Abstract
Background and objective
Psychological stress has been identified in some observational studies as a potential factor that may modify and affect periodontal diseases, but there are no similar data for peri-implantitis. The aim of this study was to determine the relationship between interleukin (IL)-1β, IL-6, IL-10, interferon (IFN)α inflammatory cytokines and the psychological stress-related markers, glucocorticoid receptor-α (GRα), and salivary α-amylase (sAA) gene expression levels in saliva samples obtained from healthy implants and peri-implantitis patients.
Materials and methods
The study included a total of 50 systemically healthy subjects. Peri-implant clinical parameters were recorded and psychological stress level was evaluated with the hospital anxiety and depression scale (HAD) and state-trait anxiety inventory (STAI) questionnaire forms. Following the evaluations, the patients were divided into 4 groups according their stress and clinical status (Ia, Ib, IIa, IIb). IL-1β, IL-6, IL-10, IFNα, GRα, sAA gene expression levels in the saliva samples were quantified by quantitative polymerase chain reaction (qPCR).
Results
In the group of peri-implantitis who had a high score in stress level assessment scales, significantly higher IL-1β, IL-6, sAA expression levels were observed (p < 0.001). The IL-10 gene expression levels were lower in the groups with a high score in the stress level assessment scales (p < 0.001). GRα gene was expressed at lower levels in the group of peri-implantitis who had a high score in stress level assessment scales but the difference was not statistically significant (p = 0.065).
Conclusion
The study findings suggest that psychological stress may increase the inflammation associated with peri-implantitis by affecting cytokine expression levels.
Clinical relevance
To prevent peri-implantitis or reduce its prevalence, it could be beneficial to evaluate stress levels and identify individuals experiencing stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An imbalance among bacterial load and host response results in peri-implant diseases [1]. Peri-implant diseases may affect peri-implant mucosa alone (peri-implant mucositis) or both peri-implant mucosa and supporting bone (peri-implantitis) [2]. Peri-implantitis and peri-implant mucositis are differentiated by the match around the teeth; periodontitis and gingivitis. Both periodontitis and peri-implantitis have common features in terms of clinical features, etiology, pathogenesis, therapy and risk factors [3]. Studies have shown that the major risk factors for periodontal disease, such as poor oral hygiene and tobacco consumption, also represent risk indicators for peri-implantitis. Diabetes, alcohol consumption, and genetic traits have also been suggested as risk factors for peri-implantitis [3, 4]. Stress, depression and anxiety have been identified in some observational studies as potential factors that may modify and affect periodontal diseases [5, 6], but there are no similar data for peri-implantitis.
Changes in psychological conditions, the emergence of depression and stress factors can affect oral hygiene, smoking or alcohol consumption habits indirectly and can increase microbial dental plaque accumulation. Thus, individuals become more susceptible to unhealthy conditions. These factors may also alter the host immune response and can directly affect periodontal health [7].
Investigations have explained that psychological stress promotes the hypothalamus–pituitary–adrenal (HPA) axis activation, after which corticotrophin-releasing hormone (CRH) is secreted from the hypothalamus. Subsequently, adrenocorticotropic hormone (ACTH) release is stimulated from the pituitary gland and finally glucocorticoid secretions increase from the adrenal cortex [7, 8]. Glucocorticoids can inhibit immunoglobulin (Ig)A secretion, which can lead to a response in the immune system, cytokine expression and colonization of periodontal pathogens, and inhibit IgG secretion, which can allow pathogens to be recognized and phagocytized by neutrophils [7, 9, 10].
Glucocorticoid hormones exhibit their effects by binding to glucocorticoid receptors (GRs) [11]. GRs, members of the superfamily of nuclear receptors, bind glucocorticoids in cytoplasm and act as a transcription factor, inhibiting both CRH and ACTH secretion and synthesis. They play a critical role in the regulation of HPA axis feedback mechanisms and in stress adaptation [12, 13]. GRs have been identified in two isoforms: GRα, and GRβ. GRα binds glucocorticoids and mediates glucocorticoid effects but GRβ is unable to bind glucocorticoids [14, 15].
Another biological marker, which has been proposed to be sensitive to stress-associated changes, is salivary α-amylase (sAA). Stimulation of the autonomic nervous system (ANS) that controls the salivary glands results in release of sAA. It is known that sAA plays a role in the digestion of starch and has an inhibitory function against micro-organisms, but at the same time increases corresponding to the response of the sympathetic nervous system (SNS) to both psychological and physical stressors [16, 17].
