Abstract
Maternal Vitamin B12 deficiency during pregnancy is associated with offspring neuropsychiatric disorders. Few previous studies examining this association with attention-deficit/hyperactivity disorder (ADHD) report inconsistent findings. The study examines the association between maternal serum Vitamin B12 levels and offsprings’ risk of ADHD. This study is based on the Finnish Prenatal Study of ADHD with a nested case–control design. All the singleton children born in Finland between January 1998 and December 1999 and diagnosed with ADHD were included in the study. A total of 1026 cases were matched with an equal number of controls on sex, date of birth and place of birth. Maternal Vitamin B12 levels were assessed using a chemiluminescence microparticle immunoassay and archived from maternal serum banks, collected during the first and early second trimester of pregnancy. Lower maternal Vitamin B12 levels when analyzed as a continuous variable was not associated with offspring ADHD (aOR 0.97, 95% CI 0.79–1.18, p = 0.75). No significant associations were seen in the lowest quintile of Vitamin B12 levels (aOR 0.96, 95% CI 0.73–1.27, p = 0.80). This is the first study examining maternal sera Vitamin B12 levels during early pregnancy and offspring ADHD. The result suggests that Vitamin B12 deficiency during early pregnancy has specificity for some disorders but not with offspring ADHD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental disorder characterized by symptoms of hyperactivity, impulsivity, and inattention [1]. The estimated prevalence of ADHD is 3.4% in children [2]. Although there is strong evidence for genetic factors in ADHD [1], several environmental factors also contribute [3,4,5,6,7]. Evidence linking maternal nutrition and neuropsychiatric disorders in children has been shown in the Dutch and the Chinese famine studies in which maternal exposure to famine resulted in offspring schizophrenia [8,9,10,11,12] and depression [13, 14]. Maternal nutrition is critical for fetal growth and development [15], and prenatal nutritional deficiency during a critical phase of brain development may result in irreversible functional changes to the brain, predisposing children to neurodevelopmental disorders [16, 17]. Several nutrient deficiencies such as folate, polyunsaturated fatty acids and minerals like iron and iodine in early pregnancy have been reported to negatively impact cognitive and behavioural outcomes of offspring [18,19,20]. Maternal nutrient deficiency, including folic acid and iron deficits, has been suggested in several birth cohort studies as being related to offspring risk of schizophrenia [21].
Vitamin B12 (Cobalamin) is an essential nutrient required for neural myelination, synaptogenesis and neurotransmitter synthesis [22]. Vitamin B12 functions as an enzyme in the conversion of methylmalonic acid to succinyl-CoA and as a cofactor with folic acid in the methionine synthase reaction, which converts homocysteine into methionine [23]. Impaired Vitamin B12 status during pregnancy has been associated with birth defects [24, 25] and immune function impairment [26]. Folate supplementation has been effective in the prevention of neural tube defects [27, 28].
According to our systematic review on the association of offspring ADHD with maternal Vitamin B12 and folate, we found five relevant studies, summarized in Table 1. None of the studies have examined maternal sera Vitamin B12 and the risk for ADHD in offspring. The UK study including 139 pregnant mothers showed that the maternal red cell folate (RCF) concentration was associated with offspring ADHD symptoms [29]. The Danish register-based study including 35,059 pregnant mothers suggested that multivitamin but not folic acid supplementation before and during early pregnancy was associated with a lower risk of offspring hyperkinetic disorder diagnosis [30]. However, studies from New Zealand (n = 6246) [31] and from Spain (n = 420) [32] did not find associations between multivitamin or folic acid supplementation during pregnancy and offspring ADHD symptoms The Japanese questionnaire study including 1199 pregnant mothers’ past 1-month diet history found no association between maternal Vitamin B12 intake and parent-rated ADHD symptoms in offspring [33].
