Abstract
Objective
The aim of this study was to analyze the effectiveness of L-PRF as a healing agent in the postoperative period of third molar extraction surgeries, as well as to investigate secondary effects, such as the reduction of pain, edema and other discomforts after the surgical intervention.
Materials and methods
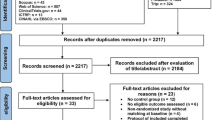
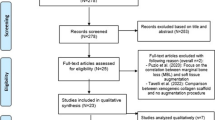
The methodology adopted consisted of carrying out a systematic review of the literature, following the model outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The inclusion criteria were previously established according to a systematic review protocol approved by the Prospective Register of Systematic Reviews (PROSPERO) under number CRD42023484679. In order to carry out a comprehensive search, a search in five databases was carried out, PubMed, Web of Science, Scopus, Cochrane Library and Embase.
Results
The search resulted in the selection of randomized controlled trials that conformed to the established criteria. Two authors independently screened the records and extracted the data. The assessment of bias was conducted according to the guidelines recommended by the Cochrane Collaboration, using version 2 of the Cochrane tool for assessing the risk of bias in randomized trials (RoB 2).
Conclusion
This study demonstrated that L-PRF stands out by providing direct benefits to healing, vascularization and tissue regeneration. Clinical relevance: L-PRF plays an important role in reducing postoperative pain, edema, the incidence of alveolar osteitis and infections after third molar removal surgery, compared to patients who did not undergo the use of L-PRF.



Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Sorg H, Tilkorn DJ, Hager S, Hauser J, Mirastschijski U (2017) Skin wound healing: an update on the current knowledge and concepts. Eur Surg Res 58(1–2):81–94. https://doi.org/10.1159/000455955
Ferguson MW, O’Kane S (2004) Scar–free healing: from embryonic mechanisms to adult therapeutic intervention. Philosophical Trans Royal Soc B: Biol Sci 359(1445):839–850. https://doi.org/10.1098/rstb.2004.1475
Ko KI, Sculean A, Graves DT (2021) Diabetic wound healing in soft and hard oral tissues. Translational Res 236:72–86. https://doi.org/10.1016/j.trsl.2021.08.001
Zhang S, Song S, Wang S, Duan Y, Zhu W, Song Y (2019) Type 2 diabetes affects postextraction socket healing and influences first-stage implant surgery: a study based on clinical and animal evidence. Clin Implant Dent Relat Res 21(3):436–445. https://doi.org/10.1111/cid.12736
Osunde OD, Saheeb BD, Adebola RA (2011) Comparative study of the effect of single and multiple suture techniques on inflammatory complications after third molar surgery. J Oral Maxillofac Surg 69(4):971–976. https://doi.org/10.1016/j.joms.2010.07.028
Coulthard P, Bailey E, Esposito M, Furness S, Renton TF, Worthington HV (2014) Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst Reviews 7. https://doi.org/10.1002/14651858.CD004345.pub3
Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V et al (2017) Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Invest 21:1913–1927. https://doi.org/10.1007/s00784-017-2133-z
Pavlovic V, Ciric M, Jovanovic V, Trandafilovic M, Stojanovic P (2021) Platelet-rich fibrin: basics of biological actions and protocol modifications. Open Med 16(1):446–454. https://doi.org/10.1515/med-2021-0318
Kiencało A, Jamka-Kasprzyk M, Panaś M, Wyszyńska-Pawelec G (2021) Analysis of complications after the removal of 339 third molars. Dent Med Probl 58(1):75–80. https://doi.org/10.17219/dmp/127028
Sifuentes-Cervantes JS, Carrillo-Morales F, Castro-Núñez J, Cunningham LL, Van Sickels JE (2021) Third molar surgery: past, present, and the future. Oral surgery, oral medicine, oral Pathology. Oral Radiol 132(5):523–531. https://doi.org/10.1016/j.oooo.2021.03.004
Ghosh A, Aggarwal VR, Moore R (2022) Aetiology, Prevention and Management of Alveolar Osteitis-A Scoping Review. J Rehabil 49(1):103–113. https://doi.org/10.1111/joor.13268
Daly BJ, Sharif MO, Jones K, Worthington HV, Beattie A (2022) Local interventions for the management of alveolar osteitis (dry socket). Cochrane Database Syst Reviews 9. https://doi.org/10.1002/14651858.CD006968.pub3
Zahid T, Ghafoor S (2021) Molecular events in the clinicopathological diagnosis of alveolar osteitis. J Pak Med Assoc 71(2A):508–513. https://doi.org/10.47391/JPMA.491
La Rosa GRM, Marcianò A, Priolo CY, Peditto M, Pedullà E, Bianchi A (2023) Effectiveness of platelet-rich fibrin in controlling pain associated with alveolar osteitis: a scoping review. Clin Oral Invest 27(7):3321–3330. https://doi.org/10.1007/s00784-023-05012-3
Rakhshan V (2018) Common risk factors of dry socket (alveolitis osteitis) following dental extraction: a brief narrative review. J Stomatology Oral Maxillofacial Surg 119(5):407–411. https://doi.org/10.1016/j.jormas.2018.04.011
Yüce E, Kömerik N (2019) Potential effects of advanced platelet-rich fibrin as a wound-healing accelerator in the management of alveolar osteitis: a randomized clinical trial. Niger J Clin Pract 22(9):1189–1195. https://doi.org/10.4103/njcp.njcp_27_19