Although the first step of peri-implant disease pathogenesis is related to micro-organisms, the immuno-inflammatory response with pro- and anti-inflammatory cytokines plays an important role in disease progression [18]. The pro- and anti-inflammatory cytokine balance determines the severity of inflammatory diseases [19], and this local host response to bacterial biofilm is in immunological and biochemical aspect, which is very similar in both periodontal and peri-implant diseases [20].
In clinical practice, peri-implant conditions are assessed through clinical indices such as probing depth, bleeding on probing, suppuration, and their combination with radiographic bone [21, 22]. Nevertheless, variables like probing orientation, the configuration of prosthetic structures, and tissue biotype can impact the outcomes of clinical assessments. At the same time, these clinical diagnostic tools provide information about the present inflammation status, but does not provide adequate prediction of the activity and severity of tissue destruction. To ensure diagnostic clarity, implantology calls for innovative diagnostic approaches such as the assessment of inflammatory biomarkers within biological fluids. Thus many studies evaluated the activity of systemic diseases, periodontal and peri-implant diseases or treatment efficacy with host derived proteins in saliva but to the best of our knowledge, no study has evaluated the psychological stress-related markers of peri-implantitis patients. Thus, the aim of this study was to determine the relationship between interleukin (IL)-1β, IL-6, IL-10, interferon (IFN)α inflammatory cytokines and the psychological stress-related markers, glucocorticoid receptor-α (GRα), and sAA gene expression levels in saliva samples obtained from healthy implants and peri-implantitis patients.
Materials and methods
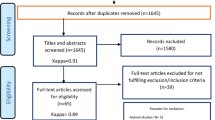
Patient population
The study included a total of 50 systemically healthy subjects (16 females, 34 males aged 23 to 72 years) who were treated at Gazi University Department of Periodontology, Ankara, Turkey. The selected patients were informed regarding the details of the research and signed informed consent forms were received. This study was approved by the human subjects ethics board of Ankara University, Faculty of Dentistry (Protocol ID: 36290600/51) and was conducted in accordance with the Helsinki Declaration.
Inclusion and exclusion criteria
This cross-sectional study included systemically healthy, partially edentulous subjects who had an implant-supported restoration functioning for at least two years. The cases were defined as peri-implantitis and healthy implants using the criteria in the consensus report of workgroup 4 of the 2017 World Workshop [23]. Peri-implantitis was defined as bleeding on probing (BOP) or suppuration, and increased pocket depth associated with radiographic bone loss. Healthy patients had no clinical signs of inflammation, BOP, suppuration, erythema or swelling.
Exclusion criteria were as follows for all groups: (1) non-surgical/ surgical periodontal or peri-implant therapy within the previous 6 months, (2) presence of periodontitis (i.e., suppuration and/or BOP in > 30% of the subgingival sites or any dental site with probing depth [PD] ≥ 4 mm), and localized (BOP ≥ 10% and ≤ 30%) or generalized (BOP > 30%) gingivitis (3) pregnancy (4) bruxism (5) antibiotics or anti-inflammatory medication usage within 6 months before the clinical examination, (6) regular intake of anticonvulsant, immunosuppressive, calcium channel blockers, antipsychotic/antidepressant drugs, (7) smoking.
Clinical examinations
The same clinician recorded all the clinical examinations using a 0.5 mm Williams-type periodontal probe from the four sides of each implant (mesial, buccal, distal, lingual/palatal). The peri-implant clinical measurements were recorded as follows for each implant side: (1) pocket depth (PD), the distance between the gingival margin and the bottom of a peri-implant pocket (2) modified plaque index (mPI) [24], (3) modified gingival index (mGI) [24], (4) bleeding on probing (BOP).
Questionnaire
The psychological stress level was evaluated with the hospital anxiety and depression scale (HAD) and state- trait anxiety inventory (STAI) questionnaire forms. The HAD scale is designed to measure the risk, level or severity of anxiety and depression in patients. The scale consists of two sub-scales, each with 7 items, assessing both anxiety (HAD-A) and depression (HAD-D) at the same time. The validity and reliability study of the questionnaire in Turkish was conducted by Aydemir [25]. The cut-off scores of the Turkish scale were calculated as 10/11 for the HAD-A sub-scale, and 7/8 for the HAD-D sub-scale. According to these results, patients with a score above the cut-off point are considered at risk for anxiety or depression.
