Abstract
Objective
To explore the bacterial and inflammatory variations in oral cancer patients with and without jawbone invasion.
Materials and methods
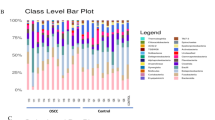
A total of 20 specimens of fresh tumor tissue, including 10 from the tumor-invaded jawbone (JIOC group) and 10 without jawbone invasion (NJIOC group), were collected from oral cancer patients. Meanwhile, 10 specimens from normal oral mucosa were collected from healthy patients (control group). The microbiomic content of each sample was analyzed by 16S rRNA gene sequencing, while the expression of inflammatory cytokines was assessed using protein microarray analysis.
Results
There was a significant difference in β diversity between JIOC and NJIOC groups (P < 0.05), but no difference between NJIOC and control groups. The average relative abundance of Fusobacteria and Spirochaetes was higher, while Firmicutes was lower in the JIOC group than in the NJIOC group (all P < 0.05). The expression of pro-inflammatory cytokines like interleukin (IL)-1α, IL-1β, IL-4, and IL-8 was upregulated in the JIOC group compared with the NJIOC group, while MCP-1 was decreased (all P < 0.05). Slackia spp. and Howardella spp. were positively correlated with IL-4; Odoribacter spp. and Acidaminococcaceae spp. were negatively correlated with IL-4, and Clostridium XIVa spp. was negatively correlated with IL-1α and IL-1β.
Conclusion
Bacterial and inflammatory differences were observed in oral cancer patients with and without jawbone invasion, where the relative abundance of the differential bacteria was associated with the expression of the inflammatory cytokines.
Clinical relevance
This study investigated the changes in the flora during jawbone invasion in oral cancer and its effect on inflammatory factors, elucidating the possible mechanisms of jawbone invasion caused by oral cancer, which may lead to new ideas for the clinical prevention and treatment of jawbone invasion in oral cancer.






Similar content being viewed by others
References
Zhang Y et al (2018) Human oral microbiota and its modulation for oral health. Biomed Pharmacother 99:883–893. https://doi.org/10.1016/j.biopha.2018.01.146
Karpinski TM (2019) Role of oral microbiota in cancer development. Microorganisms 7(1). https://doi.org/10.3390/microorganisms7010020
Sung H et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Wang H et al (2017) Microbiomic differences in tumor and paired-normal tissue in head and neck squamous cell carcinomas. Genome Med 9(1):14. https://doi.org/10.1186/s13073-017-0405-5
Kim J, Amar S (2006) Periodontal disease and systemic conditions: a bidirectional relationship. Odontology 94(1):10–21. https://doi.org/10.1007/s10266-006-0060-6
Elmusrati AA et al (2017) Cancer-associated fibroblasts promote bone invasion in oral squamous cell carcinoma. Br J Cancer 117(6):867–875. https://doi.org/10.1038/bjc.2017.239
Kokemueller H et al (2004) Adenoid cystic carcinoma of the head and neck--a 20 years experience. Int J Oral Maxillofac Surg 33(1):25–31. https://doi.org/10.1054/ijom.2003.0448
Zhang S et al (2023) Gut Prevotellaceae-GABAergic septohippocampal pathway mediates spatial memory impairment in high-fat diet-fed ovariectomized mice. Neurobiol Dis 177:105993. https://doi.org/10.1016/j.nbd.2023.105993
Li A et al (2017) S100A6 promotes cell proliferation in human nasopharyngeal carcinoma via the p38/MAPK signaling pathway. Mol Carcinog 56(3):972–984. https://doi.org/10.1002/mc.22563
Montero PH, Patel SG (2015) Cancer of the oral cavity. Surg Oncol Clin N Am 24(3):491–508. https://doi.org/10.1016/j.soc.2015.03.006