Gollapudi M, Bajaj P, Oza RR (2022) Injectable platelet-rich fibrin-a revolution in periodontal regeneration. Cureus 14(8). https://doi.org/10.7759/cureus.32663
Shirbhate U, Bajaj P (2022) Third-generation platelet concentrates in Periodontal Regeneration: gaining Ground in the field of regeneration. Cureus 14(8). https://doi.org/10.7759/cureus.32664
Damsaz M, Castagnoli CZ, Eshghpour M, Alamdari DH, Alamdari AH, Noujeim ZEF et al (2020) Evidence-based clinical efficacy of leukocyte and platelet-rich fibrin in maxillary sinus floor lift, graft and surgical augmentation procedures. Front Surg 7:537138. https://doi.org/10.3389/fsurg.2020.537138
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372(160):1–36. https://doi.org/10.1136/bmj.n160
Fan Y, Perez K, Dym H (2020) Clinical uses of platelet-rich fibrin in oral and maxillofacial surgery. Dental Clin N Am 64(2):291–303. https://doi.org/10.1016/j.cden.2019.12.012
PROSPERO (n.d.). International prospective register of systematic reviews. About PROSPERO. Retrieved from https://www.crd.york.ac.uk/prospero/#aboutpage
Ouzzani H, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan — a web and mobile app for systematic reviews. Syst Reviews 5:210. https://doi.org/10.1186/s13643-016-0384-4
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Fujioka-Kobayashi M et al (2021) Efficacy of platelet-rich fibrin on socket healing after mandibular third molar extractions. J Oral Maxillofacial Surg Med Pathol 33(4):379–388
O’Sullivan L, Gallagher C, Ríordáin RN (2022) Effect of plasma rich in growth factors on quality of life following mandibular third molar removal: a double-blind randomized controlled trial. Int J Oral Maxillofac Surg 51(9):1237–1244
Barhate UH et al (2022) Effects of autologous leukocyte-platelet rich fibrin (L-PRF) on the rate of maxillary canine retraction and various biomarkers in gingival crevicular fluid (GCF): a split mouth randomized controlled trial. Int Orthod 20(4):100681
Antonio SCARANO et al (2021) Autologous platelet gel (APG): a preliminary evaluation of the Mechanical Properties after activation with autologous thrombin and calcium chloride. Materials 14(14):3941. https://doi.org/10.3390/ma14143941
Kalyani P et al (2023) Effect of leucocyte and platelet Rich Fibrin (L-PRF) in postoperative sequelae of impacted mandibular third molar Surgery-A Split Mouth Randomized Controlled Trial. J Popul Ther Clin Pharmacol 30(6):128–133
Afat IM, Akdogan ET, Gonul O (2019) Effects of leukocyte-and platelet-rich fibrin alone and combined with hyaluronic acid on early soft tissue healing after surgical extraction of impacted mandibular third molars: a prospective clinical study. J Cranio-Maxillofacial Surg 47(2):280–286
Da Silva MT et al (2021) Effects of leukocyte-platelet-rich fibrin (L–PRF) on Pain, Soft tissue Healing, Growth factors, and cytokines after third molar extraction: a Randomized, Split-Mouth, double-blinded clinical trial. Appl Sci 11(4):1666
Mourão CFAB et al (2020) The use of leukocyte-and platelet-rich fibrin in the management of soft tissue healing and pain in post-extraction sockets: a randomized clinical trial. J Cranio-Maxillofacial Surg 48(4):452–457
Daugela P et al (2018) Influence of leukocyte-and platelet-rich fibrin (L-PRF) on the outcomes of impacted mandibular third molar removal surgery: a split-mouth randomized clinical trial. Quintessence Int, 49(5)
Funding
There was no funding for this research.
Author information
Authors and Affiliations
Contributions
E.D.R and I.H.G.S: Responsible for the conception of the study, the design of the systematic review and the formulation of the research question. Played a central role in the selection of the inclusion and exclusion criteria for the studies. Actively participated in the search, selection and analysis of the articles. M.R.M.V: Contributed significantly to the literature review and search for evidence. Participated in the critical analysis of the included studies. Collaborated in writing and reviewing the study protocol. J.C.P.F: Involved in the initial screening of articles and the application of inclusion/exclusion criteria. Extracted data from some of the included studies. Participated in writing specific sections of the manuscript. O.F.J: Actively participated in interpreting the results. Proofread and edited the manuscript to ensure accuracy and clarity. E.S: Played a role in the coordination, guidance and logistical management of the systematic review. Participated in the review and final formatting of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
As this was a systematic review, it was not necessary to obtain approval from the research ethics committee to carry out this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro, E.D., de Santana, I.H.G., Viana, M.R.M. et al. Use of platelet- and leukocyte-rich fibrin (L-PRF) as a healing agent in the postoperative period of third molar removal surgeries: a systematic review. Clin Oral Invest 28, 241 (2024). https://doi.org/10.1007/s00784-024-05641-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05641-2