Abstract
Objectives
To assess the long-term clinical performance of ceramic in-/onlays (CIOs) and cast gold partial crowns (CGPCs) in posterior teeth in terms of success, survival, complications (biological, technical) and quality.
Material and methods
In a retrospective study, a total of 325 patients were recorded after up to 24.8 years (mean 13.9 ± 3.8 years) having (pre-)molars restored with CIO (Empress I, Ivoclar Vivadent, n = 161) and CGPC (Degunorm, DeguDent, n = 164) by supervised undergraduate students. A total of 296 restorations were assessed clinically and radiologically in healthy and endodontically treated teeth using modified United States Public Health Service (USPHS) criteria. Cumulative success and survival rates of the restorations were calculated using Kaplan–Meier estimates. Biological and technical complications were recorded. Status of oral health comprising caries risk and localized periodontitis were assessed.
Results
The cumulative success rates of CIOs were 92.1% and of CGPCs 84.2% after mean service times of 14.5 years. The annual failure rates of total service times were 0.5% in teeth restored with CIO (n = 155) and 0.7% in teeth restored with CGPC (n = 163). The cumulative survival rates of CIOs were 93.9% after a mean service time of 15.2 years and decreased to 91.7% after 23.5 years. The cumulative survival rates of CGPCs were 92.6% after a mean service time of 14.9 years and 91.8% after 23.5 years. Complications in CIOs (n = 149) were ceramic fracture (6.7%), secondary caries (4.7%), endodontic complication (2.7%) and tooth fracture (1.3%) compared to CGPCs (n = 147) with endodontic complication (8.8%), secondary caries (4.8%) and decementation (2.0%). Endodontically treated teeth restored with CIO or CGPC revealed significantly less often success compared with corresponding vital teeth (p = .02). CIOs and CGPCs revealed clinically and radiographically good and excellent qualities with 71.8% (107/149) and 68% (100/147) without any significant differences regarding type of restoration.
Conclusions
Both CIOs and CGPCs achieved high survival rates up to 24.8 years when performed by supervised undergraduate students. The longevity of the restorations may benefit from the intraoral repair of accessible defects and, in case of pulp infection or necrosis, an adequate endodontic management.
Clinical relevance
CIOs and CGPCs made by supervised undergraduate students are proper restoration types in posterior teeth in the long-term. An adequate preparation design, meticulous care in the inserting technique and constant biofilm removal due to proper oral hygiene combined with professional maintenance care are substantial. The clinical long-term performance was mostly limited by ceramic fractures in CIOs and endodontic complications in CGPCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Partial crowns, in- and onlays are common types of indirect restorations in posterior teeth. They are usually manufactured from gold alloys or ceramics, nowadays sometimes from composite or polymer-infiltrated ceramics. They allow a functional reconstruction of large defects while preserving more sound hard tissue compared to full crown coverage [1]. Endodontically treated premolars and molars may benefit from this approach since partial crowns are believed to reinforce such teeth by minimizing diverging forces impacting the cups which might lead to tooth fracture [2,3,4]. Consequently, lower mean fracture rate values were reported in endodontically treated teeth restored with indirect restorations compared to those with direct restorations [5]. Previous studies revealed a lower annual failure rate for indirect restorations in posterior teeth compared to direct restorations [6, 7]. Recent investigations showed rather similar annual failure rates for both restoration types (direct: 1.1%; indirect: 1.6%) [8, 9]. However, a recent meta-analysis assessing the clinical performance of composite and ceramic restorations showed that the failure risk increased with defect size. Further, one common complication was the fracture of the ceramic, whereas resin composite materials mainly failed due to secondary caries [10]. If adhesive techniques with cusp-replacement are used, the performance of direct postendodontic restorations seems to be almost equivalent to that of indirect techniques [11]. From a clinical perspective, indirect restorations can be considered to be superior to direct fillings in terms of marginal adaption, polishing, and design of the proximal contact area [12].
Esthetic requirements play a crucial role in selecting the most suitable type of restoration. Tooth-colored materials allow a wide range of reconstructions complying with highest esthetic demands. Further, the preparation design can be extended on buccal tooth cusps and surfaces. Nowadays, when restoring teeth with cast gold partial crowns (CGPC), the extension of the preparation should be limited to esthetically insignificant tooth surfaces resulting in a more challenging tooth preparation.
Gold alloys are characterized by two substantial longevity-related dental material properties: the plastic deformation of its metallic microstructure and the effect of increased hardness after deformation. In a restoration’s lifetime occlusal forces and recurrent occlusal wear deform the metallic surface. Thus, a micro-mechanical adaptation might rather resist the effects of abrasion and attrition in the long-term. That is why the fracture of an alloy can be almost excluded as a complication of clinical relevance. Ceramics have different properties and limitations, irrespective of their various fabrication methods: the proneness for cohesive and adhesive fractures, a high brittleness, a high bending strength, a low toughness, and specific handling requirements regarding the design of prepared cavity or adhesive luting method [13, 14]. Several studies investigated the beneficial effects of adequate ceramic thickness with a minimum of approximately 1.5 mm, cusp coverage preferred in endodontically treated teeth, adequate remaining cusp wall thickness with at least 2.0 mm, and proper ceramic surface processing in order to reduce failures such as crack formation [15,16,17,18,19]. However, there is much evidence in literature, that fracture poses the most common failure of ceramics [20,21,22]. Other adverse events are secondary caries, retention loss, and delayed endodontic treatment for both restoration types [23,24,25,26,27,28,29,30,31,32]. Nevertheless, the crucial advantages of partial crowns made of gold alloys or ceramics are the high amount of preserved sound dental hard tissue and the excellent biocompatibility [33].
