Abstract
Objectives
To determine whether intravenous (IV) sedation would contribute to the stabilization of patients’ hemodynamics during periodontal and oral surgical procedures, and to evaluate the patient-reported outcome measures (PROMs).
Materials and methods
Periodontal or oral surgery patients were recruited and distributed into two groups: (1) sedation group (SG): intravenous sedation plus local anesthesia; (2) control group (CG): local anesthesia only. Systolic and diastolic blood pressure (SBP, DBP), heart rate (HR), and oxygen saturation (SaO2), were monitored at 15-min intervals from sitting in the dental chair (baseline) until the end of the treatment. In addition, a subjective assessment of PROMs was obtained through a post-operative questionnaire.
Results
Forty-nine patients (25 in SG and 24 in CG) were included. The highest SBP and DBP were significantly higher in CG compared to the SG (141.1 ± 18.4 and 133.6 ± 15.1, respectively in SBP; and 85.5 ± 11.0 and 82.9 ± 10.1, respectively in DBP), but no mean significant differences were found between groups (P value of 0.85 and 0.72 for systolic and diastolic BP, respectively). HR and SaO2 did not show statistical intra- and inter-group differences. The overall patient satisfaction score was significantly higher in the SG group compared to CG.
Conclusions
Intravenous moderate sedation seems to contribute to the stabilization of patient’s hemodynamics, especially the systolic blood pressure, although small differences have been found.
Clinical relevance
Intravenous sedation seems to contribute to stabilize the hemodynamic values, and enhances the patient satisfaction after periodontal and oral surgical treatment in the dental office.


Similar content being viewed by others
Data availability
The data that supports the findings of this paper is available from the corresponding author upon request.
Notes
(Xylocaine®, Dentsply Sirona, Charlotte, NC, UUEE)
%IBM® SPSS Statistics® 24.0.0 (Chicago, IL)
References
Brand HS, Abraham-Inpijn L (1996) Cardiovascular responses induced by dental treatment. Eur J Oral Sci 104:245–252. https://doi.org/10.1111/j.1600-0722.1996.tb00074.x
Corah NL, Gale EN, Illig SJ (1978) Assessment of a dental anxiety scale. JADA 97:816–819. https://doi.org/10.14219/jada.archive.1978.0394
Shepherd SR, Sims TN, Johnson BW, Hershman JM (1988) Assessment of stress during periodontal surgery with intravenous sedation and with local anesthesia only. J Periodontol 59:147–154. https://doi.org/10.1902/jop.1988.59.3.147
Liau FL, Kok SH, Lee JJ et al (2008) Cardiovascular influence of dental anxiety during local anesthesia for tooth extraction. Oral Surg, Oral Med, Oral Pathol, Oral Radiol Endod 105:16–26. https://doi.org/10.1016/j.tripleo.2007.03.015
Tolas AG, Pflug AE (1939) Halter JB (1982) Arterial plasma epinephrine concentrations and hemodynamic responses after dental injection of local anesthetic with epinephrine. JADA 104:41–43. https://doi.org/10.14219/jada.archive.1982.0114
González-Lemonnier S, Bovaira-Forner M, Peñarrocha-Diago M, Peñarrocha-Oltra D (2011) Relationship between preoperative anxiety and postoperative satisfaction in dental implant surgery with intravenous conscious sedation. Med Oral Patol Oral Cir Bucal 16:e541–e545. https://doi.org/10.4317/medoral.16.e541
Askar H, Misch J, Chen Z, Chadha S, Wang HL (2020) Capnography monitoring in procedural intravenous sedation: a systematic review and meta-analysis. Clin Oral Investig 24:3761–3770. https://doi.org/10.1007/s00784-020-03395-1
Holtzclaw DJ, Hinze F, Burnham JK, Toscano NJ, Shumaker N (2014) Intravenous moderate sedation as an adjunct for periodontal surgery: a retrospective analysis of 964 cases. Clin Adv Periodontics 4:88–93. https://doi.org/10.1902/cap.2013.120103
Malamed SF (1986) Conscious sedation and general anesthesia techniques and drugs used in dentistry. Anesth Progr 33:176
Tomioka S, Uchida D, Eguchi S, Nakajo N (1998) Elimination of hypersensitive gagging reaction to dentistry by propofol at subhypnotic doses. Oral Dis 4:279–280. https://doi.org/10.1111/j.1601-0825.1998.tb00292.x
Seok U, Ji S, Yoo S, Kim J, Kim S, Kim J (2016) A survey of the intravenous sedation status in one provincial dental clinic center for the disabled in Korea. J Dent Anesth Pain Med 16:123–129. https://doi.org/10.17245/jdapm.2016.16.2.123