The STAI questionnaire is composed of two sub-scales, each consisting of 20 items, which can measure state (STAI-I) and trait (STAI-II) of anxiety. Oner and Le Compte conducted the validity and reliability studies of the questionnaire in Turkish [26]. Scores can range from 20 to 80, higher scores indicates greater anxiety, and ≥ 40 indicates clinical symptoms of anxiety [27, 28]. Groups were divided into “a” or “b’’ according to the cut-off points of the stress level assessment scales (HAD-A ≥ 11, HAD-D ≥ 8, STAI-I ≥ 40, STAI-II ≥ 40).
The study participants were divided into four groups: patients with healthy implant and a score above the cut-off value of the stress level assessment scales (Group Ia, n = 16) or a score below the cut-off value of the stress level assessment scales (Group Ib, n = 9); patients with peri-implantitis and a score above the cut-off value of the stress level assessment scales (Group IIa, n = 15), and those with a score below the cut-off value of the stress level assessment scales (Group IIb, n = 10).
Saliva sampling
All saliva samples were collected between 08.00 am -10.00 am to avoid circadian rhythm changes. Participants were instructed not to consume any nutrients or liquid for at least 1 h prior to sampling, and atraumatic brushing should be done 1 h before sampling. Then unstimulated whole saliva was collected into propylene collection tubes. If there was any blood or foreign substance in the collection tube, the sampling was repeated. Immediately after the appropriate collection of the saliva samples, they were stored in the RNAlater® (Sigma-Aldrich, Germany) to avoid RNA degradation. The samples were incubated at 4 °C for 24 h and then stored at -80 °C until RNA extraction.
RNA extraction and reverse transcription
Saliva were put in a tube and subsequently, the IL-1β, IL-6, and IL-10, IFNα, GRα, sAA mRNA levels were evaluated. Gene expression levels of beta-actin (β-actin) were used as a reference. Total RNA was extracted from respective saliva samples using the TriPure isolation kit (Roche, Germany) under the manufacturer’s recommendation. RNA was suspended in diethylpyrocarbonate-treated water, DNAse-treated (Turbo DNA-free; Ambion Inc.), and stored at 70 °C until use. RNA concentrations were determined by the microvolume spectrophotometer (Nanodrop 1000; Nanodrop Technologies LLC, Wilmington, NC, USA). Afterward, 1 μg of total RNA was used to synthesize cDNA using the first-strand cDNA synthesis kit (Roche Diagnostics Co., Indianapolis, USA) as described by the manufacturer.
The housekeeping gene of β-actin was used as control by performing with both in-house PCR and qPCR methods. 2X SYBR Green dye with (10pmol/ μl) forward (F1) primer (0,5pmol/ μl) reverse (R1) primer (0,5pmol/μl), dionised water (4 μl) and cDNA (5 μl) were added and the final volume was adjusted to 20 μl.
Real-time PCRs
The primers used to amplify mRNA corresponding to the IL-1β, IL-6, and IL-10, IFNα, GRα, sAA sequences for quantitative PCR analysis were designed using the Light Cycler probe design software (Roche Diagnostics GmbH, Mannheim, Germany). The primer sequences, the amplification profiles, and amplicon length are described in Table 1.
Quantitative PCR (qPCR) was carried out using the LightCycler System (Roche Diagnostics GmbH) as recommended by the manufacturer (FastStart DNA MasterPLUS SYBR Green; Roche Diagnostics Co., Indianapolis, IN, USA). Results were expressed as relative quantification to the β-actin gene expression levels.
qPCR stages were performed on LightCycler® Nano (Roche, Germany) with the denaturation (950C, 600 s), cycling: 95oC 10 s 60oC 10 s., annealing 72oC 30 s for 40 cycles, then cooling with 40oC 600 s. The calculations were done according to the control gene expressions of the housekeeping gene of β-actin. Quantitations were performed by using LightCycler® Nano Software 1.1 and the data of the expressions of the chosen genes in the study were calculated according to the 2(-∆∆Ct) method.
Statistical analysis
Given the absence of similar studies in the literature, the sample size was determined based on the effect size. Assuming an effect size of 0.5 for the difference in IL-1β expression level changes among the groups (Ia-IIa, Ia-IIb, Ib-IIa, and Ib-IIb), a sample size calculation was performed using a One Way ANOVA test with a power of 0.80 and a significance level of 0.05. The analysis indicated that a minimum sample of 48 individuals would be sufficient for the study.