Many different patient- and operator-related factors affect the longevity of an indirect restoration. Restorative aspects are an extensive loss of dental hard tissue in posterior teeth, a cost–benefit-analysis balancing other treatment options, and the feasibility of the adhesive cementation. Several clinical studies revealed favourable rates of survival in vital teeth restored with CGPCs compared to similar rates in those with ceramic partial crowns (CPCs) [23, 30, 31], in endodontically treated teeth as well [34]. Survival estimates were calculated after 13 years with 72% in CGPCs from 42 patients and after 7 years with 81% in CPCs from 22 patients [30]. One prospective split-mouth study showed a cumulative survival rate after 5.5 years with 93.3% in CGPC and 88.8% in CPCs from 29 patients [31]. Interestingly, the pooled estimated 10-year survival rate of ceramic inlays, onlays and overlays (n = 2154 restorations) was calculated with 91% regardless of the material (glass ceramic or feldspathic porcelain), study design or setting [20]. Whereas the range of Kaplan–Meier-survival estimates in teeth with CGPC revealed 72 to 98.9% [24, 25, 30, 31, 35], the survival for ceramic restorations after 4 to 8 years was 81 to 92% [29,30,31, 36,37,38] and up to 18 years with 75.9 to 92.4% [26,27,28, 39, 40]. A drawback of clinical studies calculating cumulative survival rates remain short-term observation data and small sample sizes of patients/restorations in a selected pool.
This retrospective study aimed to evaluate the long-term performance of CGPCs and ceramic in-/onlays (CIOs) with the primary outcomes of calculating the cumulative success and survival rates. Secondary outcomes were quality and complications (biological, technical). The study collective was a patient pool treated within one consistent university teaching from two decades.
Material and methods
Three-hundred-twenty-five study participants were recruited from a pool of 1651 patients, who received CGPCs (Degulor C) and CIOs (leucite reinforced glass ceramic) between the years 1994 and 2009 at the Department of Conservative Dentistry and Periodontology, University Hospital of Würzburg, Germany. All restorations were performed by supervised fifth-year students in vital and endodontically treated teeth. Ethical approval (no. 184/15) was obtained from the local ethics committee for the clinical and radiographic evaluation and all participants provided written informed consent. There was a total of 1126 patients meeting the inclusion criteria (Table 1). A patient’s restoration was excluded in case of less than three years of service time in order to exclude any technical short-term failures. A total of 600 patients was successfully contacted by phone on two occasions or once by mail. Three hundred and twenty-five patients were willing to make an appointment for the follow-up examination (Table 2), performed by two dentists (L.D.,C.S.) achieving a consensus. The clinical examination started with two calibration-set-ups of all variables for the first ten restorations of each type (CGPC/CIO) in coordination with a certified university’s principal investigator (R.K.) with ten years of experience in restorative dentistry. The presence or absence of clinical signs and symptoms were assessed using pain, discomfort, sensitivity to percussion and pulp vitality, pocket probing depth (PPD) and clinical attachment level (CAL). Further, tooth mobility index by Lindhe & Nyman (1977), sulcus bleeding index (SBI) compassing six measuring points per tooth by Mühlemann & Son (1971) and the modified Plaque-Index by Turesky (1970) were assessed. Caries risk assessment was performed according to Hotz et al. (2005) and categorised into three degrees. Digital radiographs (VistaScan, Duerr Dental SE, Bietigheim-Bissingen, Germany) were made to evaluate the presence of periapical lesion, secondary caries and quality of the restoration.
The CGPCs were manufactured by using high-gold alloy (Degulor C, Degudent, Dentsply Sirona, Bensheim, Germany) and inserted with glass ionomer cement (Ketac™ Cem, 3 M, Neuss, Germany). The CIOs were made of leucite reinforced glass ceramic (Empress I, Ivoclar Vivadent AG, Schaan, Liechtenstein) and inserted with an adhesive resin cement (to 54.2% with Bifix QM, VOCO GmbH, Cuxhaven, Germany; to 38.3% with Compolute™, 3 M, or Variolink, Ivoclar Vivadent AG) or by using acid-etch-technique with a flowable composite (Tetric EvoFlow, Ivoclar Vivadent AG). During inserting the CIOs rubber dam was used obtaining moisture-free environment. The placement of partial crowns was usually performed by fifth-year students supervised by university’s dentists. A total of 13.5% (44/325) of the student’s restorations were inserted by the dentist, predominantly in challenging cases.