The previous studies with inconsistent findings have several limitations. First, no studies have measured Vitamin B12 levels using maternal sera samples and ADHD outcomes in the offspring. Information in previous studies on Vitamin B12 was based on multivitamin supplementation or food intake and the composition of the multivitamins used during pregnancy was not clear. Second, in four of the studies, ADHD symptoms were assessed by parents’ [29, 31, 33] or teachers’ [32] ratings and in only one study, the outcome was derived using register-based diagnoses of ADHD [30]. Third, the doses of supplements were unknown, thus limiting findings and conclusions drawn from these studies.
This is the first population-based study using maternal sera to analyze Vitamin B12 levels in early pregnancy and follow-up of the offsprings’ ADHD outcome. The aim of this study was to examine the association between maternal serum Vitamin B12 levels in early pregnancy and the risk of ADHD diagnosis in the offspring.
Methods
The study is based on the Finnish Prenatal Study of ADHD (FIPS-ADHD) derived from a nested case–control design. The study includes all singleton live births in Finland from 1998 to 1999 and diagnosed with ADHD in the Care Register for Health Care (CRHC) by 2011. Ethical approval for the study was provided by the Ethics Committee of the Hospital District of Southwest Finland, by the data protection authorities at the National Institute for Health and Welfare, and by the Institutional Review Board of the New York State Psychiatric Institute.
Nationwide registers
In this study, data were derived from three national registers: the CRHC, the Finnish Medical Birth Register (FMBR), and the Finnish Population Register Center (PRC). These registers are linked using personal identity codes (PIC).
The CRHC includes computerized data on all public and private inpatient diagnoses since 1967 and all outpatient diagnoses since 1998. The diagnostic classification in Finland is based on the International Classification of Diseases (ICD), which is the international standard for reporting diseases and health conditions maintained by the World Health Organization [34]. The ICD-10 has been used since 1996 [34], ICD-9 from 1987 to 1995 [35] and ICD-8 from 1969 to 1986 [36]. A previous diagnostic validation study of the ADHD diagnosis in the register, based on the ICD-criteria for hyperkinetic disorder, has shown 88% validity for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for ADHD [37]. The ICD-10 and DSM-IV criteria for hyperkinetic disorder/ADHD overlap, but the DSM-IV criteria have been shown to identify a broader group of children [38, 39].
The FMBR includes comprehensive and standardized data on all live births in Finland during the neonatal period up to 7 days of age, and stillbirths where the fetuses had reached at least 22 weeks of gestation or had a birth weight of at least 500 g. Data also include demographic characteristics, reproductive history, maternal health-related behaviors and perinatal events.
The PRC is a computerized national archive that contains basic demographic information on Finnish citizens and permanent residents in Finland. The personal data recorded in the system include name, PIC, address, citizenship and native language, family relations, date of birth and death (if applicable).
Case and control identification
The Finnish public health care system covers both primary health care and specialized health services and the mental health care services are provided free of charge for both children and adults. Most patients are referred by primary health services, including child welfare clinics and school health care, to specialized services. ADHD is diagnosed by a specialist in psychiatry or neurology in public outpatient services.
The ADHD cases were identified from the CRHC and included all singletons born in Finland between 1998 and 1999 and diagnosed with ADHD based on the ICD-10 codes of hyperkinetic disorders F90.0, F90.1, F90.8, and F90.9 or with the ICD-9 code 314X before 31.12.2011. Cases who had received the diagnosis of severe or profound mental retardation (F72–F73 in ICD-10 or 318 in ICD-9) and who were diagnosed before the age of 2 but not after that were excluded.
The controls were singleton offspring born in Finland and without a diagnosis of ADHD or conduct disorder (F91–F92) or severe or profound mental retardation (F72–73). Each case is matched with one control on date of birth (± 30 days), sex, and place of birth. The controls were alive and residing in Finland at the time of the diagnosis of the matched cases. Among 1672 identified cases and controls, sufficient serum was available in the FMC for 1026 cases and 1026 matched controls.
