Abstract
Aim
The purpose of the present study was to evaluate permanent teeth with post-traumatic transversal root fractures, for their initial healing modality, the effect of candidate predictors and their long-term prognosis.
Methodology
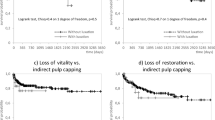
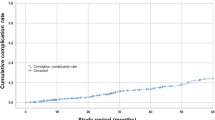
A retrospective longitudinal clinical study was conducted to evaluate records from patients bearing transversal root fractures in permanent teeth in order to radiographically assess short-term healing and non-healing events in the fracture line, their prognostic factors and their relationship with long term outcomes. The inter-fragmentary tissues were classified as healing: hard tissue (HT), connective tissue (CT) or connective tissue and bone (CT + B) and non-healing: interposition of granulation tissue (GT). A competing risk survival analysis was conducted to estimate the hazards of healing and non-healing events in the short-term and the effect of demographic, clinical, and treatment variables was assessed using the subdistribution regression model (Fine & Gray).
Results
Radiographic findings showed 61.4% of healing in the short-term being strongly influenced by the presence and type of concomitant injuries to the coronal fragment. Teeth with concomitant crown fractures (sHR 24.38, 95% CI [3.16–188.3], p = 0.0022), luxations with dislocations (sHR 10.58, 95% CI [1.37–81.9], p = 0.0240) and subluxations (HR 9.66, 95% CI [1.14–81.7], p = 0.0370) were more likely to present non-healing of root fractures in the short-term. The healing rate in the long-term was of 75.9%, most of them with interposition of bone and connective tissue. Kappa statistics demonstrated an overall agreement of 67.1% between short and long-term healing patterns, in special HT and CT + Bone modalities.
Conclusion
Healing at the fracture site was the most frequent outcome, both in the short-term and in the long-term. Short-term healing modality was strongly influenced by the presence and type of concomitant injuries to the crown fragment, being the worst prognosis observed in root-fractured teeth with concomitant crown fractures, followed by concomitant luxations with dislocation.
Clinical relevance
Post-traumatic transversal root fractures have a positive prognosis supporting therefore, a more conservative approach for these teeth before considering more radical treatments.




Similar content being viewed by others
Data availability
The following elements are available upon request: data extracted from clinical records, data used for all analyses and the analytic code. Contactinfo: Juliana Vilela Bastos, julianavbtrauma@gmail.com.
References
Heithersay AO, Geoffrey S, Kahler B (2013) Healing responses following transverse root fracture: a historical review and case reports showing healing with (a) calcified tissue and (b) dense fibrous connective tissue. Dent Traumatol 29(4):253–265
Abbott PV (2019) Diagnosis and management of transverse Root fracture. JournalofEndodontics, v. 45. https://doi.org/10.1016/j.joen.2019.05.009
Andreasen JO, Hjørting–Hansen E (1967) Intraalveolar root fractures: radiographic and histologic study of 50 cases. Journal Oral Surgery, Copenhagen, 25:414 – 26
Andreasen FM, Andreasen JO (1988) Resorption and mineralization processes following root fracture of permanent incisors. EndodDentTraumatol 4:202–214
Andreasen FM, Andreasen JO, Bayer T (1989) Prognosis of root-fractured permanent incisors-prediction of healing modalities, vol 5. Endodontics Dental Traumatology, Copenhagen, pp 11–22
Andreasen (2001) Pulp healing acute following dental trauma: clinical and radiographic review. PractProcedSesthetDent 13:315–322
Cvek M, Mejare I, Andreasen JO (2002) Healing and prognosis of teeth with intra-alveolar fractures involving the cervical part of the root. DentTraumatol 18:57–65
Cvek M, Mèjare I, Andreasen JO (2004) Conservative endodontic treatment of teeth fractured in the middle or apical part of the root. DentTraumatol 20:261–269
Cvek M, Tsilingaridis G, Andreasen JO (2008) Survival of 534 incisors after intra alveolar root fracture in patients aged 7–17 years. DentTraumatol 24:379–387
Yates JA (1992) Root fractures in permanent teeth: a clinical review, vol 25. InternationalEndodonticsJournal, Oxford, pp 150–157