Schultz-Haudt S, Bibby BG, Bruce MA (1954) Tissue-destructive products of gingival bacteria from nonspecific gingivitis. J Dent Res 33(5):624–631. https://doi.org/10.1177/00220345540330050601
Schultz-Haudt S, Bruce MA, Bibby BG (1954) Bacterial factors in nonspecific gingivitis. J Dent Res 33(4):454–458. https://doi.org/10.1177/00220345540330040301
Socransky SS et al (2004) Use of checkerboard DNA-DNA hybridization to study complex microbial ecosystems. Oral Microbiol Immunol 19(6):352–362. https://doi.org/10.1111/j.1399-302x.2004.00168.x
Tezal M, Grossi SG, Genco RJ (2005) Is periodontitis associated with oral neoplasms? J Periodontol 76(3):406–410. https://doi.org/10.1902/jop.2005.76.3.406
Shin YJ et al (2019) Association of periodontitis with oral cancer: a case-control study. J Dent Res 98(5):526–533. https://doi.org/10.1177/0022034519827565
Irfan M, Delgado RZR, Frias-Lopez J (2020) The oral microbiome and cancer. Front Immunol 11:591088. https://doi.org/10.3389/fimmu.2020.591088
Ganly I et al (2019) Periodontal pathogens are a risk factor of oral cavity squamous cell carcinoma, independent of tobacco and alcohol and human papillomavirus. Int J Cancer 145(3):775–784. https://doi.org/10.1002/ijc.32152
Hou LT et al (2003) Interleukin-1beta, clinical parameters and matched cellular-histopathologic changes of biopsied gingival tissue from periodontitis patients. J Periodontal Res 38(3):247–254. https://doi.org/10.1034/j.1600-0765.2003.02601.x
Ebrahimi A et al (2011) The prognostic and staging implications of bone invasion in oral squamous cell carcinoma. Cancer 117(19):4460–4467. https://doi.org/10.1002/cncr.26032
Chugal N et al (2011) Molecular characterization of the microbial flora residing at the apical portion of infected root canals of human teeth. J Endod 37(10):1359–1364. https://doi.org/10.1016/j.joen.2011.06.020
Celik ZC et al (2021) The complex microbiome of caries-active and caries-free supragingival plaques in permanent dentition. Niger J Clin Pract 24(10):1535–1540. https://doi.org/10.4103/njcp.njcp_49_21
Johnson ES (1989) Mortality among nonwhite men in the meat industry. J Occup Med 31(3):270–272. https://doi.org/10.1097/00043764-198903000-00015
Li J et al (2016) Probiotics modulated gut microbiota suppresses hepatocellular carcinoma growth in mice. Proc Natl Acad Sci U S A 113(9):E1306–E1315. https://doi.org/10.1073/pnas.1518189113
Cui Y et al (2022) Roles of intestinal Parabacteroides in human health and diseases. FEMS Microbiol Lett 369(1). https://doi.org/10.1093/femsle/fnac072
Zeuthen LH, Christensen HR, Frokiaer H (2006) Lactic acid bacteria inducing a weak interleukin-12 and tumor necrosis factor alpha response in human dendritic cells inhibit strongly stimulating lactic acid bacteria but act synergistically with gram-negative bacteria. Clin Vaccine Immunol 13(3):365–375. https://doi.org/10.1128/CVI.13.3.365-375.2006
Fink LN et al (2007) Distinct gut-derived lactic acid bacteria elicit divergent dendritic cell-mediated NK cell responses. Int Immunol 19(12):1319–1327. https://doi.org/10.1093/intimm/dxm103
Ferreira-Halder CV, Faria AVS, Andrade SS (2017) Action and function of Faecalibacterium prausnitzii in health and disease. Best Pract Res Clin Gastroenterol 31(6):643–648. https://doi.org/10.1016/j.bpg.2017.09.011
Lima SF et al (2022) Transferable immunoglobulin A-coated Odoribacter splanchnicus in responders to fecal microbiota transplantation for ulcerative colitis limits colonic inflammation. Gastroenterology 162(1):166–178. https://doi.org/10.1053/j.gastro.2021.09.061
Hashim D et al (2016) The role of oral hygiene in head and neck cancer: results from International Head and Neck Cancer Epidemiology (INHANCE) consortium. Ann Oncol 27(8):1619–1625. https://doi.org/10.1093/annonc/mdw224