Description of biobank in Finland
The Finnish Maternity Cohort (FMC) of the Northern Finland Biobank Borealis [40] was established in 1983 and is a nationwide serum bank with approximately 2 million serum samples collected during the first and early second trimester of pregnancy (5th to 95th percentile: months 2–4 of pregnancy) from over 950,000 women. The FMC covers virtually all pregnancies in Finland during 1983–2016 with archived prenatal serum specimens drawn for routine screening for congenital infections (HIV, Hepatitis B and syphilis). After informed consent, the remaining serum samples (one sample of 1–3 mL for each pregnancy) are stored at − 25 °C in a protected biorepository at the Biobank Borealis and can be used for scientific research [41]. All samples in the FMC can be linked with offspring and other Finnish nationwide registers by a unique PIC that is issued to each resident of Finland since 1971.
Vitamin B12 measurement
To investigate Vitamin B12 levels in the prenatal serum samples, we measured Active B12 (HoloTC, Holotranscobalamin) using a chemiluminescence microparticle immunoassay (CMIA) on the Architect i2000SR automatic immunoassay analyzer (Abbott Diagnostics) according to the manufacturer’s instructions [42]. The coefficient of variation (mean ± SD) derived from repeated quality control samples included in each set of daily assays was 4.7% in the control samples with high B12 levels (range 43.7–49.6 pmol/L) and 6.4% in those with low B12 levels (range 13.6–17.3 pmol/L).
Covariates
A number of covariates that have shown to be associated with both Vitamin B12 and ADHD were examined as potential confounders [4, 7, 37, 43,44,45,46,47,48,49]. We obtained information on the number of previous births, maternal socioeconomic status (SES), maternal age, maternal smoking during pregnancy, gestational age and weight for gestational age from the FMBR. In Finland, the maternal SES categories are based on occupation-based classification that is used in the FMBR: upper white-collar workers, lower white-collar workers, blue-collar workers and others (e.g. students and housewives) or missing (if the data were not available). Information on maternal and paternal psychiatric diagnoses and maternal substance abuse was obtained from the CRHC [4]. Information on maternal immigrant status was obtained from the PRC and included in the analysis, as maternal nutrition deficiency is more common in certain ethnic groups [50] and there is an increased risk for offspring ADHD diagnosis [45]. The FMC was used for information on gestational week and season of blood draw. The seasons of blood collection were defined as winter (December to February), spring (March to May), summer (June to August) and fall (September to November). More description of all covariates is presented in Tables 2 and 3.
Statistical analysis
We examined the association between Vitamin B12 levels as a continuous variable and ADHD. Due to the skewed distribution, Vitamin B12 was log-transformed before analysis. In the secondary analysis, we examined maternal Vitamin B12 classified as quintiles. The cut-off of the quintiles for case and control groups was based on the distribution in the control group. The reference group was the highest quintile. The categorically defined covariates were tested with χ2 and Student’s t tests for the association with log-transformed maternal Vitamin B12 levels among controls, and for the association with ADHD. The covariates were included in the adjusted regression models as potential confounders if they were associated with both the exposure and the outcome at p < 0.1. The point and interval estimate of odds ratios were obtained by fitting conditional logistic regression models for matched pairs. Statistical significance was based on p < 0.05. All the statistical analyses were performed with (SAS 9.4, SAS Institute, Cary, N.C.)
Results
The study included 1026 ADHD case–control pairs. The mean age of diagnosis for cases was 7.3 years (SD 1.9, range 2–14 years).
Table 2 shows the association between covariates and maternal Vitamin B12 among controls. Gestational week of blood draw and maternal SES were associated with maternal Vitamin B12 levels among controls. Table 3 shows the association between covariates and offspring ADHD among case and control subjects. Maternal age, previous births, history of maternal ADHD diagnoses, maternal substance abuse, maternal psychopathology, paternal ADHD diagnoses, paternal psychopathology, maternal smoking, maternal SES, gestational age, weight for gestational age and maternal immigration status were associated with offspring ADHD. Therefore, adjustment was made only for maternal SES.