Yamamoto T, Fujii-Abe K, Fukayama H, Kawahara H (2018) The effect of adding midazolam to propofol intravenous sedation to suppress gag reflex during dental treatment. Anesth Progr 65:76–81. https://doi.org/10.2344/anpr-65-02-03
Taguchi T, Fukuda K, Sekine H, Kakizawa T (2011) Intravenous sedation and hemodynamic changes during dental implant surgery. Int J Oral Maxillofac Implants 26:1303–1308
Ueno D, Sato J, Nejima J et al (2012) Effects of implant surgery on blood pressure and heart rate during sedation with propofol and midazolam. Int J Oral Maxillofac Implants 27:1520–1526
Mohammadi A, Dehkordi NR, Mahmoudi S et al (2022) Effects of drugs and chemotherapeutic agents on dental implant osseointegration: narrative review. Curr Rev. Clin Exp Pharmacol 7 (online ahead of print). https://doi.org/10.2174/2772432817666220607114559
Hillman JD, McFall WT Jr, Gregg JM (1981) Intravenous conscious sedation in the periodontal patient. J Periodontol 52:24–29. https://doi.org/10.1902/jop.1981.52.1.24
Ellis S (1996) Response to intravenous midazolam sedation in general dental practice. Br Dent J 180:417–420. https://doi.org/10.1038/sj.bdj.4809108
Fukayama H, Yagiela JA (2006) Monitoring of vital signs during dental care. Int Dent J 56:102–108. https://doi.org/10.1111/j.1875-595x.2006.tb00081.x
Alemany-Martínez A, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C (2008) Hemodynamic changes during the surgical removal of lower third molars. J Oral Maxillofac Surg 66:453–461. https://doi.org/10.1016/j.joms.2007.06.634
Aeschliman SD, Blue MS, Williams KB, Cobb CM, MacNeill SR (2003) A preliminary study on oxygen saturation levels of patients during periodontal surgery with and without oral conscious sedation using diazepam. J Periodontol 74:1056–1059. https://doi.org/10.1902/jop.2003.74.7.1056
Woods S, McCormack P (2013) Disputing the ethics of research: the challenge from bioethics and patient activism to the interpretation of the Declaration of Helsinki in clinical trials. Bioethics 27:243–250. https://doi.org/10.1111/j.1467-8519.2011.01945.x
Doyle DJ, Garmon EH (2017) American Society of Anesthesiologists classification (ASA class)
Saravia ME, Currie WR, Campbell RL (1987) Cardiopulmonary parameters during meperidine, promethazine, and chlorpromazine sedation for pediatric dentistry. Anesth Prog 34:92–96
Patterson AC, Wadia SA, Lorenz DJ, Stevenson MD (2017) Changes in blood pressure and heart rate during sedation with ketamine in the pediatric ED. Am J Emerg Med 35:322–325. https://doi.org/10.1016/j.ajem.2016.10.019
Sanadhya YK, Sanadhya S, Jalihal S, Nagarajappa R, Ramesh G, Tak M (2013) Hemodynamic, ventilator, and ECG changes in pediatric patients undergoing extraction. J Indian Soc Pedod Prev Dent 31:10–16. https://doi.org/10.4103/0970-4388.112393
Dag C, Bezgin T, Ozalp N, Golcuklu Aydin G (2014) Utility of bispectral index monitoring during deep sedation in pediatric dental patients. J Clin Pediatr Dent 39:68–73
Canpolat DG, Yildirim MD, Aksu R, Kutuk N, Alkan A, Cantekin K (2016) Intravenous ketamine, propofol and propofol-ketamine combination used for pediatric dental sedation: a randomized clinical study. Pak J Med Sci 32:682–687. https://doi.org/10.12669/pjms.323.9834
Eshghi A, Mohammadpour M, Kaviani N, Tahririan D, Akhlaghi N (2016) Comparative evaluation of bispectral index system after sedation with midazolam and propofol combined with remifentanil versus ketamine in uncooperative during dental procedures. Dent Res J (Isfahan) 13:1–6. https://doi.org/10.4103/1735-3327.174688
Ramazani N (2016) Different aspects of general anesthesia in pediatric dentistry: a review. Iran J Pediatr 26:e2613. https://doi.org/10.5812/ijp.2613
Ganzberg S, Pape RA, Beck FM (2002) Remifentanil for use during conscious sedation in outpatient oral surgery. J Oral Maxillofac Surg 60:244–250. https://doi.org/10.1053/joms.2002.30565
Garip H, Gurkan Y, Toker K, Goker K (2007) A comparison of midazolam and midazolam with remifentanil for patient-controlled sedation during operations on third molars. Br J Oral Maxillofac Surg 45:212–216. https://doi.org/10.1016/j.bjoms.2006.06.002