In case of CGPC the cusps from maxillary teeth were covered up to the buccal ridge line, cusps from mandibular teeth were minimally extended on the external surface. In the case of ceramics at least one cusp-replacement was needed to include it in this study assessing different types of CIO with three up to five restored tooth surfaces. At follow-up patients had a mean age of 59.2 ± 10.8 years. The mean observation times were 13.8 ± 4.1 years for CGPCs (n = 164) and 14.0 ± 3.5 years for CIOs (n = 161, 3 missings).
Modified United-States-Public-Health-Service (USPHS)-criteria (in total 13) were used for evaluation of restorations’ quality with a range of 1 to 5 scores (Hickel et al. 2007) (Table 3). Two categories were defined subdividing various quality levels (Table 4). All restorations of a patient were systematically listed. CGPCs and CIOs with earliest date of placement were selected obtaining one restoration for each patient. Complications with the time point of intervention, type and diagnosis during and after placement of the selected restoration were collected from the patient records or the attended dentist.
The dichotomized variable “oral health” was defined based on the findings of evident gingivitis (SBI values ≥ 10%), high plaque accumulation (PI > 3), and increased caries risk (≥ 2) for diagnosing poor oral health. Localized periodontitis was detected in the region of both the restored tooth and the adjacent teeth if signs of increased tooth mobility (≥ 2) and/or increased PPD (≥ 5 mm) were present compared critically with radiological findings of pathologic bone loss. Additionally, data were categorised in terms of the tooth type (premolar or molar) and a dichotomized variable regarding vital or non-vital tooth (with endodontic complication).
A total of n = 325 patients were used for descriptive statistics and the calculation of Kaplan–Meier success and survival rates based on treatment outcomes (Table 5). Esthetic, functional, and biological characteristics were assessed in restored teeth of examined patients at follow-up (n = 296). Statistical analyses were performed with SPSS software (Vers. 28.0.1.1, IBM Corp., Armonk, USA). Chi-square-tests for independence with Yates Continuity Correction were conducted on 2 × 2 contingency tables showing significant differences of non-metric scaled data. Effect sizes were expressed as Phi (φ) or Cramer’s V. Binary logistic regression analyses were conducted to test if there are specific predictors for success or non-success. Cox & Snell R2 and Nagelkerkes R2 indicated the model’s variance of dependent variables. Kaplan–Meier analysis were represented graphically to point out complications within the selected observation period. The use of the log-rank test allowed comparing success and survival rates of CGPCs and CIOs as unpaired samples. The null hypothesis, that posterior teeth restored with either CIO or CGPC do not differ in terms of success, survival, failure or quality of the restoration in the long-term, was tested. The level of statistical significance was set at α = 0.05.
Results
Excellent and good qualities were assessed up to 68% (100/147) in CGPCs and 71.8% (107/149) in CIOs. There were no significant differences between the quality of CGPC and that of CIO for category A (χ2(1, n = 296) = 1.51, p = 0.22, φ = -0.07) and category B (χ2(4, n = 296) = 6.6, p = 0.16, Cramer’s V = 0.15).
The restorations of the recalled patients revealed similar success rates with 75.6% (124/164) in case of CGPC (range of follow-up: 3.2 to 24.3 years) and 78.3% (126/161) in case of CIO (3.3 to 24.8 years) (Table 6). There was no significant correlation between the prevalences of success and survival compared with the types of restoration, χ2 (3, n = 325) = 7.51, p = 0.06. There was a significant correlation between failure and the type of restoration, χ2 (1, n = 46) = 4.62, p = 0.03, φ = 0.36. Posterior teeth with CGPC were rather extracted than those with CIO, whereas teeth with CIO rather achieved a new restoration than those with CGPC. Endodontic failure was the most common reason for failure in teeth restored with CGPC (29.4%, 5/17). Except for vertical bone loss, other reasons were not recorded. No reasons were identified for extraction of all teeth with CIO restored (n = 5). Secondary caries was the main reason for re-restoring teeth with a new CGPC (5/10). Correspondingly, there were 14 teeth with CIO which received a new restoration. Three cases (3/14) were affected by secondary caries and another three (3/14) by ceramic fracture. Further reasons in remaining cases (8/14) were not recorded.
The category failure was detected after a mean service time of 11.3 ± 4.4 years (n = 42, 4 missings). Kaplan–Meier estimates were compiled comparing the periods of success or survival between CGPC and CIO. In terms of a 20-year service time 84% (137/163) of CGPCs and 90.3% (140/155) of CIOs had to be censored due to shorter times of follow-up estimating success. Estimating survival, 92.6% (151/163) of CGPCs and 92.9% (144/155) of CIOs had to be censored due to shorter times of follow-up, respectively.
The null hypothesis was not rejected as the log-rank-test revealed no significant difference regarding the category success between CGPCs and CIOs, χ2 (1, n = 311 (CIO: 149, 6 missings; CGPC: 162, 1 missing)) = 2.85, p = 0.091.
The cumulative success rates of CIOs were 92.1% after a mean service time of 14.5 years and decreased to 89.3% after 22.4 years. The cumulative success rates of CGPCs were 84.2% after a mean service time of 14.5 years and 82.9% after 23.8 years, respectively (Fig. 1). The annual failure rates of total service times were 0.5% in teeth restored with CIO and 0.7% in teeth restored with CGPC.