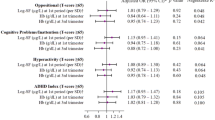
Table 4 shows the unadjusted and adjusted results for the association between maternal serum Vitamin B12 and offspring ADHD. The maternal Vitamin B12 levels, analyzed as a continuous variable, were not associated with offspring ADHD in either the unadjusted (OR 0.96, 95% CI 0.79–1.16, p = 0.68) or the adjusted analyses (aOR 0.97, 95% CI 0.79–1.18, p = 0.75). Maternal Vitamin B12 levels, measured in quintiles, were also not associated with offspring ADHD. There was no significant association between the lowest quintile of maternal Vitamin B12 and ADHD in either the unadjusted (OR 0.96, 95% CI 0.73–1.26, p = 0.77) or the adjusted analyses (aOR 0.96, 95% CI 0.73–1.27, p = 0.80). When an additional analysis was conducted adjusting for all covariates for maternal Vitamin B12 levels measured as a continuous variable, and in quintiles, the findings did not change. As ADHD diagnoses may be considered unreliable before the age of 6 years, we conducted sensitivity analyses, including cases diagnosed at age 6 years or more (n = 948). These cases might have been diagnosed before age 6, but they had to have the diagnosis recorded at six years or more. The findings remained negative in all analyses (Supplementary Table 1).
Discussion
This is the first population-based study examining maternal Vitamin B12 levels in prenatal sera in relation to ADHD in offspring. There was no significant association observed between maternal Vitamin B12 and offspring ADHD. The findings of the study were in line with previous studies based on folate and multivitamin supplementation [31,32,33]. In contrast, the only previous study with offspring ADHD diagnoses from Denmark showed that multivitamin supplementation was associated with a reduced risk for ADHD in offspring [30]. However, the Danish study did not include the levels of serum Vitamin B12 during pregnancy.
The major strengths of the present study are the large nationwide representative sample and availability of maternal Vitamin B12 levels from prospectively collected maternal serum samples during pregnancy. The study was well powered to detect even a relatively small difference between case and control levels of maternal Vitamin B12. Assuming two independent samples and given the number of cases and controls (n = 1026 per group) with alpha set at 5% for a two-sided t test, at 80% power the minimum detectable effect size would have been d = 0.12 (in units of SD), generally considered a “small” effect size.
We note some limitations to our study. First, ADHD is a multifactorial disorder involving a combination of genetic and environmental factors; yet, the present study concerns only Vitamin B12, a single nutrient. However, as in most research studies of complex outcomes, effects can still be observed for single risk factors including micronutrients as in studies of folic acid and neural tube defects [21, 51], and the reduction in risk obtained is also of public health benefit even though the outcome is not entirely eliminated by this intervention. The ultimate goal of this research is to improve the explanatory variance of ADHD, and for that purpose, other groups and we are working to increase the number of micronutrients and other factors quantified. With regard to the present study, folic acid and homocysteine are not measurable in the stored sera; however, one advantage of quantifying serum levels is that it represents a final outcome of such factors, including genes related to homeostatic and metabolic processes and, as in the folic acid/neural tube defects findings, the pathology can be corrected by supplementation of this nutrient even without directly addressing the antecedent factors [21]. Second, we did not quantify neonatal levels of Vitamin B12. However, maternal and neonatal serum levels of Vitamin B12 were significantly correlated with one another in prior work [51]. Third, ADHD cases were referred to specialized services and are likely to represent more severe cases. Fourth, ADHD diagnoses were based on register information. However, our previous study has reported the validity of ADHD diagnosis to be high (88%) [37]. Fifth, information about serum Vitamin B12 levels was restricted to the first and early second trimesters of pregnancy, and thus the findings cannot be generalized to those occurring later in pregnancy.
