Abstract
Aim
To investigate the outcome of elective full pulpotomy, using calcium silicate-based cements (CSBC), after 2 years, in symptomatic mature permanent teeth with carious lesions, diagnosed as irreversible pulpitis, and analyse the capacity of Wolters et al. (2017) classification to predict the likelihood of treatment failure.
Methods
The treatment records of 56 patients with symptomatic mature teeth with carious lesions, diagnosed as irreversible pulpitis and treated by elective full pulpotomy, using CSBCs as pulp capping materials, were reviewed. Thirteen teeth were excluded. The remaining 43 teeth were evaluated retrospectively at 24 months. Fisher`s exact test with the Lancaster’s mid-P adjustment was used to assess different outcomes amongst the diagnostic categories.
Results
Four of the cases failed before 24 months and required root canal treatment (RCT). Overall success rate at 2 years was 90.7% (39 of 43). An inverse, but non-significant, correlation was observed between the severity of pulpitis according to the Wolters classification and the treatment success rate (p > 0.05). The type of CSBC used was associated to the success rate (OR = 10.5; 95% C.I. = 0.5 – 207.4; p = 0.027), being 82% with Endosequence and 100% with Biodentine. Postoperative pain associated significantly to lower success rate (66.7%) (Odds ratio = 8.0; 95% C.I. = 0.7 – 95.9; p = 0.047).
Conclusions
Elective full pulpotomy using a CSBC was a successful choice for the treatment of mature permanent teeth with symptoms indicative of irreversible pulpitis. There were no significant differences between the success rate of mild, moderate and severe pulpitis. Postoperative pain could be considered a risk marker for failure of full pulpotomy. The term “irreversible pulpitis” should be re-signified to indicate the need for access to the pulp chamber, rather than an indication for extraction or RCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Caries lesion is the most common cause of pulpitis in mature permanent teeth [30]. For decades, pulpitis has been classified, according to the AAE diagnostic criteria [3], as reversible and irreversible. Vital pulp therapy techniques, including pulp capping and pulpotomy, have been used to treat reversible pulpitis [14], while irreversible pulpitis was treated using root canal therapy (RCT) [33].
Lingering pain after cold stimuli and spontaneous pain, are the main criteria used by the AAE classification to determine that pulp is irreversibly affected [3, 4]. Typical pain characteristics that lead to the diagnosis of symptomatic irreversible pulpitis are: sharp and lingering pain triggered by thermal stimulus (often 30 s or longer after stimulus removal), spontaneous pain and often referred pain. The pain can be accentuated by postural changes such as lying down or bending over, and over-the-counter analgesics are typically ineffective [4].
However, numerous studies have shown that there is no exact correlation between the pain symptom and the pulpal inflammatory state [13, 15, 23, 30]. Histological studies have shown that in patients with symptoms of irreversible pulpitis, the inflammatory and infectious process often involved only the coronal pulp tissue underlying the carious lesion, with the root pulp tissue being practically healthy [41]. These findings suggest that strict application of the AAE classification could lead to over-prescription of root canal treatment [17, 33]. Furthermore, in some cases of pulpitis, theoretically irreversible, vital pulp therapy techniques could allow pulpitis to be cured without having to perform RCT. In 2017, Wolters et al. [51] suggested leaving aside the AAE dichotomous classification pulpitis and applying a new classification that recommended more conservative and less invasive treatments. This new classification completely changed the therapeutic attitude towards pulpitis. For Wolters et al. [51] the goal of treatment should be to remove irreversibly inflamed tissue and preserve the remaining normal or reversibly inflamed pulp tissues. The main concept is that vital pulp tissue, managed properly, is quite resistant, and a diseased pulp can heal if most of the inflamed/necrotic tissue is removed [51]. Along these same lines, the ESE clinical practice guideline on the treatment of pulpal and apical disease [26], recommended pulpotomy, full or partial, for patients diagnosed with nontraumatic pulpitis associated with spontaneous pain in permanent teeth. Moreover, pulpotomy is generally quicker, less technically complex, and less invasive than root canal treatment, reducing the risk of unwanted effects such as fracture, or residual periapical inflammation [24, 26].
A full, coronal or complete pulpotomy involves the ‘complete removal of the coronal pulp and the application of a biomaterial onto the pulp tissue at the level of the root canal orifice(s)’ [24]. Numerous studies have been published demonstrating that full pulpotomy, carried out using mineral trioxide aggregate (MTA), or CSBCs such as Biodentine (Septodont) or Endosequence (Brasseler), achieves a success rate greater than 90% in teeth with supposedly irreversible pulpitis symptoms [7, 9, 16, 18, 22, 46,47,48]. These results have led the ESE to recommend full pulpotomy for patients with teeth diagnosed with nontraumatic pulpitis associated with lingering pain after cold stimuli or spontaneous pain [26].
However, most of the studies on the outcome of full pulpotomy in teeth with irreversible pulpitis do not provide data on some important variables, such as clinical data on which the preoperative diagnosis was based, depth of the carious lesion, and characteristics of the patient's pain. Moreover, although the capability of the Wolters classification in predicting the likelihood of partial pulpotomy failure has been investigated [13], data are needed on its ability to predict the outcome of full pulpotomy. Furthermore, published studies on the outcome of full pulpotomy usually refer to cases in which pulpotomy was performed after the occurrence of pulp exposure during carious tissue removal [31, 36, 39, 46,47,48]. There have been few studies evaluating the outcome of full pulpotomy performed electively to treat irreversible pulpitis [5, 40].