The cumulative survival rates of CIOs were 93.9% after a mean service time of 15.2 years and decreased to 91.7% after 23.5 years. The cumulative survival rates of CGPCs were 92.6% after a mean service time of 14.9 years and 91.8% after 23.5 years, respectively (Fig. 2).
Of all teeth 84.5 ± 0.1% were free of complications. Endodontic complications were more often found in CGPCs (8.8%) than in CIOs (2.7%). Secondary caries was approximately to 4.7% in both types of restoration (Table 7). Survival of restorations was not associated with endodontic complication, rather with secondary caries and ceramic fracture (Table 8). All fractures of CIOs were detected in vital teeth (10/137). Complications were almost equally distributed to 22.9% (60/262) in molars and to 23.8% (15/63) in premolars. There were defects in need of repair up to 20.8% (31/149) in CIOs and 25.9% (38/147) in CGPCs.
A logistic regression was conducted in order to test a model predicting failure in teeth restored with CGPCs or CIOs depending on following factors: complication, secondary caries, endodontic complication, patient’s age, age of restoration, and gender. This model was significant with all six predictors, χ2 (6, n = 296) = 77.84, p < 0.01. It ranged between 23.1% (Cox & Snell R2) and 65% (Nagelkerkes R2). It met the correct category with a rate of 96.3%. In case of secondary caries as the one significant predictor of this model the probability of predicting “no success” increased with an odds ratio of 6.6 (Table 9).
Endodontically treated teeth restored with CGPC or CIO showed low rates of failures irrespective of treatment pre- or postoperatively (Table 10). There was a significant difference between the outcome “success or survival” in contrast to failure and performed endodontic therapy in restored teeth, χ2 (2, n = 296) = 7.36, p = 0.02, Cramer’s V = 0.16.
Regarding the evaluation of biological complications affecting treatment outcome the variable „oral health “ was assessed in examined teeth (n = 295, 1 missing). There was a homogenous distribution of the patients in terms of „oral health “ with the different treatment outcome for both restoration types (CGPC and CIO) (Table 11). The absence of secondary caries in restored teeth was detected in 95.1% (235/247) of the patients with „good oral health “ and in 95.8% (46/48) of the patients with „poor oral health “. There was no significant correlation in patients with poor oral health between the type of restoration (CGPC or CIO) and the presence of secondary caries, χ2 (1, n = 48) = 0.96, p = 0.33.
Additionally, the impact of localized periodontitis in the region of the restored tooth on complication rate and the treatment outcome were evaluated. There was no significant correlation between the presence of localized periodontitis and the occurrence of complication in restored teeth, χ2 (1, n = 295) = 0.13, p = 0.72. Further, there was no significant correlation between the presence of localized periodontitis and failure of restoration, χ2 (1, n = 295) = 3.19, p = 0.07.
Discussion
The present study revealed high cumulative success rates with 92.1% and 84.2% after mean service times of 14.5 years in posterior teeth restored with CIO (leucite reinforced glass ceramic) or CGPC (high gold alloy) performed by supervised undergraduate students. There were similiar annual failure rates of total service times with 0.5% and 0.7%, respectively. The cumulative survival rates were 81.3% in CIOs after 23.7 years and 76.1% in CGPCs after 23.8 years. Of all examined teeth, 84.5% stayed free of complication. There were excellent and good qualities with a rate of 71.8% in teeth restored with CIO and 68% in teeth restored with CGPC.
The recall rate was 28.9% (325/1126), which is a common drawback of retrospective clinical studies [41,42,43,44]. A low recall rate may limit the results due to a high drop-out rate as a common effect in long-term observational studies. Various drop-out rates in long-term studies were reported with 12.3% after a mean observation period of 18.7 years [24] assessing gold restorations, with 9.5% after 15 years [28] in a prospective study assessing ceramic restorations or up to 40% after eleven [45] and twelve years [26] in retrospective studies. In the present study, randomly selected and non-specific patients were examined, in contrast to other studies excluding patients with poor oral hygiene and bruxism [26, 38, 46, 47], with high caries risk [48], or with endodontically treated teeth [46]. Within the limitations of the high drop-out rate and the retrospective study design, the included patient pool of this study seems to represent general practice patients with various risk factors. Each patient was invited to be part of a systematic follow-up examination with professional tooth cleaning service or, if necessary, a systematic treatment of periodontitis. In the present study, 83.7% of the recalled patients showed a status of good oral health. Secondary caries was with a rate of 4.7% very low for both types of restoration. It can be assumed that there was a beneficial effect of good oral hygiene supporting the effect of caries prevention.