The present study does not support the hypothesis that Vitamin B12 deficiency during pregnancy is an etiological factor for offspring ADHD. Some previous studies have suggested that maternal multivitamin or folate supplementation and high homocysteine levels might have an association with offspring neuropsychiatric disorders such as autism and schizophrenia [52,53,54,55]. In a large birth cohort, the Child Health and Development Study, Brown et al. [55] demonstrated that maternal homocysteine levels in the highest tertile of the distribution were related to a greater than twofold increased risk of schizophrenia among offspring. It has been suggested that one possible explanation for these associations could be related to dysfunction in one-carbon metabolism resulting in altered DNA methylation [56]. Low folate causes high homocysteine in maternal serum through a disruption in methionine metabolism, which may induce abnormal fetal brain development. Of note, the present study is not comparable with previous studies on other neuropsychiatric disorders that have not specifically measured Vitamin B12 levels during pregnancy. Future studies should address the possibility that maternal Vitamin B12 deficiency has specificity as an etiological factor for some disorders but not others as well as the possibility that Vitamin B12 could be related to offspring ADHD only in mothers or offspring with a genetic mutation that alters one-carbon metabolism. This has been suggested in studies of gene variants such as methylene tetrahydrofolate reductase (MTHFR), folic acid, and neural tube defects [57].
References
Thapar A, Cooper M (2016) Attention deficit hyperactivity disorder. Lancet 387:1240–1250
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA (2015) Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 56:345–365. https://doi.org/10.1111/jcpp.12381
Banerjee TD, Middleton F, Faraone SV (2007) Environmental risk factors for attention-deficit hyperactivity disorder. Acta Paediatr 96:1269–1274. https://doi.org/10.1111/j.1651-2227.2007.00430.x
Joelsson P, Chudal R, Uotila J, Suominen A, Sucksdorff D, Gyllenberg D, Sourander A (2017) Parental psychopathology and offspring attention-deficit/hyperactivity disorder in a nationwide sample. J Psychiatr Res 94:124–130. https://doi.org/10.1016/j.jpsychires.2017.07.004
Sucksdorff M, Lehtonen L, Chudal R, Suominen A, Gissler M, Sourander A (2018) Lower Apgar scores and Caesarean sections are related to attention-deficit/hyperactivity disorder. Acta Paediatr 107:1750–1758. https://doi.org/10.1111/apa.14349
Sourander A, Sucksdorff M, Chudal R, Surcel H, Hinkka-Yli-Salomäki S, Gyllenberg D, Cheslack-Postava K, Brown AS (2019) Prenatal cotinine levels and ADHD among offspring. Pediatrics. https://doi.org/10.1542/peds.2018-3144
Sucksdorff M, Lehtonen L, Chudal R, Suominen A, Joelsson P, Gissler M, Sourander A (2015) Preterm birth and poor fetal growth as risk factors of attention-deficit/hyperactivity disorder. Pediatrics 136:599. https://doi.org/10.1542/peds.2015-1043
Brown AS, Susser ES (2005) Homocysteine and schizophrenia: from prenatal to adult life. Prog Neuropsychopharmacol Biol Psychiatry 29:1175–1180
Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, Gorman JM (1996) Schizophrenia after prenatal famine. Further evidence. Arch Gen Psychiatry 53:25–31
Susser E, Hoek HW, Brown A (1998) Neurodevelopmental disorders after prenatal famine: the story of the Dutch Famine Study. Am J Epidemiol 147:213–216
Xu M, Sun W, Liu B, Feng G, Yu L, Yang L, He G, Sham P, Susser E, St Clair D, He L (2009) Prenatal malnutrition and adult schizophrenia: further evidence from the 1959–1961 Chinese famine. Schizophr Bull 35:568–576. https://doi.org/10.1093/schbul/sbn168