Analyses were performed using SPSS for Windows 11.5 software program. (SPSS Inc., Chicago, IL, USA). The compatibility of data with normal distribution was examined graphically and with the Kolmogorov-Smirnov test. Data are presented as mean ± standard deviation for normally distributed continuous variables, median (minimum-maximum) for non-normally distributed continuous variables and count, percentages for categorical variables. In the examination of a statistically significant difference between the categories of a qualitative variable with two categories in terms of a quantitative variable, the Student’s t-test was used if the normal distribution assumption was met; otherwise the Mann-Whitney U test was used. In the examination of a statistically significant difference between the categories of a qualitative variable with more than two categories in terms of a quantitative variable, the One Way ANOVA test was used if the normal distribution assumption was met, otherwise the Kruskal Wallis H test was used. The Chi-Square test was applied to compare the relationship between qualitative variables. p value < 0.05 was considered statistically significant.
Results
Peri-implant clinical parameters were recorded and saliva samples were obtained from a total of 50 patients. The clinical variables are presented in Table 2, and all groups were well matched. Peri-implant clinical examinations datas and questionnaire scores of the study groups are presented in Table 3. In both the IIa and IIb groups, mGI, mPI, BOP and PD data were significantly higher compared with group Ia and group Ib (p < 0.001). There were no significant differences between groups Ia and Ib, or between group IIa and group IIb. In terms of the mean age and functional loading times of the implants, no significant difference was observed between all the compared groups.
There was a statistically significant difference among the groups Ia, Ib, IIa, IIb in terms of HAD-A variable (p < 0.001). After Bonferroni correction was applied to the subgroups that showed significance, the Mann Whitney U test was used. Binary groups with a significant difference were found to be Ia-IIb, IIa-IIb and Ib-IIa (p = 0.015, p = 0.001, p = 0.034). There was a statistically significant difference between the groups Ia, Ib, IIa, IIb in respect of the HAD-D variable (p < 0.001). Bonferroni correction was applied to the subgroups with significance and the Mann Whitney U test was used. Significant differences were determined between the groups Ia-IIb and IIa-IIb (p = 0.001, p < 0.001).
A statistically significant difference was found between groups Ia, Ib, IIa, IIb in terms of STAI-I (p < 0.001). The groups showing significance were found to be Ia-Ib, Ia-IIb, Ib-IIa and IIa-IIb when they were examined with the Tukey Post Hoc test (p < 0.001, p < 0.001, p = 0.001, p < 0.001). In respect of the STAI-II variable, there was a significant difference between all the groups (p < 0.001). The Mann Whitney U test was used after Bonferroni correction was applied to the subgroups with significance. Binary groups with significant results were found to be IIa-IIb, IIb-Ia, Ib-IIa and Ia-Ib (p < 0.001, p < 0.001, p = 0.008, p = 0.003).
The gene expression levels for each biological marker in all the groups are shown in Fig. 1. IL-1β and IL-6 expressions were significantly higher in group IIa compared with group IIb (p < 0.001). IFNα gene expression was similar in groups IIa and IIb. IL-10 gene expression was significantly lower in group IIa than in group IIb (p < 0.001). IL-1β gene expression was significantly higher in group Ia than in group Ib. IL-6 and IFNα gene expressions were similar in groups Ia and Ib. IL-10 gene expressions were significantly lower in group Ia compared to group Ib (p < 0.001).
In respect of sAA gene expressions in saliva samples, there was significantly higher expression in group IIa compared with group IIb (p < 0.001), and in group Ia compared to group Ib (p < 0.001). GRα gene expressions were significantly higher in group Ib than in group Ia (p < 0.001). GRα gene was expressed at lower levels in group IIa than in group IIb but the difference was not statistically significant (p = 0.065). When the participants were divided according to the stress level assessment scores, regardless of peri-implant health or disease status, group (Ia + IIa) was determined to have significantly lower GRα gene expression values than group (Ib + IIb).
Discussion
In this study, the association between inflammatory cytokine levels and stress-related biomarkers was examined in order to evaluate the effect on peri-implantitis and peri-implant health of psychological stress, which is known to significantly affect quality of life and cause the development of many diseases.