Selected study criteria aimed to exclude technical short-term failures, which can be caused by procedural errors from the operator or the dental technician. Failures do also occur due to inadequate properties of the dental material. In the present clinical study, the adhesive cementation was always performed using rubberdam in order to minimize the risk of debonding in CIOs. Other key aspects of the present study were a well-established and standardized university’s training concept since nearly two decades, the systematic support of supervising dentists, and the entire dental technical work supported by two experienced dental technicians (K.H., J.M.) from an in-house dental laboratory. Thus, all indirect restorations were fabricated and inserted with the claim for a high level of accuracy resulting in a clinical performance as good as possible. The present study showed excellent and good qualities with 68% (in CGPCs) and 71.8% (in CIOs) for both types of restoration. There are no differences regarding the clinical performance or the survival of ceramic restorations in data pools from university teaching compared with data pools from private practice [49].
In literature, there are numerous short-term and a few long-term data with high survival rates for teeth restored with ceramic partial crowns, mostly up to ten years. It was also reported that includable information on the survival of ceramic on- and overlays performing up to 15 years are barely available [49].
Numerous retrospective studies revealed survival data of partial crown coverage in posterior teeth with a high number of recalled patients [23, 24, 27, 29, 30, 36, 38] compared to a few prospective medium- and long-term studies, usually with a low number of patients. One prospective split-mouth study assessed the quality and the cumulative survival rates of CGPC (93.3%) compared with CIO (88.8%) from 29 patients after 5.5 years [31]. Another split-mouth study revealed a survival rate of 97% or more in posterior teeth restored with two types of ceramic onlays from 25 patients at the 7-years follow-up [50]. There are two prospective clinical studies assessing the success rates of ceramic in- and onlays with a maximum of 96 restorations after 12 years [26, 32]. Further, there is one prospective study revealing a success rate of 75.9% after a 15-years follow-up in 252 partial and complete all-ceramic coverage restorations from 121 patients [28]. In a prospective non-randomized clinical study all 103 occlusal lithium disilicate onlays were in function at the 11-years follow-up from seven patients suffering severe tooth wear [51].
In a review, medium-term survival rates were evaluated for ceramic onlays with 91 to 100% after two up to five years [52]. The long-term survival rates decreased to 71—98.5% after more than five years. Interestingly, neither the fabrication materials, the methods, nor the adhesive bonding systems seemed to affect longevity. The ceramic thickness of at least 2 mm and a retentive preparation design were evaluated to be more crucial. Further, ceramic failures were more often in non-vital teeth, posterior teeth and teeth from patients with parafunctional habits. A recently published meta-analysis revealed a pooled overall survival for ceramic onlays with 89.2% after five years including four studies [49]. Malament et al. [53] revealed a remarkable high estimated cumulative survival rate of e.max lithium disilicate glass ceramic onlays with 98.3% at 9.8 years. These authors showed additional data with an estimated cumulative survival rate of 95% in posterior complete and partial coverage ceramic restorations at 16.9 years [54]. Interestingly, the 10-years survival rate of CGPCs (n = 1679) was reported with 86.1% compared to estimated rates of other studies with a range of 70—96% [23]. Largely consistent with current literature, in the present study the survival estimates of CIOs and CGPCs from 325 patients were similar with 93.9 after 15.2 years and 92.6% after 14.9 years. However, the difference of the higher success rates of CIO (92.1%) compared to the lower rates of CGPC (84.2%) after 14.5 years was minimized obviously with follow-up times of more than 20 years.
Metal restorations, such as CGPC, do have a wide range of clinical applications since decades. They are characterized by a well-established manufacturing process in dental laboratory and must be considered as clinically proven. Modern dentistry does focus more and more on the preservation of dental hard tissue, a high biocompatibility of dental materials and the patient’s wish for tooth colored restorations in order to obtain good esthetic results. Teeth restored with ceramic partial coverage restorations are able to meet these requirements. However, the depth of the tooth cavity is still one crucial parameter when selecting the most suitable type of restoration, particular in case of defects below the cementoenamel junction (CEJ). The more subgingival the margin of the sound dental hard tissue is located, the more challenging is the reliable use of an adhesive technique, which is needed to insert a CIO properly. In our department operators rather preferred to restore teeth with subgingival cavities with CGPC than CIO, especially in the upper molars. To overcome deep-cavity associated restrictions of restoring posterior teeth with ceramics, deep margin elevation was introduced, e.g. in case of ceramic and resin composite inlays [55, 56]. Hereby the operator builds up the deepest dentinal cavity with a few layers of composite in order to allow placing the indirect restoration’s margin superior to the CEJ. A recent study demonstrated an overall cumulative survival rate of 95% with a mean observation time of 4.8 years in such restored teeth [57]. Besides the higher rate of biofilm accumulation on composite surfaces compared to ceramic surfaces, significantly more degradation of the composite build-ups was shown over time. Thus, one might suppose there is a high risk for the formation of secondary caries as a potential complication in the long-term. However, until now, the current evidence, mainly based on laboratory studies and limited clinical data, indicates that the deep marginal elevation can be a promising approach to restore teeth with localized subgingival defects resulting in good periodontal health [58]. In the present study, this specific concept was not implemented. According to the former university’s teaching concept in restorative dentistry, molars with extremely deep localized subgingival defects were restored more likely with CGPCs. The data highlight the outstanding long-term survival of teeth restored with both types, CIO or CGPC.