The aim of this study was to retrospectively investigate the outcome of elective full pulpotomy after 2 years, using CSBC, in symptomatic mature permanent teeth with carious lesions, diagnosed according to AAE classification as symptomatic irreversible pulpitis, and investigating the factors that may affect the outcome of the treatment. As a secondary objective, the capacity of Wolters et al. [51] classification to predict the likelihood of treatment failure was analysed.
Methods
Case selection
The Ethics Committee of the institutional review board of the University of Sevilla approved our retrospective study (protocol number 2024–1209). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients included in the study had given their informed consent so that data from their medical history could be used in research.
This retrospective study has been conducted according to PROBE 2023 guidelines for reporting observational studies in Endodontics [35]. The study was carried out with the medical records of patients treated from January 2021 to December 2021.
All included patients had been diagnosed as having irreversible pulpitis according to the AAE, so RCT had been indicated. However, if after accessing the pulp chamber the bleeding had been controlled in less than 5 min, elective full pulpotomy had been performed. Before receiving treatment, all patients had given informed consent so that their data could be used in any research study. Clinical data on the patients that had undergone full pulpotomy, including their radiographs, were retrieved from the database.
Fifty-six patients between 11–76 years old diagnosed with irreversible pulpitis [4] and reporting occlusal/proximal caries lesion, whose clinical history included data on the characteristics of the pain and the intraoral examination that justified the diagnosis of irreversible pulpitis, were included.
Inclusion and exclusion criteria
The inclusion criteria were: (1) pulpotomy had been carried out in mature teeth with a probing pocket depth and mobility within normal limits; (2) with a carious lesion reaching the middle or inner third of dentine [24]; (3) had a preoperative diagnose of irreversible pulpitis according to the AAE classification [4], and providing data about pain characteristics and response to pulp sensitivity tests; (4) had no signs of sinus tract or swelling; (5) periapical radiograph indicated a normal periapical status (PAI score 1–2) [37]; (6) the tooth had been restored; (7) the medical record provided data on the outcome of the treatment over 24 months.
The exclusion criteria were: (1) pulpotomy in immature teeth; (2) pulpotomy carried out after pulp exposure during the removal of carious tissue; (3) pulpotomy performed to treat a pulpal exposure of traumatic origin; (4) the treatment record did not provide sufficient information on the clinical data supporting the diagnosis of irreversible pulpitis; (5) the medical record does not provided information about the outcome of the treatment over 24 months; (6) patients with systemic disease that could affect the outcome of treatment.
Treatment protocol of pulpotomy
All database treatments had been carried out by the same operator (C.J-M.), which had followed the same protocol in all cases, but using two different CSBC: Biodentine (Septodont) or Endosequence BC RRM Fast Set Putty (Brasseler).
After diagnosis of irreversible pulpitis, local anesthesia had been carried out using 4% articaine with 1:100,000 epinephrine. After rubber dam isolation, the crown of the tooth had been disinfected with 5% NaOCl. Removal of carious tissue had been carried out under sterile water cooling using high-speed tungsten carbide fissure burs, slow-speed round burs, and a spoon excavator. In the periphery of the lesion, the affected tissue had been removed until reaching hard dentin, while in the central area of the lesion, the spoon excavator had been used until reaching soft dentin.
After removing the carious tissue, the pulp chamber had been accessed using a round tungsten carbide bur, and the chamber roof had been completely removed. After pulp exposure, pulp vitality had been confirmed by the presence of bleeding pulp tissue and by the achievement of hemostasis by applying a cotton wool moistened with 5% NaOCl for 2 min, with a dry cotton ball at the top. This operation had been repeated if necessary for a period of 5 min [24, 26]. In all cases included in the study, hemostasis had been achieved in less than 5 min. When this had not been achieved, root canal treatment had been prescribed.
Once hemostasis was achieved, the coronal pulp was removed up to cement-enamel junction in single-rooted teeth, and up to the level of root canal orifices in multi-rooted teeth, using a sterile diamond round bur under water coolant and amputated with a sharp spoon excavator. Remains of pulp tissue were removed using the Start-X #1 ultrasonic tip (DentsplySirona). Then, the cavity was flushed with sterile saline water and the pulp wound was stanched with sterile cotton pellet soaked with 5% sodium hypochlorite for 1 min.
A 2-mm-thick layer of CSBC was then applied on the top of the remaining root pulp with gentle pressure with a clean cotton pellet. In multi-rooted teeth, the cement was placed on the root canal orifices and the whole pulp chamber floor following the manufacturer's instructions. After waiting 12 min (Biodentine) or 20 min (Endosequence) for the biomaterial to set, a layer of glass ionomer (Vitrebond Plus, 3 M) was placed. The pulp chamber was rinsed with alcohol to clean any remaining biomaterial, selectively etched with 37% orthophosphoric acid for 30 s, rinsed with water, and dried with the air/water syringe. The composite resin had been applied with the incremental technique and each layer had been polymerized for 20 – 40 s. Once the tooth reconstruction was completed, the occlusion was checked and the restoration was polished. Finally, an end-of-treatment x-ray had been taken and the patient had been scheduled for subsequent check-ups. When an inlay and/or crown was indicated, the patient was rescheduled for a second appointment for the prosthetic restoration.
