Abstract
Objectives
Three distinct models were utilized to investigate the combined impacts of serum aldehyde exposure and periodontitis.
Materials and methods
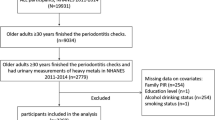
We performed a cross-sectional analysis using data from 525 participants in the 2013–2014 National Health and Nutrition Examination Survey (NHANES). The directed acyclic graphs (DAG) were used to select a minimal sufficient adjustment set of variables (MSAs). To investigate the relationship between aldehydes and periodontitis, we established three models including multiple logistic regression model, restricted cubic spline (RCS) model, and Bayesian kernel machine regression (BKMR) model.
Results
After taking all covariates into account, the multiple logistic regression model revealed that elevated concentrations of isopentanaldehyde and propanaldehyde were strongly associated with periodontitis (isopentanaldehyde: OR: 2.38, 95% CI: 1.34–4.23; propanaldehyde: OR: 1.51, 95% CI: 1.08–2.13). Furthermore, the third tertile concentration of isopentanaldehyde was associated with a 2.04-fold increase in the incidence of periodontitis (95% CI: 1.05–3.95) compared to the first tertile concentration, with a P for trend = 0.04. RCS models showed an “L”-shaped relationship between isopentanaldehyde and periodontitis (P for nonlinear association < 0.01), with inflection point of 0.43 ng/mL. BKMR identified a strong connection between mixed aldehydes and periodontitis, with isopentanaldehyde exhibiting the greatest posterior inclusion probability (PIP) with 0.901 and propanaldehyde exhibiting a PIP with 0.775.
Conclusions
Isopentanaldehyde and propanaldehyde are positively associated with the risk of periodontitis.
Clinical relevance
Periodontitis may be associated with exposure to mixed aldehyde. This study emphasizes the important role of aldehydes in primary prevention of periodontitis.




Similar content being viewed by others
Data availability
The data that support the findings of this study are openly available at NHANES—National Health and Nutrition Examination Survey Homepage (cdc.gov).
References
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F et al. (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Clin Periodontol 45(S20). https://doi.org/10.1111/jcpe.12946
Chen MX, Zhong YJ, Dong QQ, Wong HM, Wen YF (2021) Global, regional, and national burden of severe periodontitis, 1990–2019: an analysis of the Global Burden of Disease Study 2019. J Clin Periodontol 48(9):1165–1188. https://doi.org/10.1111/jcpe.13506
Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJL, Marcenes W (2014) Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res 93(11):1045–1053. https://doi.org/10.1177/0022034514552491
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J (2017) Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol 44(5):456–462. https://doi.org/10.1111/jcpe.12732
Slots J (2020) Life-threatening pathogens in severe/progressive periodontitis: focal infection risk, future periodontal practice, role of the Periodontology 2000. Periodontology 2000 84(1):215–216. https://doi.org/10.1111/prd.12375
Teles F, Collman RG, Mominkhan D, Wang Y (2022) Viruses, periodontitis, and comorbidities. Periodontology 2000 89(1):190–206. https://doi.org/10.1111/prd.12435
Silva LK, Hile GA, Capella KM, Espenship MF, Smith MM, De Jesús VR, Blount BC (2018) Quantification of 19 aldehydes in human serum by headspace SPME/GC/high-resolution mass spectrometry. Environ Sci Technol 52(18):10571–10579. https://doi.org/10.1021/acs.est.8b02745