Caliskan MK, Pehlivan Y (1996) Prognosis of root-fractured permanent incisors. Endodontics Dent Traumatol Cph 12(3):129–136. https://doi.org/10.1111/j.1600-9657.1996.tb00111.x
Welbury R, Kinirons MJ, Day P, Humphreys K, Gregg TA (2002) Outcomes for root-fractured permanent incisors: a retrospective study. PediatrDent 2:98–102
Cvek M, Andreasen JO, Borum MK (2001) Healing of 208 intra-alveolar root fractures in patients aged 7–17 years. DentTraumatol 17:53–62
Feely L, Mackie IC, Macfarlane T (2003) An investigation of root-fractured permanent incisor teeth in children. DentTraumatol 19:52–54
Andreasen FM, Andreasen JO, Cvek M, Mejare I (2004) Healing of 400 intra alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dental Traumatology, Copenhagen, 20:203 – 11. https://doi.org/10.1111/j.1600-9657.2004.00278.x
Majorana A, Pasini S, Bardellini E, Keller E (2002) Clinical and epidemiological study of traumatic root fractures. Dent Traumatol 18:77–80. https://doi.org/10.1034/j.1600-9657.2002.180206.x
Zachrisson BU, Jacobsen I (1975) Long-term prognosis of 66 permanent anterior teeth with root fracture, vol 83. ScandinavianJournalDentistryResearch, Copenhagen, pp 345–354
Isaksson et al (2020) Effect of splinting times on the healing of intra-alveolar root fractures in 512 permanent teeth in humans: a scandinavian multicenter study. Dent Traumatol Cph 37:672–676. https://doi.org/10.1111/edt.12683
Andreasen JO, Ahrensburg SS, Tsilingaridis G (2012) Root fractures: the influence of type of healing and location of fracture on tooth survival rates- an analysis of 492 cases. DentalTraumatol 28:404–409
Diangelis AJ et al (2012) International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fracturesandluxationsofpermanentteeth. In: DentTraumatol, 28:2–12
Bastos JV, Goulart EM, Côrtes MIS (2014) Pulpal response to sensibility tests after traumaticdental injuries in permanent teeth. Dent Traumatol 30(3):188–192
Andreasen FM, Andreasen JO (1985) Diagnosis of luxation injuries. The importance of standardized clinical, radiographic and photographic techniques in clinical investigation. EndodDentTraumatol 1:160–169
Iqbal MK, Kim S (2008) A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J Endod 34:519–529
Rosenquist B, Grenthe B (1996) Immediate placement of implants into extraction sockets: implant survival. Int J Oral MaxillofacImplants 11:205–209
Acknowledgements
The authors confirm contribution to the paper as follows: Study conception and design: N. O. M Pedrosa, J.V. Bastos; Analysis and interpretation of results: N.O.M Pedrosa, R. A Santos, E.A. Colosimo, J.V. Bastos; Draft manuscript preparation: N. O. M Pedrosa, S.C. Coste, J.V. Bastos. All authors have reviewedand approved the final version of the manuscript.
Funding
No funding was obtained for this study, with the exception of scholarships provided to undergraduate and postgraduate students. This study received support fromCoordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), a Brazilian funding agency.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: Study conception and design: N.O.M Pedrosa, J.V. Bastos; Analysis and interpretation of results: N.O.M Pedrosa, R. A. Santos. Colosimo, J.V. Bastos; Draft manuscript preparation: N.O.M. Pedrosa, S.C. Coste, J.V. Bastos. All authors have revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Study approval was obtained from COEP-UFMG − 4.384.144.
Patient consent statement
All study participants and/or their legal guardians have provided consent and signed the terms of consent and assent for participation in the study and authorization to use their data in the research. These documents will be made available upon request.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Permission to reproduce material from other sources
Not applicable.
Clinical trial registration
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pedrosa, N., Santos, R., Coste, S. et al. Healing and long-term prognosis of root-fractured permanent teeth: a retrospective longitudinal study. Clin Oral Invest 28, 209 (2024). https://doi.org/10.1007/s00784-024-05581-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05581-x