Data collection
In each medical history the following data had been recovered: name, age, sex, tooth type, characteristics of pain, probing pocket depth, tooth mobility, interpretations of preoperative radiographs, tooth surfaces affected by caries, depth of the caries lesion, preoperative PAI score [37], and pulpitis diagnose according to AAE classification [3, 4], which in all cases was irreversible pulpitis. The depth of the carious lesion was evaluated on the periapical radiograph and was classified into two types, depending on whether it reached the inner third or the middle third of the dentin.
With the data from the clinical history, each case was classified as mild, moderate or severe pulpitis, according to the classification suggested by Wolters et al. [51].
The following data regarding treatment were also recovered: CSBC used, number of visits and type of the coronal restoration (resin composites or inlay).
Postoperative pain was considered present when patients consulted for pain during the week following treatment. If there was no consultation due to post-treatment discomfort or pain, it was considered absent.
Finally, regarding the postoperative period and follow-up visits, the following data, when they appeared registered, were collected: history of spontaneous pain or discomfort, response to the cold pulp sensitivity test, pain when biting, pain on percussion, probing pocket depth, color changes, radiographic periapical status (PAI score), presence of root canal obliteration, and presence of root resorption.
Assessment of treatment outcome
The clinical criteria used to assess the outcome of the treatment were based on previous research [25, 46, 53]: no history of spontaneous pain or discomfort, except for the first week after treatment; no swelling; no tenderness to palpation or percussion and the tooth is functional; normal mobility and probing pocket depth; soft tissues around the tooth are normal with no swelling or sinus tract.
In addition, the outcome was also assessed radiographically using the following criteria: absence of emerging root periapical or periradicular radiolucent image, and PAI score ≤ 2. When all these clinical and radiographical conditions were met, the treatment was considered successful.
Statistical analysis
Sample size was calculated based on the success rate of previous studies [39, 44] using a method of comparing two proportions [42] for a study with α = 5% and power of 80%, a minimum of 42 participants were required for the results to be statistically meaningful.
The collected data was entered into Excel software, Version 2019 (Microsoft). The success rate were determined. Fisher`s exact test with the Lancaster’s mid-P adjustment [11] was used to assess the influence of various factors for pulpotomy success. Haldane-Anscombe correction was used to calculate odds ratios if any of the cell expectations would cause a division by zero error. The OpenEpi Module for Diagnostic Test Evaluation (https://www.openepi.com/DiagnosticTest/DiagnosticTest.htm) [19] was used to analyse postoperative pain as diagnostic indicator for the outcome of pulpotomy. Significance was set at p < 0.05.
Results
Sample characteristics
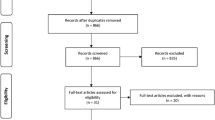
Initially, 56 pulpotomy cases were found that seemed to meet the inclusion criteria. However, after carefully reviewing the medical records, thirteen cases were excluded for the following reasons: immature teeth (n = 2), pulpotomy after pulp exposure (n = 2), pulpotomy after traumatic injury (n = 1), insufficient data about pain characteristics and diagnosis (n = 6), and no information about the outcome of the treatment over 24 months (n = 2). There remained 43 pulpotomy cases that were included in the study and analysed (Fig. 1).
The treatment of all pulpotomies had been carried out by the same operator. The only variation in the protocol had been the type of CSBC: Biodentine (Septodont) had been used in 21 cases and Endosequence (Brasseler) in 22 cases (Fig. 2).
Full pulpotomy clinical protocol. (A) After cavity access, coronal pulp tissue was removed. Pulpal hemorrhage is evident. (B) Cotton pellet soaked in 2.5% NaOCl, pressed against the exposed pulp tissue. (C) Hemostasis obtained after five minutes by placing cotton pellet. (D) Biodentine™ used to restore the entire cavity. (E) Vitrebond placed between Biodentine and composite material. (F) Tooth permanently restored with resin-based composite material
The summary outcomes during the follow-up period are shown in Table 1. Four of the cases failed before 24 months and required root canal treatment (RCT). The first failed case had been diagnosed as moderate pulpitis, showing spontaneous pain, pain on biting and tenderness to percussion at 2 weeks, being diagnosed as severe pulpitis and emerging apical periodontitis. RCT was indicated. The next three failures occurred in teeth that had been diagnosed as moderate pulpitis. They occurred at 14, 20 and 23 months, all of them showing intense spontaneous pain and being diagnosed as severe pulpitis. In one of them the restoration was leaked (Fig. 3).
Outcome
The characteristics of the included cases according to the type of pulpitis diagnosed, and the success rates at two years are shown in Table 2. Of the 43 cases with irreversible pulpitis treated with full pulpotomy, 39 met the success criteria after 2 years of follow-up (success rate = 90.7%).