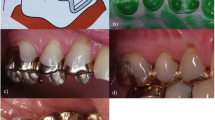
Interestingly, in cases of restoring posterior teeth with CIO, it was reported that failures do occur commonly in the molar region [53]. In the present study, the proportion of molars in teeth restored with CGPC or CIO was 89.6 or 71.4%. Taking into account the above mentioned more challenging restorative condition in molars restored with CGPC and the higher number of such teeth compared to the molars restored with CIO, both cumulative success estimates are close to each other with 82.9% (CGPC) and 89.3% (CIO) after 23.8 and 22.4 years. Fig. 3
In the present study, secondary caries was the significant predictor for a probability model predicting failure with an odds ratio of 6.6. The model included restorative and endodontic complications, secondary caries, patient’s age, age of restoration, and gender. Endodontic complications occurred three times more often in CGPCs than in CIOs. Survival of restorations was not associated with endodontic complication, rather with secondary caries and ceramic fracture. However, the root canal treated tooth is deemed to be a substantial risk factor for the survival of teeth with cast gold restorations [24]. In the present work, the performance of endodontic therapy affected significantly the estimate of success, however, pre- and postoperatively, there was a low rate of failures. Adverse events e.g. chipping or fracture of the ceramic restoration is common and well-reported, mainly occurring as an early complication [59]. In the long-term operator- and patient-related factors have a higher impact on treatment outcome than restorative therapy choices. Periodontal and endodontic reasons, which may lead to an early tooth loss, must be evaluated carefully. Within the limitations of this retrospective study, it is possible to overestimate the promising long-term success rates of both restoration types from the recalled patients due to a high rate of censored restorations within the observation period. However, a restorative concept of high quality and the need for professional tooth cleaning supporting the patient’s skills maintaining good oral health seem to be crucial in order to obtain high success rates of dental restorations in the long-term. Fig. 4
Conclusions
CIOs and CGPCs achieved high cumulative success rates with 92.1 and 84.2% after 14.5 years performed by supervised undergraduate students. After up to 24.8 years, there were excellent and good qualities with a rate of 68% in teeth restored with CGPC and 71.8% in those restored with CIO. The longevity of the restorations may benefit from the intraoral repair of accessible defects and, in case of pulp infection or necrosis, an adequate endodontic management.
Clinical relevance: CIOs and CGPCs made by supervised undergraduate students are proper restoration types in posterior teeth in the long-term. An adequate preparation design, meticulous care in the inserting technique and constant biofilm removal due to proper oral hygiene combined with professional maintenance care are substantial. The clinical long-term performance was mostly limited by ceramic fractures in CIOs and endodontic complications in CGPCs.
References
Edelhoff D, Sorensen JA (2002) Tooth structure removal associated with various preparation designs for posterior teeth. Int J Perio Res Dent 22(3):241–249
Mannocci F, Cowie J (2014) Restoration of endodontically treated teeth. Br Dent J 216(6):341–346
Carvalho MA, Lazari PC, Gresnigt M, Del Bel Cury AA, Magne P (2018) Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz Oral Res 32(suppl 1):e74
Frankenberger R, Winter J, Dudek MC, Naumann M, Amend S, Braun A, Kramer N, Roggendorf MJ (2021) Post-fatigue fracture and marginal behavior of endodontically treated teeth: partial crown vs. full crown vs. endocrown vs. fiber-reinforced resin composite. Materials (Basel) 14(24):7733
Dammaschke T, Steven D, Kaup M, Ott KH (2003) Long-term survival of root-canal-treated teeth: a retrospective study over 10 years. J Endod 29(10):638–643
Manhart J, Chen H, Hamm G, Hickel R (2004) Buonocore Memorial Lecture Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent 29(5):481–508
Hickel R, Manhart J (2001) Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent 3(1):45–64
Collares K, Correa MB, Laske M, Kramer E, Reiss B, Moraes RR, Huysmans MC, Opdam NJ (2016) A practice-based research network on the survival of ceramic inlay/onlay restorations. Dent Mater 32(5):687–694
Pallesen U, van Dijken JW (2015) A randomized controlled 30 years follow up of three conventional resin composites in Class II restorations. Dent Mater 31(10):1232–1244
Fan J, Xu Y, Si L, Li X, Fu B, Hannig M (2021) Long-term Clinical Performance of Composite Resin or Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-analysis. Oper Dent 46(1):25–44
Plotino G, Buono L, Grande NM, Lamorgese V, Somma F (2008) Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J Prosthet Dent 99(3):225–232