Chen Y, Shen X, Li G, Yue S, Liang C, Hao Z (2022) Association between aldehyde exposure and kidney stones in adults. Front Public Health 10:978338. https://doi.org/10.3389/fpubh.2022.978338
Srivastava S, Chandrasekar B, Bhatnagar A, Prabhu SD (2002) Lipid peroxidation-derived aldehydes and oxidative stress in the failing heart: role of aldose reductase. Amer J Physiol Heart Circ Physiol 283(6):2612–2619. https://doi.org/10.1152/ajpheart.00592.2002
O’Brien PJ, Siraki AG, Shangari N (2005) Aldehyde sources, metabolism, molecular toxicity mechanisms, and possible effects on human health. Crit Rev Toxicol 35(7):609–662. https://doi.org/10.1080/10408440591002183
Lu X, Gong C, Lv K, Zheng L, Li B, Zhao Y, Lu H, Wei T, Huang J, Li R (2022) Impacts of combined exposure to formaldehyde and PM2.5 at ambient concentrations on airway inflammation in mice. Environ Pollut 315:120234. https://doi.org/10.1016/j.envpol.2022.120234
Lopes Castro MM, Nascimento PC, Souza-Monteiro D, Santos SM, Arouck MB, Garcia VB, de Araújo RF, de Araujo AA, de Balbinot GS, Collares FM et al (2020) Blood oxidative stress modulates alveolar bone loss in chronically stressed rats. Int J Molec Sci 21(10):3728. https://doi.org/10.3390/ijms21103728
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ (2012) Update of the case definitions for population-based surveillance of periodontitis. J Periodontol 83(12):1449–1454. https://doi.org/10.1902/jop.2012.110664
Sung C-E, Huang R-Y, Cheng W-C, Kao T-W, Chen W-L (2019) Association between periodontitis and cognitive impairment: analysis of national health and nutrition examination survey (NHANES) III. J Clin Periodontol 46(8):790–798. https://doi.org/10.1111/jcpe.13155
Xu C, Liang J, Xu S, Liu Q, Xu J, Gu A (2020) Increased serum levels of aldehydes are associated with cardiovascular disease and cardiovascular risk factors in adults. J Hazard Mater 400:123134. https://doi.org/10.1016/j.jhazmat.2020.123134
Textor J, Hardt J, Knüppel S (2011) DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology 22(5):745. https://doi.org/10.1097/EDE.0b013e318225c2be
Harre FE, Lee KL, Pollock BG (1988) Regression models in clinical studies: determining relationships between predictors and response. JNCI J Nat Cancer Ins 80(15):1198–1202. https://doi.org/10.1093/jnci/80.15.1198
Bobb JF, Valeri L, Claus Henn B, Christiani DC, Wright RO, Mazumdar M, Godleski JJ, Coull BA (2015) Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics 16(3):493–508. https://doi.org/10.1093/biostatistics/kxu058
Sczepanik FSC, Grossi ML, Casati M, Goldberg M, Glogauer M, Fine N, Tenenbaum HC (2020) Periodontitis is an inflammatory disease of oxidative stress: we should treat it that way. Periodontology 2000 84(1):45–68. https://doi.org/10.1111/prd.12342
Morinaga T, Hasegawa G, Koyama S, Ishihara Y, Nishikawa T (2010) Acute inflammation and immunoresponses induced by ortho-phthalaldehyde in mice. Arch Toxicol 84(5):397–404. https://doi.org/10.1007/s00204-010-0512-1
Duan J, Xie J, Deng T, Xie X, Liu H, Li B, Chen M (2020) Exposure to both formaldehyde and high relative humidity exacerbates allergic asthma by activating the TRPV4-p38 MAPK pathway in Balb/c mice. Environ Pollut 256:113375. https://doi.org/10.1016/j.envpol.2019.113375
Luo J, Shi R (2004) Acrolein induces axolemmal disruption, oxidative stress, and mitochondrial impairment in spinal cord tissue. Neurochem Int 44(7):475–486. https://doi.org/10.1016/j.neuint.2003.09.006
Sun L, Luo C, Long J, Wei D, Liu J (2006) Acrolein is a mitochondrial toxin: effects on respiratory function and enzyme activities in isolated rat liver mitochondria. Mitochondrion 6(3):136–142. https://doi.org/10.1016/j.mito.2006.04.003