Relating outcome to preoperative diagnosis according to the criteria of Wolters et al. [51] revealed that teeth with mild pulpitis were 100% successful, 88.5% moderate pulpitis successful and severe pulpitis 80.0% successful at 2 year. There were no significant differences between the success rate of “mild” and “moderate” pulpitis (p = 0.27), “moderate” and “severe” pulpitis (p = 0.68) or “mild” and “severe” pulpitis (p = 0.16) at 2 years follow-up.
Table 3 shows the characteristics of the cases and their relationship with the treatment outcome. Sex, age, or the number of roots of the treated tooth did not influence the success rate (p > 0.05). Neither the type of preoperative pain, nor the affected tooth surface, nor its depth, significantly influenced the treatment result (p > 0.05).
Regarding intraoperative factors, bleeding time after pulp access had been ≤ 5 min in all cases, without the medical records collecting more details. No significant association was found with the type of restoration performed and the number of appointments (p > 0.05). On the contrary, the type of CSBC used was associated to the success rate (OR = 10.5; 95% C.I. = 0.5 – 207.4; p = 0.027). In the treatments performed with Endosequence there were 4 failures (success rate of 81.9%), while in those performed with Biodentine there were no failures (100% success) (Figs. 4 and 5).
Top: full pulpotomy using Endosequence (A) Left lower first molar (36) with symptoms of irreversible pulpitis. (B) Full pulpotomy with Endosequence (this material is more radiopaque than biodentine). (C) Follow-up x-ray at 12 months. (D) Follow-up x-ray at 2-years. Bottom: full pulpotomy using Biodentine. (A) Left lower first molar (36) with symptoms of irreversible pulpitis and left lower second premolar (35) with pain on percussion, negative response to pulp test, and signs of apical periodontitis. (B) Full pulpotomy with Biodentine (36) and root canal treatment (35). (C) Follow-up x-ray at 12 months. (D) Follow-up x-ray at 2 years
Marginal leakage of restoration was not related to treatment outcome (p > 0.05). Only one of the four failure cases showed marginal leakage. However, a significant association was found between the presence of postoperative pain and the treatment outcome.
Cases in which the patient had postoperative pain (14.0%) showed a significantly lower success rate (66.7%) than cases in which there was no postoperative pain (95.9%) (Odds ratio = 8.0; 95% C.I. = 0.7 – 95.9; p = 0.047). Presence of postoperative pain showed a sensitivity of 50% (15.0%—85.0%), a specificity of 89.7% (76.4%—95.9%) and a diagnostic accuracy of 86.1% (72.7%—93.4%). Its negative predictive value was 94.6% (82.3%—98.5%). No correlation was found between postoperative and preoperative pain (p = 0.68).
None of the successfully treated teeth showed pain on biting, pain on percussion, abnormal probing pocket depth, presence of root canal obliteration, or presence of root resorption throughout the follow-up period.
At 24 months, the 39 teeth evaluated showed PAI scores less than or equal to 2. Only four teeth (10.3%) responded positively to the cold pulp sensitivity test: an upper second premolar (15), two lower first molars (36 and 46), and one upper first molar (26). Likewise, in only one of the treated teeth (45) a darkening of the crown was observed.
Discussion
This retrospective study aimed, first of all, to analyze the outcome of elective full pulpotomy in mature permanent teeth with carious lesions and diagnosed as symptomatic irreversible pulpitis, after 2 years of follow-up. The results have shown a success rate of 90.7%, indicating that elective full pulpotomy is a successful treatment for irreversible pulpitis in mature permanent teeth with carious lesions. These results, together with those of a large body of previous research [34], show that full pulpotomy is effective and predictable, and can be considered a simpler, less invasive and cheaper option to RCT for the management of irreversible pulpitis in mature teeth.
Regarding the second objective, to analyse the ability of Wolters classification [51] to predict failure of full pulpotomy, the results show an inverse correlation between the severity of pulpitis and the success rate of the treatment, with the success rate being 100% and 88.5% in cases diagnosed as mild or moderate pulpitis, respectively, observing the lowest success rate (80%) in cases of severe pulpitis. However, these differences were not statistically significant (p > 0.05).
The methodology used in this study has followed the PROBE 2023 guidelines for reporting observational studies in Endodontics [35]. Although it is a retrospective study, it is important to note that all the included cases had been performed by the same operator, who had followed the same strict protocol in all of them. The only intraoperative variable had been the type of CSBC. Likewise, th operator had taken very precise notes of the variables analyzed, which subsequently facilitated data collection and avoided many of the drawbacks that most retrospective studies have. Moreover, in all cases included in the study, the clinical history stated that pulpal hemostasis had been achieved in less than 5 min, suggesting that the pulp inflammation was limited in all cases to the coronal pulp [1]. Then, full pulpotomy had been well indicated according to scientific evidence [24, 26].
It is important to make some comments on the statistical treatment carried out. The Lancaster's mid-P (LMP) correction to the Fisher’s exact test (FET) has been used. The conventional approach to calculating the p value for FET has been shown to be conservative, requiring more evidence than is necessary to reject a false null hypothesis [11]. On the contrary, the LMP correction to the FET is less conservative and more powerful. The LMP test provide a better balance of Type I and Type II errors, when compared with the FET, and produce higher levels of power than the FET while still adhering closely to the desired 0.05 significance level.
