry Psychiatr Epidemiol 7:1163
Stanford S, Jones MP, Hudson JL (2017) Rethinking pathology in adolescent self-harm: towards a more complex understanding of risk factors. J Adolesc 54:32–41
Sutin AR et al (2018) Perceived body discrimination and intentional self-harm and suicidal behavior in adolescence. Child Obes 14(8):528–536
Tang J et al (2016) Stressful life events as a predictor for nonsuicidal self-injury in southern chinese adolescence: a cross-sectional study. Medicine (Baltimore) 95(9):e2637
Tang J et al (2018) Prevalence of and risk factors for non-suicidal self-injury in rural China: results from a nationwide survey in China. J Affect Disord 226:188–195
Tanner A, Hasking P, Martin G (2016) Co-occurring non-suicidal self-injury and firesetting among at-risk adolescents: experiences of negative life events, mental health problems, substance use, and suicidality. Arch Suicide Res 20(2):233–249
Tilton-Weaver L, Marshall SK, Svensson Y (2019) Depressive symptoms and non-suicidal self-injury during adolescence: latent patterns of short-term stability and change. J Adolesc 75:163–174
Tseng FY, Yang HJ (2015) Internet use and web communication networks, sources of social support, and forms of suicidal and nonsuicidal self-injury among adolescents: different patterns between genders. Suicide Life Threat Behav 45(2):178–191
Wan YH et al (2015) Longitudinal effects of psychological symptoms on non-suicidal self-injury: a difference between adolescents and young adults in China. Soc Psychiatry Psychiatr Epidemiol 50(2):237–247
Wan Y et al (2019) Associations of adverse childhood experiences and social support with self-injurious behaviour and suicidality in adolescents. Br J Psychiatry 214(3):146–152
Wan YH et al (2020) Associations of coping styles with nonsuicidal self-injury in adolescents: do they vary with gender and adverse childhood experiences? Child Abuse Neglect 104: 104470
Wang BY et al (2016) Developmental trajectories of nonsuicidal self-injury in adolescence and intrapersonal/interpersonal risk factors. J Res Adolesc 27(2):392–406
Zetterqvist M (2016) Nonsuicidal self-injury in adolescents: characterization of the disorder and the issue of distress and impairment. Suicide Life Threat Behav 47(3):321–335
Zhang SC et al (2016) Low health literacy and psychological symptoms potentially increase the risks of non-suicidal self-injury in Chinese middle school students. BMC Psychiatry 16(1):327
Zubrick SR et al (2015) Self-harm: prevalence estimates from the second Australian child and adolescent survey of mental health and wellbeing. Aust N Z J Psychiatry 50(9):911–921
American Psychiatric and Association (2013) Diagnostic and statistical manual of mental disorders, 5th ed. Diagnostic and statistical manual of mental disorders. American Psychiatric Association, Washington DC
Gratz KL (2001) Measurement of deliberate self-harm: preliminary data on the deliberate self-harm inventory. J Psychopathol Behav Assess 23(4):253–263
Klonsky ED, Glenn CR (2009) Assessing the functions of non-suicidal self-injury: psychometric properties of the inventory of statements about self-injury (ISAS). J Psychopathol Behav Assess 31(3):215–219
Lloyd EE, Kelley ML, Hope T (1997) Self-mutilation in a community sample of adolescents: descriptive characteristics and provisional prevalence rates. In: Poster presented at the annual meeting of the society for behavioral medicine. New Orleans, LA
Higgins JPT, Sally G (2011) Cochrane handbook for systematic reviews of interventions. Higgins JPT, Sally G (eds). The Cochrane Collaboration
Nock MK, Prinstein MJ (2005) Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol 114(1):140–146
Hawton K, Harriss L (2008) Deliberate self-harm by under-15-year-olds: characteristics, trends and outcome. J Child Psychol Psychiatry 49(4):441–448
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
BFF made the literature search, coded the articles, made the analyses, wrote the main manuscript text and prepared the figures. ZKT supervised and reviewed the statistical analysis of the manuscript. NK made the consensus coding of the articles and the risk of bias. JB participated in the design of the study, coordinated the steps, reviewed the manuscript and the figures. All authors read and approved the final manuscript. All authors contributed equally to this work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farkas, B.F., Takacs, Z.K., Kollárovics, N. et al. The prevalence of self-injury in adolescence: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry (2023). https://doi.org/10.1007/s00787-023-02264-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-023-02264-y