FronChabouis H, SmailFaugeron V, Attal JP (2013) Clinical efficacy of composite versus ceramic inlays and onlays: a systematic review. Dent Mater 29(12):1209–1218
Li RW, Chow TW, Matinlinna JP (2014) Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res 58(4):208–216
Zhang Y, Sailer I, Lawn BR (2013) Fatigue of dental ceramics. J Dent 41(12):1135–1147
Murgueitio R, Bernal G (2012) Three-year clinical follow-up of posterior teeth restored with leucite-reinforced ips empress onlays and partial veneer crowns. J Prosthodont 21(5):340–345
Frankenberger R, Petschelt A, Kramer N (2000) Leucite-reinforced glass ceramic inlays and onlays after six years: clinical behavior. Oper Dent 25(6):459–465
Federlin M, Krifka S, Herpich M, Hiller KA, Schmalz G (2007) Partial ceramic crowns: influence of ceramic thickness, preparation design and luting material on fracture resistance and marginal integrity in vitro. Oper Dent 32(3):251–260
Krifka S, Anthofer T, Fritzsch M, Hiller KA, Schmalz G, Federlin M (2009) Ceramic inlays and partial ceramic crowns: influence of remaining cusp wall thickness on the marginal integrity and enamel crack formation in vitro. Oper Dent 34(1):32–42
Frankenberger R, Zeilinger I, Krech M, Mörig G, Naumann M, Braun A, Krämer N, Roggendorf MJ (2015) Stability of endodontically treated teeth with differently invasive restorations: Adhesive vs. non-adhesive cusp stabilization. Dent Mater 31(11):1312–20
Morimoto S, Rebello de Sampaio FB, Braga MM, Sesma N, Ozcan M (2016) Survival Rate of Resin and Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-analysis. J Dent Res 95(9):985–994
Vagropoulou GI, Klifopoulou GL, Vlahou SG, Hirayama H, Michalakis K (2018) Complications and survival rates of inlays and onlays vs complete coverage restorations: A systematic review and analysis of studies. J Oral Rehab 45(11):903–920
Belli R, Petschelt A, Hofner B, Hajto J, Scherrer SS, Lohbauer U (2016) Fracture Rates and Lifetime Estimations of CAD/CAM All-ceramic Restorations. J Dent Res 95(1):67–73
Stoll R, Sieweke M, Pieper K, Stachniss V, Schulte A (1999) Longevity of cast gold inlays and partial crowns–a retrospective study at a dental school clinic. Clin Oral Investig 3(2):100–104
Studer SP, Wettstein F, Lehner C, Zullo TG, Scharer P (2000) Long-term survival estimates of cast gold inlays and onlays with their analysis of failures. J Oral Rehabil 27(6):461–472
Donovan T, Simonsen RJ, Guertin G, Tucker RV (2004) Retrospective clinical evaluation of 1,314 cast gold restorations in service from 1 to 52 years. J Esthet Restor Dent 16(3):194–204
Frankenberger R, Taschner M, Garcia-Godoy F, Petschelt A, Krämer N (2008) Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent 10(5):393–398
Reiss B (2006) Clinical results of Cerec inlays in a dental practice over a period of 18 years. Int J Comput Dent 9(1):11–22
van Dijken JW, Hasselrot L (2010) A prospective 15-year evaluation of extensive dentin-enamel-bonded pressed ceramic coverages. Dent Mater 26(9):929–939
Felden A, Schmalz G, Hiller KA (2000) Retrospective clinical study and survival analysis on partial ceramic crowns: results up to 7 years. Clin Oral Investig 4(4):199–205
Wagner J, Hiller KA, Schmalz G (2003) Long-term clinical performance and longevity of gold alloy vs ceramic partial crowns. Clin Oral Investig 7(2):80–85
Federlin M, Hiller KA, Schmalz G (2010) Controlled, prospective clinical split-mouth study of cast gold vs. ceramic partial crowns: 5.5 year results. Am J Dent 23(3):161–7
Santos MJ, Freitas MC, Azevedo LM, Santos GC Jr, Navarro MF, Francischone CE, Mondelli RF (2016) Clinical evaluation of ceramic inlays and onlays fabricated with two systems: 12-year follow-up. Clin Oral Investig 20(7):1683–1690
Donovan TE, Chee WW (1993) Conservative indirect restorations for posterior teeth Cast versus bonded ceramic. Dent Clin North Am 37(3):433–43
Dammaschke T, Nykiel K, Sagheri D, Schäfer E (2013) Influence of coronal restorations on the fracture resistance of root canal-treated premolar and molar teeth: a retrospective study. Aust Endod J 39(2):48–56
Erpenstein J, Kerschbaum T, Halfin T (2001) Long-term survival of cast-gold inlays in a specialized dental practice. Clin Oral Investig 5(3):162–166
Bühler J, Naef MA, Amato M, Krastl G, Weiger R, Zitzmann NU (2017) Partial Ceramic Crowns Prepared by Dental Students: Clinical Performance Up to Five Years. J Dent Educ 81(6):732–743
Krämer N, Frankenberger R (2005) Clinical performance of bonded leucite-reinforced glass ceramic inlays and onlays after eight years. Dent Mater 21(3):262–271
Naeselius K, Arnelund CF, Molin MK (2008) Clinical evaluation of all-ceramic onlays: a 4-year retrospective study. Int J Prosthodont 21(1):40–44
Stoll R, Cappel I, Jablonski-Momeni A, Pieper K, Stachniss V (2007) Survival of inlays and partial crowns made of IPS empress after a 10-year observation period and in relation to various treatment parameters. Oper Dent 32(6):556–563
Beier US, Kapferer I, Burtscher D, Giesinger JM, Dumfahrt H (2012) Clinical performance of all-ceramic inlay and onlay restorations in posterior teeth. Int J Prosthodont 25(4):395–402