Full pulpotomy has been proposed as an alternative to RCT for the management of teeth with deep carious lesions and symptoms of irreversible pulpitis [24, 26]. In the present study, unlike in others published previously [31, 36, 39, 46,47,48], full pulpotomy was not performed after pulp exposure following the removal of carious tissue, but was directly chosen, after the patient's informed consent, as the elective treatment for symptomatic irreversible pulpitis. Other studies had already analyzed the results of elective full pulpotomy in relation to the success rate [46, 53] or the response to pulp tests in the treated teeth [5], with alike results. Taha et al. [46] and Zhu et al. [53] found a success rates at 12-months of 97.5% and 92.6%, respectively, for elective full pulpotomy.
The success criteria that have been applied to assess the outcome of the treatment are similar to those previously used by other researchers [25, 46, 53]. The success rate calculated is comparable to that found in other retrospective studies, such as 93.1% [36] and 92.6% [53]. The slightly lower value may be due to the fact that both previous studies only had a 12-month follow-up, while the present study has a 24-month follow-up. However, the success rates found in previous prospective studies [9, 38, 40] and in randomized clinical trials [31, 39, 48], including teeth with symptomatic irreversible pulpitis, are also very similar, ranging 89.8%-93.8%.
Among all the variables analyzed, sex, age and the number of roots did not influence the success rate. Other previous studies have also not found any influence of these factors on the outcome of full pulpotomy [47]. Furthermore, the reviews carried out [25, 28] have concluded that the result of partial/complete pulpotomy is not influenced by age and can be considered a successful treatment in men and women of any age, and in any type of tooth.
The depth of the carious lesion has been related to both the preoperative state of the pulp and the outcome of the treatment [25, 30]. Moreover, the result of partial pulpotomy has been shown to be influenced by the depth of the carious lesion [13]. However, in the present study, although teeth with deep carious lesions had a lower success rate (87%) compared to those that did not reach the inner third (100%), there was no significant association between the caries depth and the success rate (p > 0.05). This could be because in neither case the carious lesion was extremely deep. Only 30 of the included cases were deep carious lesions [24], reaching the inner third of the dentin, while the other 13 were lesions that only reached the middle third. It has been shown that when the lesion affects the inner quarter of the dentin, the bacteria predominate in the primary dentin [12], and only contact the pulp in extremely deep lesions, in which inflammatory infiltrate and partial pulp necrosis are found underlying the lesion [20].
The location of the caries lesion and the affected surface did not significantly influence the treatment result (p > 0.05), although the success rate was lower (87%) in patients with involvement of the proximal surfaces. Other studies have found similar findings [36, 40]. Nor has any influence of the affected surface on the postoperative response to cold stimuli been found [5].
It could be expected that the type of postoperative pain, spontaneous or provoked, would influence the prognosis of the treatment, since it would supposedly correlate with the severity of the pulpitis. However, in the present study, although the presence of spontaneous preoperative pain was correlated with a lower percentage of success (80%), compared to patients who only showed provoked pain (92.5%), the difference was not significant (p > 0.05). Since spontaneous pain determines the diagnosis of severe pulpitis, according to Wolters et al. classification [51], the same success rate was found in cases of severe pulpitis. No significant correlation was found between the diagnosis according to Wolters et al. [51] classification and the treatment outcome, but the success rate decreased with the severity of the pulpitis. Other study has found significantly less successful outcome in cases of partial pulpotomy with severe pulpitis, compared with mild pulpitis [13]. Studies with larger samples are necessary to definitively determine the correlation between the diagnosis according to Wolters and the outcome of treatment.
Several previous studies have found a relationship between the type of restoration and the result of the treatment [21, 36, 49], but in the present study no influence of the type of restoration has been found. This result is in accordance with that of a systematic review [2] finding that the type of restoration did not significantly affect the success rates of full pulpotomy.
The results of the study that has been carried out show only two factors that significantly influenced the treatment outcome: the type of CSBC and postoperative pain. All four cases of failure occurred in patients in whom Endosequence had been used as a pulp capping material, with a success rate of 82%. However, all cases treated with Biodentine were successful. These results are in accordance with the findings of previous studies. Those in which Biodentine was used, provided success rates greater than 90% [10, 31, 45, 47]. Endosequence has been less investigate as pulp capping material in full pulpotomy, obtaining success rates at 12-months of 93.3% [32] and 77.5% [22].
Regarding the postoperative pain, it was present only in 14% of patients. While postoperative pain is less in pulpotomy than in RCT [29], postoperative pain affect 27%-82% of patients who have undergone full pulpotomy [7, 43]. Taking into account that presence of preoperative pain is the major predictor of postoperative pain [50], the low percentage of patients who felt postoperative pain in the present study may be due to the also low percentage of patients who showed spontaneous preoperative pain. Eghbal et al. [27] observed complete remission of symptoms 24 h following full pulpotomy.