The identification of biomarkers that play a role in the pathogenesis of peri-implantitis allows for a better understanding of the pathophysiological mechanism of the disease and allows evaluation of the immune status of the organism. Previous investigations have reported that pro-inflammatory cytokines and chemokines play a role in the early and advanced stages of peri-implant disease, leading to the process of inflammation and tissue destruction [19]. Schierano et al. showed that pro- and anti-inflammatory cytokines were released at varying levels at 4, 8, and 12 months after implant placement. This change in cytokine levels is explained by the attempts to stabilize the immune-inflammatory balance in peri-implant tissues after implant surgery [29]. In the current study, the implants of all participants had been functioning for at least 24 months and the mean duration of function was 5.58 years.
Saliva, known for its low cost, easy handling, usually available for sampling in large quantities and the presence of various biomarkers, including genomic material (mRNA, DNA) and proteins, offers notable advantages over other peri-implant fluids. The genomic material in its content is stable and in sufficient amounts for utilization in PCR procedures. In comparison to other fluids such as serum and peri-implant crevicular fluid, it offers an easy solution for storage, necessitates less technical precision and equipment during the collection process. Numerous studies use peri-implant sulcular fluid (PISF) as the preferred medium for assessing biomarkers in peri-implantitis patients [30, 31]. However, this methodology is technique-sensitive and demands a complicated toolkit. On the other hand, collecting saliva is a relatively straightforward technique that doesn’t necessitate extensive training when compared to obtaining PISF samples. Additionally, saliva sample collection is a fast and noninvasive method, which does not cause stress as blood collection may do [32]. Psychological stress-related studies have indicated that samples should be collected without activating any local reflex mechanisms [33]. In the light of this information, an unstimulated whole saliva collection protocol was applied in this study.
There are numerous studies evaluating the biomarkers that change due to peri-implant tissue inflammation in saliva samples [34,35,36]. Peri-implantitis has been linked to elevated salivary concentrations of IL1β [34, 35, 37]. IL6, and IL10 [35, 37], and these interleukins have been suggested as potential valuable indicators for the early detection and monitoring of this condition.
In the current study, HAD-A, HAD-D, STAI-I and STAI-II scales were used to determine the participants’ stress levels. These scales were used in many studies in which stress and anxiety were measured in dentistry. The validity and reliability of these questionnaires for Turkish population were tested before [25, 26]. These questionnaires, which the participants themselves have read and answered, eliminate the possibility that the researcher may affect or direct the participant [38].
The 2017 World Workshop on Periodontology report pointed out that stress is one of the environmental factors involved in periodontal breakdown [39]. There are studies showing that factors such as smoking, poor oral hygiene, diabetes, and genetic characteristics are risk factors for periodontal and peri-implant diseases and that psychological stress can also be a risk factor for periodontal disease [7, 40, 41]. However, to the best of our knowledge, there is no study in literature similar to the current research, which investigated the relationship between peri-implantitis and psychological stress.
Depression is one of the most common psychological disorders and studies have shown positive correlations with chronic inflammatory diseases such as autoimmune disease, inflammatory bowel diseases and allergies. This positive relationship is thought to be not only because of the depressive nature of chronic diseases, but also due to higher inflammatory cytokine expressions under these conditions [42]. According to recent opinions, depression does not develop due to a single neural network connection, but with multiple neural networks involving neurotransmitters, which function in the transmission of environmental stimuli to the brain, particularly stress [43]. Stressful life events affect and depress the immune system of subjects who then show depressive symptoms. Paik et al. investigated the effect of academic stress on the immune system and showed elevated levels of IL-1β, IL-6, and IL-10 [44]. These results are consistent with the current study results for IL-1β and IL-6 expression levels, although in our study, the IL-10 expression levels were lower in the groups with a high score in the stress level assessment scales. These IL-10 expression level values are consistent with the results of a study by Dhabhar et al. [45]. They evaluated pro- and anti-inflammatory cytokine concentrations in depressive patients and showed that IL-10 levels were statistically lower in depressive patients and IL-6 levels were higher but not at a statistically significant level in depressive patients. In healthy conditions, higher levels of IL-6 induce IL-10 expressions due to their anti-inflammatory and immune-regulatory effects but according to the study results, the inducing effects were seen at low levels in depressive patients [45]. In the current study, the groups with high scores in the stress level assessment scales, such as Ia and IIa, showed statistically lower IL-10 levels than groups Ib and IIb and IL-6 expression levels were statistically higher in group IIa than in group IIb.