Govindaraj P, Khan NA, Gopalakrishna P, Chandra RV, Vanniarajan A, Reddy AA, Singh S, Kumaresan R, Srinivas G, Singh L et al (2011) Mitochondrial dysfunction and genetic heterogeneity in chronic periodontitis. Mitochondrion 11(3):504–512. https://doi.org/10.1016/j.mito.2011.01.009
Sun X, Mao Y, Dai P, Li X, Gu W, Wang H, Wu G, Ma J, Huang S (2017) Mitochondrial dysfunction is involved in the aggravation of periodontitis by diabetes. J Clin Periodontol 44(5):463–471. https://doi.org/10.1111/jcpe.12711
Dan Dunn J, Alvarez LA, Zhang X, Soldati T (2015) Reactive oxygen species and mitochondria: a nexus of cellular homeostasis. Redox Biol 6:472–485. https://doi.org/10.1016/j.redox.2015.09.005
Sirisereephap K, Maekawa T, Tamura H, Hiyoshi T, Domon H, Isono T, Terao Y, Maeda T, Tabeta K (2022) Osteoimmunology in periodontitis: local proteins and compounds to alleviate periodontitis. Int J Mol Sci 23(10):5540. https://doi.org/10.3390/ijms23105540
Konopka T, Król K, Kopeć W, Gerber H (2007) Total antioxidant status and 8-hydroxy-2’-deoxyguanosine levels in gingival and peripheral blood of periodontitis patients. Arch Immunol Ther Exp 55(6):417–422. https://doi.org/10.1007/s00005-007-0047-1
Tang M-S, Lee H-W, Weng M-W, Wang H-T, Hu Y, Chen L-C, Park S-H, Chan H-W, Xu J, Wu X-R et al (2022) DNA damage, DNA repair and carcinogenicity: tobacco smoke versus electronic cigarette aerosol. Mutat Res, Rev Mutat Res 789:108409. https://doi.org/10.1016/j.mrrev.2021.108409
Tatsumi M, Yanagita M, Yamashita M, Hasegawa S, Ikegami K, Kitamura M, Murakami S (2021) Long-term exposure to cigarette smoke influences characteristics in human gingival fibroblasts. J Periodontal Res 56(5):951–963. https://doi.org/10.1111/jre.12891
Funding
This work was supported by the National Natural Science Foundation of China (81830031, 82270496, 81970969, 82001088, 82101054), the Natural Science Foundation of Jiangsu Province (BK20220309), the Natural Science Foundation of the Jiangsu Higher Education Institutions of China (22KJB320003, 22KJA320002), Chinese Postdoctoral Science Foundation (2022M721677), Young Talents Project of the Orthodontics Committee of the Chinese Stomatological Association (COS-B2021-09), Jiangsu Province Capability Improvement Project through Science, Technology and Education-Jiangsu Provincial Research Hospital Cultivation Unit (YJXYYJSDW4), and Jiangsu Provincial Medical Innovation Center (CXZX202227).
Author information
Authors and Affiliations
Contributions
Xing Cui: Conceptualization; investigation; writing – original draft; data curation. Guirong Zhu: Methodology; investigation; writing – original draft; data curation. Junyan Lin: Software; methodology. Huihan Chu: Software; methodology. Kang Li: Methodology. Liwen Fan: Supervision; validation. Changyue Xing: Supervision; validation. Lin Wang: Conceptualization; funding acquisition; writing – review and editing. Yongchu Pan: Conceptualization; funding acquisition; writing – review and editing; project administration. All authors have given their final approval and agree to be accountable for the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The cohort included in this study received approval of Ethics Review Board of the National Center for Health Statistics to enroll patients, and all participants provided written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cui, X., Zhu, G., Lin, J. et al. The association of aldehyde exposure with the risk of periodontitis: NHANES 2013–2014. Clin Oral Invest 28, 29 (2024). https://doi.org/10.1007/s00784-023-05451-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05451-y