Although the presence of postoperative pain did not correlate with preoperative pain, it was strongly associated to lower success rate of full pupotomy (67%) (Odds ratio = 8.0; 95% C.I. = 0.7 – 95.9; p = 0.047). The ability of postoperative pain to discriminate between cases that will have a good prognosis and those that will fail is high, with a prognostic accuracy of 86%. However, the relationship between postoperative pain and the outcome of full pulpotomy should be analyzed in new studies.
Concerning the response to pulp sensitivity tests, only 10% of cases responded positively to the cold test. This result agrees with what other authors have reported [5]. Well, it is normal to find that teeth with full pulpotomy are unresponsive [24].
Vital pulp therapy procedures, such as full pulpotomy, should be assessed 6 and 12 months postoperatively and at yearly intervals (if necessary) for 4 years thereafter [24]. The follow-up period of the present study, 24-months, is longer than that of other previously published studies [36, 39, 40, 46,47,48, 52, 53], what should be considered a strength. On the contrary, this study has some limitations. Most of the clinical studies carried out to analyze the outcome of full pulpotomy include cases in which treatment was indicated after pulp exposure occurred during caries removal [31, 36, 39, 46, 48]. On the contrary, there are few studies in which, as in the present one, full pulpotomy was performed electively to treat cases diagnosed as irreversible pulpitis [5, 40, 53]. The comparison of the success rates of both types of studies could be criticized, since the indication for treatment is substantially different. However, in the present study, the removal of carious tissue was carried out following the selective removal protocol, without opening the chamber until the carious tissue had been completely removed. On the other hand, the available evidence indicates that the type of pulp exposure treated does not affect the results of pulpotomy [25].
For many years, the AAE criteria [3] on the treatment of irreversible pulpitis led the dentist to ask the patient the choice between RCT and extraction. Without a doubt, this way of proceeding has led to the extraction of a large number of teeth that could have been kept in the mouth using VPT techniques [17, 33]. Uninsured patients, low-income patients, and patients with limited access to specialty care often opted for the extraction of restorable teeth with irreversible pulpitis [8]. In view of the present results, and those of all the clinical studies referenced above, the term “irreversible” can no longer be understood in the sense that the AAE has been using it [6], i.e. that the management of the affected tooth requires RCT or extraction [4]. On the contrary, the diagnosis of "irreversible pulpitis" should be understood as requiring access to the pulp chamber to assess the pulp status and to decide the extent of treatment (pulpotomy or RCT) (Fig. 6), according to what was proposed by Wolters et al. [51].
Conclusions
Elective full pulpotomy using CSBC was a successful choice for the treatment of mature permanent teeth with carious lesions originating symptoms indicative of irreversible pulpitis. It is simpler, less invasive and cheaper than root canal treatment. Postoperative pain could be considered a risk marker for failure of full pulpotomy.
An inverse, but non-significant, correlation was observed between the severity of pulpitis according to the Wolters classification and the treatment success rate. The present results, together with the large amount of scientific evidence accumulated in recent years demonstrating that the erroneously called irreversible pulpitis can be treated by maintaining, totally or partially, pulp vitality, highlights the need to definitively discard the conventional terminology of irreversible pulpitis,or maintain it but modifying its meaning towards the need to access the pulp chamber.
References
Aguilar P, Linsuwanont P (2011) Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod 37:581–587
Alqaderi H, Lee CT, Borzangy S, Pagonis TC (2016) Coronal pulpotomy for cariously exposed permanent posterior teeth with closed apices: a systematic review and meta-analysis. J Dent 44:1–7
American Association of Endodontists (2009) AAE consensus conference recommended diagnostic terminology. J Endodontics 35:1634–1634
American Association of Endodontists (2013) Endodontic diagnosis. Endod: Colleagues Excell, Fall, pp 1–6
Aravind A, Rechithra R, Sharma R et al (2022) Response to pulp sensibility tests after full pulpotomy in permanent mandibular teeth with symptomatic irreversible pulpitis: a retrospective data analysis. J Endod 48:80–86
Asgary S, Eghbal MJ (2023) Challenging the Misnomer of Irreversible Pulpitis and deliberating the Urgent need for reclassification of Pulpal diseases based on the efficacy of vital pulp therapies: an overview of systematic reviews. Iran Endod J 18:202–205
Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S (2013) One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, non-inferiority clinical trial. Clin Oral Invest 17:431–439
Asgary S, Verma P, Nosrat A (2017) Treatment outcomes of full pulpotomy as an alternative to tooth extraction in molars with hyperplastic/irreversible pulpitis: a case report. Iran Endod J 12:261–265
Asgary S, Hassanizadeh R, Torabzadeh H, Eghbal MJ (2018) Treatment outcomes of 4 vital pulp therapies in mature molars. J Endod 44:529–535
Baranwal H, Mittal N, Yadav J, Rani P, Kumar N (2022) Outcome of partial pulpotomy verses full pulpotomy using biodentine in vital mature permanent molar with clinical symptoms indicative of irreversible pulpitis: a randomized clinical trial. J Conserv Dent: JCD 25:317–323
Biddle DA, Morris SB (2011) Using Lancaster’s Mid-P correction to the Fisher’s exact test for adverse impact analyses. J Appl Psychol 96:956–965