Interferons are known as a large cytokine family that has antiviral, antitumor, anti-proliferative and immune-modulatory effects. IFNα, also known as type I interferon, is expressed by type 1 T helper cells and by fibroblasts against viral and bacterial stimuli. IFNgama(γ), known as type II interferon, has more powerful effects on immune system modulation and studies related to periodontal diseases have evaluated IFNγ much more than IFNα [46]. Recent studies have indicated that IFNα is a multifunctional cytokine, which causes anti-inflammatory cytokine activation and pro-inflammatory cytokine inhibition [47]. Wright et al. evaluated IFNα expressions in periodontitis patients and found elevated IFNα levels related with periodontal infection, suggesting that IFNα may play a role in periodontal disease pathogenesis [46]. The current study results demonstrated statistically significant higher levels of IFNα gene expression in group Ia than in group IIa, and in group Ib than in group IIb. Th1 cells are responsible for the cell-mediated immune response and producing IFNα, so the elevation in IFNα levels in the healthy groups of the current study may support the data that cell-mediated immune response is low level in peri-implantitis patients [48].
sAA is a notable protein of saliva that plays a role in the host response by acting as an inhibitory factor against micro-organisms. Sánchez et al. showed that the sympathetic system is activated by the inflammatory process in periodontitis and upregulates sAA to increase the salivary defence potential [48]. Consistent with the knowledge that sAA may be an indicator of the SNS, it has been also reported that sAA can be released in response to psychosocial stress. The results of the current study support this view as the sAA expressions were determined to be higher in groups Ia and IIa compared to groups Ib and IIb.
Previous studies have shown that inflammation and environmental factors such as stress affect GR functions in a negative way and cause glucocorticoid resistance in the organism [49, 50]. In an experimental animal study, GRα gene expressions were decreased with stress elevation and showed that stress may exacerbate the periodontitis progression mechanism. The current study results for GRα gene expression were similar, with significantly lower GRα gene expressions in group Ia than in group Ib, and although there was no statistically significant difference between groups IIa and IIb, lower GRα gene expression was observed in group IIa. When the participants were compared according to stress levels exclusively, group (Ia + IIa) showed significantly lower GRα gene expression values than group (Ib + IIb). Nevertheless, additional studies are necessary to confirm these findings, and determine whether GRα may be assessed in saliva as a stress-related marker in the same way as cortisol. To the best of the authors’ knowledge, the present study is the first study that assesses stress-related markers and inflammatory cytokines in saliva samples of peri-implantitis patients by using qPCR. Small sample size and lack of the analyzing of markers expression at protein level could be limitations of this cross-sectional study. Therefore, there is a need for further studies to correlate between the markers expression at protein levels with mRNA levels for better understanding of stress role in peri-implantitis pathogenesis.
Conclusions
The aim of current study was to evaluate inflammatory cytokines and psychological stress with its related markers in peri-implantitis patients compared to individuals with healthy implants.
The findings obtained from this study indicate that stress may increase the inflammation associated with peri-implantitis, and in healthy individuals, stress alone is not sufficient to cause inflammation but may increase the susceptibility to inflammation by affecting cytokine expression levels. For the prevention of peri-implantitis or to reduce the prevalence, it could be useful to assess stress levels, identify individuals with stress and make these patients aware of their stress levels and even to take a multidisciplinary treatment approach guided by professional psychological support when necessary. However, there is a need for further investigations to be able to better understand the role of psychological stress in the pathogenesis of peri-implantitis.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Valente NA, Andreana S (2016) Peri-implant disease: what we know and what we need to know. J Periodontal Implant Sci 46:136–151