Archibald JJ, Santos GC Jr, Moraes Coelho Santos MJ (2018) Retrospective clinical evaluation of ceramic onlays placed by dental students. J Prosthet Dent 119(5):743-48e1
Lindner S, Frasheri I, Hickel R, Crispin A, Kessler A (2023) Retrospective clinical study on the performance and aesthetic outcome of pressed lithium disilicate restorations in posterior teeth up to 8.3 years. Clin Oral Investig 27(12):7383–93
Sailer I, Bonani T, Brodbeck U, Hämmerle CH (2013) Retrospective clinical study of single-retainer cantilever anterior and posterior glass-ceramic resin-bonded fixed dental prostheses at a mean follow-up of 6 years. Int J Prosthodont 26(5):443–450
Strasding M, Sebestyen-Huvos E, Studer S, Lehner C, Jung RE, Sailer I (2020) Long-term outcomes of all-ceramic inlays and onlays after a mean observation time of 11 years. Quintessence Int 51(7):566–576
Fradeani M, Redemagni M (2002) An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quint Int 33(7):503–510
Guess PC, Strub JR, Steinhart N, Wolkewitz M, Stappert CF (2009) All-ceramic partial coverage restorations–midterm results of a 5-year prospective clinical splitmouth study. J Dent 37(8):627–637
Krämer N, Taschner M, Lohbauer U, Petschelt A, Frankenberger R (2008) Totally bonded ceramic inlays and onlays after eight years. J Adhes Dent 10(4):307–314
Galiatsatos AA, Bergou D (2008) Six-year clinical evaluation of ceramic inlays and onlays. Quint Int 39(5):407–412
Naik VB, Jain AK, Rao RD, Naik BD (2022) Comparative evaluation of clinical performance of ceramic and resin inlays, onlays, and overlays: A systematic review and meta analysis. J Conserv Dent 25(4):347–355
Guess PC, Selz CF, Steinhart YN, Stampf S, Strub JR (2013) Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7-year results. Int J Prosthodont 26(1):21–25
Edelhoff D, Güth JF, Erdelt K, Brix O, Liebermann A (2019) Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dent Mater 35(9):1319–1330
Abduo J, Sambrook RJ (2018) Longevity of ceramic onlays: A systematic review. J Esthet Restor Dent 30(3):193–215
Malament KA, Margvelashvili-Malament M, Natto ZS, Thompson V, Rekow D, Att W (2021) 10.9-year survival of pressed acid etched monolithic e.max lithium disilicate glass-ceramic partial coverage restorations: Performance and outcomes as a function of tooth position, age, sex, and the type of partial coverage restoration (inlay or onlay). J Prosthet Dent 126(4):523–32
Malament KA, Margvelashvili-Malament M, Natto ZS, Thompson V, Rekow D, Att W (2021) Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: Performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J Prosthet Dent 126(4):533–45
Frankenberger R, Hehn J, Hajto J, Krämer N, Naumann M, Koch A, Roggendorf MJ (2013) Effect of proximal box elevation with resin composite on marginal quality of ceramic inlays in vitro. Clin Oral Investig 17(1):177–183
Roggendorf MJ, Kramer N, Dippold C, Vosen VE, Naumann M, Jablonski-Momeni A, Frankenberger R (2012) Effect of proximal box elevation with resin composite on marginal quality of resin composite inlays in vitro. J Dent 40(12):1068–1073
Bresser RA, Gerdolle D, van den Heijkant IA, Sluiter-Pouwels LMA, Cune MS, Gresnigt MMM (2019) Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J Dent 91:103227
Eggmann F, Ayub JM, Conejo J, Blatz MB (2023) Deep margin elevation-Present status and future directions. J Esthet Restor Dent 35(1):26–47
Yang Y, Yu J, Gao J, Guo J, Li L, Zhao Y, Zhang S (2016) Clinical outcomes of different types of tooth-supported bilayer lithium disilicate all-ceramic restorations after functioning up to 5 years: A retrospective study. J Dent 51:56–61
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was conducted without third-party support.
Author information
Authors and Affiliations
Contributions
R.K., G.K. and S.S. conceptualized the overall strategy. R.K., L.D. and C.S. contributed to planning and execution. R.K., L.D., and C.S. designed and performed the statistical analyses, including figures and tables. R.K., L.D., C.S., B.H., E.R. and S.S. contributed to the investigation. R.K., G.K. and S.S. contributed to the methodology. R.K. wrote and prepared the original draft. R.K., G.K., E.R., B.H. and S.S. contributed to review and editing. R.K., G.K., B.H. and S.S. provided supervision. R.K. and G.K. contributed to project administration. B.H. and S.S. contributed equally to this work. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval with no. 184/15 was obtained from the local ethics committee of the University Hospital of Würzburg, Germany, for the clinical and radiographic evaluation.
Informed consent statement
All participants provided written informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krug, R., Droste, L., Schreiber, C. et al. Long-term performance of ceramic in/-onlays vs. cast gold partial crowns – a retrospective clinical study. Clin Oral Invest 28, 298 (2024). https://doi.org/10.1007/s00784-024-05682-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05682-7