St Clair D, Xu M, Wang P, Yu Y, Fang Y, Zhang F, Zheng X, Gu N, Feng G, Sham P, He L (2005) Rates of adult schizophrenia following prenatal exposure to the Chinese famine of 1959–1961. JAMA 294:557–562. https://doi.org/10.1001/jama.294.5.557
Brown AS, Susser ES, Lin SP, Neugebauer R, Gorman JM (1995) Increased risk of affective disorders in males after second trimester prenatal exposure to the Dutch hunger winter of 1944–45. Br J Psychiatry 166:601–606. https://doi.org/10.1192/bjp.166.5.601
Brown AS, van Os J, Driessens C, Hoek HW, Susser ES (2000) Further evidence of relation between prenatal famine and major affective disorder. Am J Psychiatry 157:190–195. https://doi.org/10.1176/appi.ajp.157.2.190
King JC (1437S) A summary of pathways or mechanisms linking preconception maternal nutrition with birth outcomes. J Nutr 146:1437S–S1444
Li M, Francis E, Hinkle SN, Ajjarapu AS, Zhang C (2017) Preconception and prenatal nutrition and neurodevelopmental disorders: a systematic review and meta-analysis. Nutrients 11:1628
Georgieff MK (2007) Nutrition and the developing brain: nutrient priorities and measurement. Am J Clin Nutr 85:614S–620S. https://doi.org/10.1093/ajcn/85.2.614S
Keenan K, Hipwell AE (2015) Modulation of prenatal stress via docosahexaenoic acid supplementation: implications for child mental health. Nutr Rev 73:166–174. https://doi.org/10.1093/nutrit/nuu020
Fretham SJB, Carlson ES, Georgieff MK (2011) The role of iron in learning and memory. Adv Nutr 2:112–121. https://doi.org/10.3945/an.110.000190
Skeaff SA (2011) Iodine deficiency in pregnancy: the effect on neurodevelopment in the child. Nutrients 3:265–273. https://doi.org/10.3390/nu3020265
McGrath J, Brown A, St Clair D (2011) Prevention and schizophrenia—the role of dietary factors. Schizophr Bull 37:272–283
Pepper MR, Black MM (2011) B12 in fetal development. Semin Cell Dev Biol 22:619–623. https://doi.org/10.1016/j.semcdb.2011.05.005
Kräutler B (2012) Biochemistry of B12-cofactors in human metabolism. Water Soluble Vitam. https://doi.org/10.1007/978-94-007-2199-9_17
Refsum H (2001) Folate, vitamin B12 and homocysteine in relation to birth defects and pregnancy outcome. Br J Nutr 85(Suppl 2):109
Black MM (2008) Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr Bull 29:126. https://doi.org/10.1177/15648265080292S117
Bunout D, Barrera G, Hirsch S, Gattas V, de la Maza M, Pía HF, Steenhout P, Klassen P, Hager C, Avendaño M, Petermann M, Muñoz C (2004) Effects of a nutritional supplement on the immune response and cytokine production in free-living Chilean elderly. JPEN J Parenter Enteral Nutr 28:348–354. https://doi.org/10.1177/0148607104028005348
Pitkin RM (2007) Folate and neural tube defects. Am J Clin Nutr 85:285S–288S. https://doi.org/10.1093/ajcn/85.1.285S
MRC Vitamin Study Research Group (1991) Prevention of neural tube defects: results of the medical research council vitamin study. Lancet 338:131–137. https://doi.org/10.1016/0140-6736(91)90133-A
Schlotz W, Jones A, Phillips DIW, Gale CR, Robinson SM, Godfrey KM (2010) Lower maternal folate status in early pregnancy is associated with childhood hyperactivity and peer problems in offspring. J Child Psychol Psychiatry 51:594–602. https://doi.org/10.1111/j.1469-7610.2009.02182.x
Virk J, Liew Z, Olsen J, Nohr EA, Catov JM, Ritz B (2018) Pre-conceptual and prenatal supplementary folic acid and multivitamin intake, behavioral problems, and hyperkinetic disorders: a study based on the Danish National Birth Cohort (DNBC). Nutr Neurosci 21:352–360. https://doi.org/10.1080/1028415X.2017.1290932