Author information
Authors and Affiliations
Contributions
J. GA: study design and conceptualization, manuscript writing, data interpretation, final revision, final approval.
E. D: data collection, data interpretation, initial draft preparation, final approval.
H. S: data collection, statistical analysis, manuscript writing, illustrations, final revision, final approval.
L. S: study design and conceptualization, final approval.
S. PG: study design and conceptualization, manuscript writing, final approval.
HL. W: study design and conceptualization, critical revision, final approval.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the Research Medical Ethical Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
STROBE statement—Checklist of items that should be included in reports of case-control studies
Item no | Recommendation | Page no | |
|---|---|---|---|
Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | 1 |
(b) Provide in the abstract an informative and balanced summary of what was done and what was found | 2 | ||
Introduction | |||
Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | 3 |
Objectives | 3 | State specific objectives, including any prespecified hypotheses | 4 |
Methods | |||
Study design | 4 | Present key elements of study design early in the paper | 4, 5 |
Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | 4 |
Participants | 6 | (a) Give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls | 5 |
(b) For matched studies, give matching criteria and the number of controls per case | 5 | ||
Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | 6, 7 |
Data sources/ measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | 6, 7 |
Bias | 9 | Describe any efforts to address potential sources of bias | 7 |
Study size | 10 | Explain how the study size was arrived at | 4 |
Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | 7 |
Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | 7 |
(b) Describe any methods used to examine subgroups and interactions | 7 | ||
(c) Explain how missing data were addressed | 7 | ||
(d) If applicable, explain how matching of cases and controls was addressed | 7 | ||
(e) Describe any sensitivity analyses | 7 | ||
Results | |||
Participants | 13* | (a) Report numbers of individuals at each stage of study—e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyzed | 8 |
(b) Give reasons for non-participation at each stage | 8 | ||
(c) Consider use of a flow diagram | Figure 1 | ||
Descriptive data | 14* | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders | 8, 9 |
(b) Indicate number of participants with missing data for each variable of interest | 8 | ||
Outcome data | 15* | Report numbers in each exposure category, or summary measures of exposure | 9 |
Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g., 95% confidence interval). Make clear which confounders were adjusted for and why they were included | 8, 9 |
(b) Report category boundaries when continuous variables were categorized | N/A | ||
(c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | N/A | ||
Other analyses | 17 | Report other analyses done—e.g., analyses of subgroups and interactions, and sensitivity analyses | 8, 9 |
Discussion | |||
Key results | 18 | Summarize key results with reference to study objectives | 9 |
Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | 11,12 |
Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | 9,10,11 |
Generalisability | 21 | Discuss the generalisability (external validity) of the study results | 11,12 |
Other information | |||
Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | 13 |
Appendix B
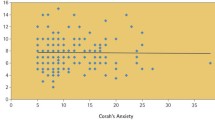
Corah’s Dental Anxiety Scale (DAS) 1 for preoperatory dental anxiety evaluation: (a = 1; b = 2; c = 3; d = 4; e = 5; Total possible = 20: < 9 = mild anxiety; 9–12 = moderate anxiety; 13–14 = high anxiety; 15–20 = severe anxiety (or phobia)
1. If you had to go to the dentist tomorrow for a check-up, how would you feel about it? a. I would look forward to it as a reasonably enjoyable experience b. I wouldn’t care one way or the other c. I would be a little uneasy about it d. I would be afraid that it would be unpleasant and painful e. I would be very frightened of what the dentist would do | |
2. When you are waiting in the dentist's office for your turn in the chair, how do you feel? a. Relaxed b. A little uneasy c. Tense d. Anxious e. So anxious that I sometimes break out in a sweat or almost feel physically sick | |
3. When you are in the dentist’s chair waiting while the dentist gets the drill ready to begin working on your teeth, how do you feel? a. Relaxed b. A little uneasy c. Tense d. Anxious e. So anxious that I sometimes break out in a sweat or almost feel physically sick | |
4. Imagine you are in the dentist’s chair to have your teeth cleaned. While you are waiting and the dentist or hygienist is getting out the instruments which will be used to scrape your teeth around the gums, how do you feel? a. Relaxed b. A little uneasy c. Tense d. Anxious e. So anxious that I sometimes break out in a sweat or almost feel physically sick |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gargallo-Albiol, J., Dastouri, E., Sabri, H. et al. Evaluation of hemodynamic changes and patient-reported outcome measures in surgical therapy with or without intravenous sedation: a prospective controlled clinical study. Clin Oral Invest 27, 7683–7693 (2023). https://doi.org/10.1007/s00784-023-05358-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05358-8