Bjørndal L, Demant S, Dabelsteen S (2014) Depth and activity of carious lesions as indicators for the regenerative potential of dental pulp after intervention. J Endod 40:S76–S81
Careddu R, Duncan HF (2021) A prospective clinical study investigating the effectiveness of partial pulpotomy after relating preoperative symptoms to a new and established classification of pulpitis. Int Endod J 54:2156–2172
Careddu R, Plotino G, Cotti E, Duncan HF (2021) The management of deep carious lesions and the exposed pulp amongst members of two European endodontic societies: a questionnaire-based study. Int Endod J 54:366–376
Cisneros-Cabello R, Segura-Egea JJ (2005) Relationship of patient complaints and signs to histopathologic diagnosis of pulpal condition. Aust Endod J 31:24–27
Clarkson JE, Ramsay CR, Mannocci F et al (2022) Pulpotomy for the Management of Irreversible Pulpitis in Mature Teeth (PIP): a feasibility study. Pilot Feasibility Stud 8:77
Crespo-Gallardo I, Hay-Levytska O, Martín-González J et al (2019) Correction: Criteria and treatment decisions in the management of deep caries lesions: Is there endodontic overtreatment? J Clin Exp Dent 11:e103
Cushley S, Duncan HF, Lappin MJ et al (2019) Pulpotomy for mature carious teeth with symptoms of irreversible pulpitis: a systematic review. J Dent 88:103158
Dean AG, Sullivan KM, Soe MM (2013) OpenEpi: open source epidemiologic statistics for public health, versión actualizado 2013/04/06. www.OpenEpi.com. Accedido 2023/05/26
Demant S, Dabelsteen S, Bjørndal L (2021) A macroscopic and histological analysis of radiographically well-defined deep and extremely deep carious lesions: carious lesion characteristics as indicators of the level of bacterial penetration and pulp response. Int Endod J 54:319–330
Demarco FF, Rosa MS, Tarquínio SBC, Piva E (2005) Influence of the restoration quality on the success of pulpotomy treatment: a preliminary retrospective study. J Appl Oral Sci: Rev FOB 13:72–77
Doranala S, Surakanti JR, Vemisetty H, Loka SR, Sudireddy K, Punna R (2021) Comparative assessment of titanium-prepared platelet-rich fibrin, EndoSequence root repair material, and calcium hydroxide as pulpotomy agents in permanent teeth with irreversible pulpitis: a randomized controlled trial. J Conserv Dent: JCD 24:606–610
Duncan HF (2022) Present status and future directions—Vital pulp treatment and pulp preservation strategies. Int Endod J 55(Suppl 3):497–511
Duncan HF, Galler KM, Tomson PL et al (2019) European Society of Endodontology position statement: management of deep caries and the exposed pulp. Int Endod J 52:923–934
Duncan HF, El-Karim I, Dummer PMH, Whitworth J, Nagendrababu V (2023) Factors that influence the outcome of pulpotomy in permanent teeth. Int Endod J 56:62–81
Duncan HF, Kirkevang LL, Peters OA et al (2023) Treatment of pulpal and apical disease: The European Society of Endodontology (ESE) S3-level clinical practice guideline. Int Endod J 56:238–295
Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J (2009) MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J 35:4–8
Elmsmari F, Ruiz XF, Miró Q, Feijoo-Pato N, Durán-Sindreu F, Olivieri JG (2019) Outcome of partial pulpotomy in cariously exposed posterior permanent teeth: a systematic review and meta-analysis. J Endod 45:1296-1306.e3
Galani M, Tewari S, Sangwan P, Mittal S, Kumar V, Duhan J (2017) Comparative evaluation of postoperative pain and success rate after pulpotomy and root canal treatment in cariously exposed mature permanent molars: a randomized controlled trial. J Endod 43:1953–1962
Innes NPT, Frencken JE, Bjørndal L et al (2016) Managing carious lesions: consensus recommendations on terminology. Adv Dent Res 28:49–57
Jassal A, Nawal RR, Yadav S, Talwar S, Yadav S, Duncan HF (2023) Outcome of partial and full pulpotomy in cariously exposed mature molars with symptoms indicative of irreversible pulpitis: a randomized controlled trial. Int Endod J 56:331–344
Kiranmayi T, Vemagiri CT, Rayala C, Chandrappa V, Bathula H, Challagulla A (2022) In vivo comparison of bioceramic putty and mineral trioxide aggregate as pulpotomy medicament in primary molars. A 12-month follow-up randomized clinical trial. Dent Res J (Isfahan) 19:84
León-López M, Cabanillas-Balsera D, Martín-González J, Montero-Miralles P, Saúco-Márquez JJ, Segura-Egea JJ (2022) Prevalence of root canal treatment worldwide: a systematic review and meta-analysis. Int Endod J 55:1105–1127
Li Y, Wang W, Zeng Q et al (2024) Efficacy of pulpotomy in managing irreversible pulpitis in mature permanent teeth: a systematic review and meta-analysis. J Dent 144:104923
Nagendrababu V, Duncan HF, Fouad AF et al (2023) PROBE 2023 guidelines for reporting observational studies in Endodontics: a consensus-based development study. Int Endod J 56:308–317
Ngamthuam I, Manmontri C, Chompu-inwai P, Phinyo P, Nirunsittirat A, Chaipattanawan N (2023) Outcomes of coronal pulpotomy on permanent first molars in children: a retrospective cohort study. Clin Oral Invest 27:7473–7488
Orstavik D, Kerekes K, Eriksen HM, Ørstavik D, Kerekes K, Eriksen HM (1986) The periapical index: a scoring system for radiographic assessment of apical periodontitis. Dent Traumatol 2:20–34
Qudeimat MA, Alyahya A, Hasan AA, Barrieshi-Nusair KM (2017) Mineral trioxide aggregate pulpotomy for permanent molars with clinical signs indicative of irreversible pulpitis: a preliminary study. Int Endod J 50:126–134
Ramani A, Sangwan P, Tewari S, Duhan J, Mittal S, Kumar V (2022) Comparative evaluation of complete and partial pulpotomy in mature permanent teeth with symptomatic irreversible pulpitis: a randomized clinical trial. Int Endod J 55:430–440
Rechithra R, Aravind A, Kumar V, Sharma S, Chawla A, Logani A. Influence of occlusal and proximal caries on the outcome of full pulpotomy in permanent mandibular molar teeth with partial irreversible pulpitis: A prospective study. Int Endod J. 2021 Oct;54(10):1699-1707.