D'Souza S, Waldie KE, Peterson ER, Underwood L, Morton SMB (2019) Antenatal and postnatal determinants of behavioural difficulties in early childhood: evidence from growing up in New Zealand. Child Psychiatry Hum Dev 50:45–60. https://doi.org/10.1007/s10578-018-0816-6
Julvez J, Fortuny J, Mendez M, Torrent M, Ribas-Fitó N, Sunyer J (2009) Maternal use of folic acid supplements during pregnancy and four-year-old neurodevelopment in a population-based birth cohort. Paediatr Perinat Epidemiol 23:199–206. https://doi.org/10.1111/j.1365-3016.2009.01032.x
Miyake Y, Tanaka K, Okubo H, Sasaki S, Arakawa M (2018) Maternal B vitamin intake during pregnancy and childhood behavioral problems in Japan: The Kyushu Okinawa Maternal and Child Health Study. Nutr Neurosci. https://doi.org/10.1080/1028415X.2018.1548139
World Health Organization (1992) International Classification of Diseases, 10th Revision (ICD-10). The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. WHO, Geneva
World Health Organization (1977) International Classification of Diseases, Ninth Revision (ICD-9). WHO, Geneva
World Health Organization (1967) International Classification of Diseases, Eight Revision (ICD-8). WHO, Geneva
Joelsson P, Chudal R, Gyllenberg D, Kesti A, Hinkka-Yli-Salomäki S, Virtanen J, Huttunen J, Ristkari T, Parkkola K, Gissler M, Sourander A (2016) Demographic characteristics and psychiatric comorbidity of children and adolescents diagnosed with ADHD in specialized healthcare. Child Psychiatry Hum Dev 47:574–582. https://doi.org/10.1007/s10578-015-0591-6
Tripp G, Luk SL, Schaughency EA, Singh R (1999) DSM-IV and ICD-10: a comparison of the correlates of ADHD and hyperkinetic disorder. J Am Acad Child Adolesc Psychiatry 38:156–164. https://doi.org/10.1097/00004583-199902000-00014
Lahey BB, Pelham WE, Chronis A, Massetti G, Kipp H, Ehrhardt A, Lee SS (2006) Predictive validity of ICD-10 hyperkinetic disorder relative to DSM-IV attention-deficit/hyperactivity disorder among younger children. J Child Psychol Psychiatry 47:472–479. https://doi.org/10.1111/j.1469-7610.2005.01590.x
Oulu University Hospital: Biobank Borrealis
Gissler M, Surcel H (2012) Combining health register data and biobank data. Stat J IAOS 28:53–58. https://doi.org/10.3233/SJI-2012-0744
Golding PH (2016) Holotranscobalamin (HoloTC, Active-B12) and Herbert’s model for the development of vitamin B12 deficiency: a review and alternative hypothesis. Springerplus. https://doi.org/10.1186/s40064-016-2252-z
Carballo JJ, García-Nieto R, Alvarez-García R, Caro-Cañizares I, López-Castromán J, Muñoz-Lorenzo L, de Leon-Martinez V, Baca-García E (2013) Sibship size, birth order, family structure and childhood mental disorders. Soc Psychiatry Psychiatr Epidemiol 48:1327–1333. https://doi.org/10.1007/s00127-013-0661-7
Joelsson P, Chudal R, Talati A, Suominen A, Brown AS, Sourander A (2016) Prenatal smoking exposure and neuropsychiatric comorbidity of ADHD: a Finnish nationwide population-based cohort study. BMC Psychiatry 16:306. https://doi.org/10.1186/s12888-016-1007-2
Lehti V, Chudal R, Suominen A, Gissler M, Sourander A (2016) Association between immigrant background and ADHD: a nationwide population-based case-control study. J Child Psychol Psychiatry 57:967–975
Chudal R, Joelsson P, Gyllenberg D, Lehti V, Leivonen S, Hinkka-Yli-Salomäki S, Gissler M, Sourander A (2015) Parental age and the risk of attention-deficit/hyperactivity disorder: a nationwide, population-based cohort study. J Am Acad Child Adolesc Psychiatry 54:487–494.e1. https://doi.org/10.1016/j.jaac.2015.03.013
Tuenter A, Bautista Nino PK, Vitezova A, Pantavos A, Bramer WM, Franco OH, Felix JF (2019) Folate, vitamin B12, and homocysteine in smoking-exposed pregnant women: a systematic review. Maternal Child Nutr 15:e12675