Zitzmann NU, Berglundh T (2008) Definition and prevalence of peri-implant diseases. J Clin Periodontol 35:286–291
Heitz-Mayfield LJ, Lang NP (2010) Comparative biology of chronic and aggressive periodontitis vs. peri‐implantitis. Periodontol 2000 53(1):167–181
Lindhe J, Meyle J (2008) Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J Clin Periodontol 35:282–285
Vettore MV, Leão ATT, Monteiro Da Silva AM, Quintanilha RS, Lamarca GA (2003) The relationship of stress and anxiety with chronic periodontitis. J Clin Periodontol 30(5):394–402
Genco RJ, Ho AW, Grossi SG, Dunford RG, Tedesco LA (1999) Relationship of stress, distress, and inadequate coping behaviors to periodontal disease. J Clin Periodontol 70(7):711–723
Genco RJ, Ho AW, Kopman J, Grossi SG, Dunford RG, Tedesco LA (1998) Models to evaluate the role of stress in periodontal disease. Ann Periodontol 3(1):288–302
Tsigos C, Chrousos GP (2002) Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. J Psychosom Res 53(4):865–871
Peruzzo DC, Benatti BB, Ambrosano GM, Nogueira-Filho GR, Sallum EA, Casati MZ et al (2007) A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol 78(8):1491–1504
Williams T (1990) Effect of glucocorticosteroids on microvascular permeability. Am Rev Respir Dis 141:39–43
Nicolaides NC, Galata Z, Kino T, Chrousos GP, Charmandari E (2010) The human glucocorticoid receptor: molecular basis of biologic function. Steroids 75(1):1–12
Lupien SJ, McEwen BS, Gunnar MR, Heim C (2009) Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 10(6):434
Juruena MF, Cleare AJ, Pariante CM (2004) The hypothalamic pituitary adrenal axis, glucocorticoid receptor function and relevance to depression. Braz J Psychiatry 26(3):189–201
Matsubara T, Funato H, Kobayashi A, Nobumoto M, Watanabe Y (2006) Reduced glucocorticoid receptor α expression in mood disorder patients and first-degree relatives. Biol Psychiatry 59(8):689–695
Oakley RH, Jewell CM, Yudt MR, Bofetiado DM, Cidlowski JA (1999) The dominant negative activity of the human glucocorticoid receptor β isoform specificity and mechanisms of action. J Biol Chem 274(39):27857–27866
Nater UM, Rohleder N (2009) Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology 34(4):486–496
Sánchez GA, Miozza V, Delgado A, Busch L (2011) Determination of salivary levels of mucin and amylase in chronic periodontitis patients. J Periodontal Res 46(2):221–227
Mardegan GP, Shibli JA, Roth LA, Faveri M, Giro G, Bastos MF (2017) Transforming growth factor-β, interleukin‐17, and IL‐23 gene expression profiles associated with human peri‐implantitis. Clin Oral Implants Res 28(7):e10–e15
Petković-Ćurčin A, Matić S, Vojvodić D, Stamatović N, Todorović T (2011) Cytokines in pathogenesis of peri-implantitis. Vojnosanit Pregl 68(5):435–440
Uitto VJ (2003) Gingival crevice fluid–an introduction. Periodontol 2000 31(1):9–11
Heitz-Mayfield LJ (2008) Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 35(8 Suppl):292–304
Renvert S, Persson GR, Pirih FQ, Camargo PM (2018) Peri-implant health, peri‐implant mucositis, and peri‐implantitis: case definitions and diagnostic considerations. J Clin Periodontol 45(Suppl 20):S278–S285
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E et al (2018) Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol 45(Suppl 20):S286–S291
Mombelli A, Van Oosten MAC, Schürch E Jr, Lang NP (1987) The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol 2(4):145–151
Anksiyete AÖH (1997) Depresyon Ölçeği Türkçe formunun geçerlilik ve güvenilirlik çalışması. Turk Psikiyatri Derg 8(4):280–287
Oner N, Le Compte A Durumluk-Surekli kaygi envanteri el kitabi. Istanbul: Boğaziçi Yayinları 1985
Spielberger CD, Gorsuch RL (1983) State-trait anxiety inventory for adults: manual and sample: Manual, instrument and scoring guide. Consulting Psychologists
Addolorato G, Ancona C, Capristo E, Graziosetto R, Di Rienzo L, Maurizi M, et al (1999) State and trait anxiety in women affected by allergic and vasomotor rhinitis. J Psychosom Res 46:283–289.