Ricucci D, Loghin S, Siqueira JF (2014) Correlation between clinical and histologic pulp diagnoses. J Endod 40:1932–1939
Ryan T (2013) Methods of determining sample sizes. In: John Wiley & Sons I (ed) Sample size determination and power, Firstedn. John Wiley & Sons, Inc, pp 17–55
Simon S, Perard M, Zanini M et al (2013) Should pulp chamber pulpotomy be seen as a permanent treatment? Some preliminary thoughts. Int Endod J 46:79–87
Taha NA, Abdelkhader SZ (2018) Outcome of full pulpotomy using Biodentine in adult patients with symptoms indicative of irreversible pulpitis. Int Endod J 51:819–828
Taha NA, Abdulkhader SZ (2018) Full pulpotomy with biodentine in symptomatic young permanent teeth with carious exposure. J Endod 44:932–937
Taha NA, Ahmad MB, Ghanim A (2017) Assessment of Mineral Trioxide Aggregate pulpotomy in mature permanent teeth with carious exposures. Int Endod J 50(2):117–125
Taha NA, Al-Rawash MH, Imran ZA (2022) Outcome of full pulpotomy in mature permanent molars using 3 calcium silicate-based materials: a parallel, double blind, randomized controlled trial. Int Endod J 55:416–429
Taha NA, Abuzaid AM, Khader YS (2023) A randomized controlled clinical trial of pulpotomy versus root canal therapy in mature teeth with irreversible pulpitis: outcome, quality of life, and patients’ satisfaction. J Endod 49:624-631.e2
Tan SY, Yu VSH, Lim KC et al (2020) Long-term pulpal and restorative outcomes of pulpotomy in mature permanent teeth. J Endod 46:383–390
Torabinejad M, Cymerman JJ, Frankson M, Lemon RR, Maggio JD, Schilder H (1994) Effectiveness of various medications on postoperative pain following complete instrumentation. J Endod 20:345–354
Wolters WJ, Duncan HF, Tomson PL et al (2017) Minimally invasive endodontics: a new diagnostic system for assessing pulpitis and subsequent treatment needs. Int Endod J 50:825–829
Zhang M, Xiong Y, Wang X et al (2022) Factors affecting the outcome of full pulpotomy in permanent posterior teeth diagnosed with reversible or irreversible pulpitis. Sci Rep 12:1–9
Zhu X, Zhang Y, Wang J et al (2023) Effect of full pulpotomy using a calcium silicate–based bioactive ceramic in adult permanent teeth with symptoms indicative of irreversible pulpitis: a retrospective study. J Am Dent Assoc 154:486–494
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not- for- profit sectors.
Funding
Funding for open access publishing: Universidad de Sevilla/CBUA. This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, J.J.S-E., J.M-G., and D.C-B.; Data curation, C.J-M., P.M-M., and J.J.S-E.; Formal analysis, J.J.S-E., J.M-G., P.M-M., and D.C-B.; Investigation, C.J-M., I.C-G., and J.J.S-E.; Methodology, J.J.S-E., C.J-M., and D.C-B.; Supervision, J.J.S-E., and D.C-B.; Validation, J.J.S-E., and D.C-B.; Writing – original draft, J.J.S-E., J.M-G., I.C-G., and D.C-B.; Writing – review & editing, J.J.S-E., D.C-B., C.J-M., I.C-G., P.M-M., and J.M-G.
Corresponding authors
Ethics declarations
Human ethics and consent to participate
The Ethics Committee of the institutional review board of the University of Sevilla approved our retrospective study (protocol number 2024–1209). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients included in the study had given their informed consent so that data from their medical history could be used in research.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiménez-Martín, C., Martín-González, J., Crespo-Gallardo, I. et al. Elective full pulpotomy in mature permanent teeth diagnosed with symptomatic irreversible pulpitis: a two years retrospective study. Clin Oral Invest 28, 421 (2024). https://doi.org/10.1007/s00784-024-05814-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05814-z