Rogne T, Tielemans MJ, Chong MF, Yajnik CS, Krishnaveni GV, Poston L, Jaddoe VW, Steegers EA, Joshi S, Chong Y (2017) Maternal vitamin B12 in pregnancy and risk of preterm birth and low birth weight: a systematic review and individual participant data meta-analysis. Am J Epidemiol 185:212
Krajcovicová-Kudlácková M, Valachovicová M, Blazícek P (2013) Seasonal folate serum concentrations at different nutrition. Cent Eur J Public Health 21:36–38
Devi A, Rush E, Harper M, Venn B (2018) Vitamin B12 status of various ethnic groups living in New Zealand: an analysis of the adult nutrition survey 2008/2009. Nutrients. https://doi.org/10.3390/nu10020181
Peker E, Demir N, Tuncer O, Üstyol L, Balahoroğlu R, Kaba S, Karaman K (2016) The levels of vitamın B12, folate and homocysteine in mothers and their babies with neural tube defects. J Matern Fetal Neonatal Med 29:2944–2948
Schmidt RJ, Iosif A, Guerrero Angel E, Ozonoff S (2019) Association of maternal prenatal vitamin use with risk for autism spectrum disorder recurrence in young siblings. JAMA Psychiatry 76:391–398
Levine SZ, Kodesh A, Viktorin A, Smith L, Uher R, Reichenberg A, Sandin S (2018) Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring. JAMA Psychiatry 75:176–184. https://doi.org/10.1001/jamapsychiatry.2017.4050
Picker JD, Coyle JT (2005) Do maternal folate and homocysteine levels play a role in neurodevelopmental processes that increase risk for schizophrenia? Harv Rev Psychiatry 13:197–205
Brown AS, Bottiglieri T, Schaefer CA, Quesenberry CP, Liu L, Bresnahan M, Susser ES (2007) Elevated prenatal homocysteine levels as a risk factor for schizophrenia. Arch Gen Psychiatry 64:31–39
Lee H (2015) Impact of maternal diet on the epigenome during in utero life and the developmental programming of diseases in childhood and adulthood. Nutrients 7:9492–9507
Etheredge AJ, Finnell RH, Carmichael SL, Lammer EJ, Zhu H, Mitchell LE, Shaw GM (2012) Maternal and infant gene-folate interactions and the risk of neural tube defects. Am J Med Genet A 158A:2439–2446
Acknowledgements
The study was supported by the following funding sources: the Academy of Finland Flagship Programme, decision number: 320162, the Strategic Research Council at the Academy of Finland, decision number: 303581, the Academy of Finland Health from Cohorts and Biobanks Programme, decision number: 308552, and the National Institute of Environmental Health Sciences, Grant number: 5R01ES028125. Silwal and Upadhyaya received funding from University of Turku Graduate School. This research was supported by the INVEST Research Flagship, APEX Research Consortium and PSYCOHORTS consortium. We thank the investigators and staff at the medical centers involved in this research.
Funding
Open access funding provided by University of Turku (UTU) including Turku University Central Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The ethical approval for the study was provided by the Ethics Committee of the Hospital District of Southwest Finland, by the data protection authorities at the National Institute for Health and Welfare, and by the Institutional Review Board of the New York State Psychiatric Institute. Informed consent was obtained before collection of maternal serum.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sourander, A., Silwal, S., Upadhyaya, S. et al. Maternal serum Vitamin B12 and offspring attention-deficit/hyperactivity disorder (ADHD). Eur Child Adolesc Psychiatry 30, 1449–1462 (2021). https://doi.org/10.1007/s00787-020-01621-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01621-5