Schierano G, Bellone G, Cassarino E, Pagano M, Preti G, Emanuelli G (2003) Transforming growth Factor-β and interleukin 10 in oral implant sites in humans. J Dent Res 82(6):428–432
Fonseca FJ, Moraes Junior M, Lourenco EJ, Teles Dde M, Figueredo CM (2014) Cytokines expression in saliva and peri-implant crevicular fluid of patients with peri-implant disease. Clin Oral Implants Res 25(2):e68–e72
Duarte PM, Serrão CR, Miranda TS et al (2016) Could cytokine levels in the peri-implant crevicular fluid be used to distinguish between healthy implants and implants with peri‐implantitis? A systematic review. J Periodontal Res 51(6):689–698
Akcali A, Huck O, Tenenbaum H, Davideau JL, Buduneli N (2013) Periodontal diseases and stress: a brief review. J Oral Rehabil 40(1):60–68
Bosch JA, Veerman EC, de Geus EJ, Proctor GB (2011) α-Amylase as a reliable and convenient measure of sympathetic activity: don’t start salivating just yet! Psychoneuroendocrinology 36(4):449–453
Rocha FS, Jesus RN, Rocha FM, Moura CC, Zanetta-Barbosa D (2014) Saliva versus peri-implant inflammation: quantification of IL-1β in partially and totally edentulous patients. J Oral Implantol 40(2):169–173
Liskmann S, Vihalemm T, Salum O, Zilmer K, Fischer K, Zilmer M (2006 Jul-Aug) Correlations between clinical parameters and interleukin-6 and interleukin-10 levels in saliva from totally edentulous patients with peri-implant disease. Int J Oral Maxillofac Implants 21(4):543–550
Liskmann S, Vihalemm T, Salum O, Zilmer K, Fischer K, Zilmer M (2007) Characterization of the antioxidant profile of human saliva in peri-implant health and disease. Clin Oral Implants Res 18(1):27–33
Abduljabbar T, Vohra F, Ullah A, Alhamoudi N, Khan J, Javed F (2019) Relationship between self-rated pain and peri-implant clinical, radiographic and whole salivary inflammatory markers among patients with and without peri-implantitis. Clin Implant Dent Relat Res 21(6):1218–1224
Solis ACO, Lotufo RFM, Pannuti CM, Brunheiro EC, Marques AH, Lotufo-Neto F (2004) Association of periodontal disease to anxiety and depression symptoms, and psychosocial stress factors. J Clin Periodontol 31(8):633–638
Lang NP, Bartold PM (2018) Periodontal health. J Periodontol 89:9–16
Rai B, Kaur J, Anand SC, Jacobs R (2011) Salivary stress markers, stress, and periodontitis: a pilot study. J Periodontol 82(2):287–292
Monteiro da Silva AM, Oakley DA, Newman HN, Nohl FS, Lloyd HM (1996) Psychosocial factors and adult onset rapidly progressive periodontitis. J Clin Periodontol 23(8):789–794
Rook GAW, Lowry CA (2009) The hygiene hypothesis and affective and anxiety disorders. In: Rook GAW, (eds). The hygiene hypothesis and Darwinian medicine. Progress in Inflammation Research; Birkhäuser Basel; 2009:189–220
Stone EA, Lin Y, Quartermain D (2008) A final common pathway for depression? Progress toward a general conceptual framework. Neurosci Biobehav Rev 32(3):508–524
Paik IH, Toh KY, Lee C, Kim JJ, Lee SJ (2000) Psychological stress may induce increased humoral and decreased cellular immunity. Behav Med 26(3):139–141
Dhabhar FS, Burke HM, Epel ES, Mellon SH, Rosser R, Reus VI et al (2009) Low serum IL-10 concentrations and loss of regulatory association between IL-6 and IL-10 in adults with major depression. J Psychiatr Res 43(11):962–969
Wright HJ, Matthews JB, Chapple IL, Ling-Mountford N, Cooper PR (2008) Periodontitis associates with a type 1 IFN signature in peripheral blood neutrophils. J Immunol 181(8):5775–5784
Benveniste EN, Qin H (2007) Type I interferons as anti-inflammatory mediators. Sci STKE 2007(416):pe70–pe70
Mathur A, Michalowicz B, Castillo M, Aeppll D (1996) Interleukin-1 alpha, interleukin‐8 and interferon‐alpha levels in gingival crevicular fluid. J Periodontal Res 31(7):489–495
Pace TW, Hu F, Miller AH (2007) Cytokine-effects on glucocorticoid receptor function: relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun 21(1):9–19
Marques AH, Silverman MN, Sternberg EM (2009) Glucocorticoid dysregulations and their clinical correlates. Ann N Y Acad Sci 1179(1):1–18
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). This study was supported by a grant from board of Gazi University Projects of Scientific Investigation (grant number: 01–01/2017).
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
F. Soysal contributed to conceptualization, methodology, investigation, writing - original draft. B. Unsal contributed to supervision, writing - review & editing and project administration. S.C Isler and G. Akca contributed to the investigation, writing - review & editing and resources. B. Bakirarar contributed to formal analysis and resources. M. Ozcan contributed to, writing - review & editing and resources. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the human subjects ethics board of Ankara University, Faculty of Dentistry (Protocol ID: 36290600/51). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soysal, F., Unsal, B., Isler, S.C. et al. Evaluation of salivary stress markers and inflammatory cytokine levels in peri-implantitis patients. Clin Oral Invest 28, 290 (2024). https://doi.org/10.1007/s00784-024-05692-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05692-5