Garlet GP (2010) Destructive and protective roles of cytokines in periodontitis: a re-appraisal from host defense and tissue destruction viewpoints. J Dent Res 89(12):1349–1363. https://doi.org/10.1177/0022034510376402
Ashida H et al (2011) Shigella are versatile mucosal pathogens that circumvent the host innate immune system. Curr Opin Immunol 23(4):448–455. https://doi.org/10.1016/j.coi.2011.06.001
Hiippala K et al (2020) Isolation of anti-inflammatory and epithelium reinforcing Bacteroides and Parabacteroides spp. from a healthy fecal donor. Nutrients 12(4). https://doi.org/10.3390/nu12040935
Pfalzer AC et al (2015) Diet- and genetically-induced obesity differentially affect the fecal microbiome and metabolome in Apc1638N mice. PLoS One 10(8):e0135758. https://doi.org/10.1371/journal.pone.0135758
Papathanasiou E et al (2020) IL-1 superfamily members and periodontal diseases. J Dent Res 99(13):1425–1434. https://doi.org/10.1177/0022034520945209
Graves D (2008) Cytokines that promote periodontal tissue destruction. J Periodontol 79(8 Suppl):1585–1591. https://doi.org/10.1902/jop.2008.080183
Chompunud NA, Ayudhya C et al (2020) Roles of a mast cell-specific receptor MRGPRX2 in host defense and inflammatioN. J Dent Res 99(8):882–890. https://doi.org/10.1177/0022034520919107
Trebec-Reynolds DP et al (2010) IL-1alpha and IL-1beta have different effects on formation and activity of large osteoclasts. J Cell Biochem 109(5):975–982. https://doi.org/10.1002/jcb.22476
Behl Y et al (2008) Activation of the acquired immune response reduces coupled bone formation in response to a periodontal pathogen. J Immunol 181(12):8711–8718. https://doi.org/10.4049/jimmunol.181.12.8711
Goertzen C, Mahdi H, Laliberte C, Meirson T, Eymael D, Gil-Henn H, Magalhaes M (2018) Oral inflammation promotes oral squamous cell carcinoma invasion. Oncotarget. https://doi.org/10.18632/oncotarget.25540
Li Z, Chen L, Qin Z (2009) Paradoxical roles of IL-4 in tumor immunity. Cell Mol Immunol 6(6):415–422. https://doi.org/10.1038/cmi.2009.53
Amarasekara DS et al (2018) Regulation of osteoclast differentiation by cytokine networks. Immune Netw 18(1):e8. https://doi.org/10.4110/in.2018.18.e8
Acknowledgements
The authors also acknowledge the support of Peking University School and the Hospital of Stomatology for data acquisition for Table 1.
Funding
This study was funded by the National Natural Science Foundation of China (81900979 and 81972540), Beijing Municipal Natural Science Foundation (7212137), and the National Clinical Key Discipline Construction Project (PKUSSNKP-202114).
Author information
Authors and Affiliations
Contributions
Yuxing Guo, Yuanning Yang, and Qingxiang Li contributed to the conception, design, and data acquisition; drafted the manuscript; and critically revised the manuscript. Qiao Qiao, Ning Zhao, Hongyuan Huang, and Ying Zhou contributed to the design, data acquisition, drafting the manuscript, and critical revision of the manuscript. Chuanbin Guo contributed to the design, interpretation, drafting of the manuscript, and critical revision of the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the ethics committee of the Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology (PKUSHS). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The participants have consented to the submission of the case report to the journal and signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, Y., Li, Q., Qiao, Q. et al. Bacterial distribution and inflammatory cytokines associated with oral cancer with and without jawbone invasion—a pilot study. Clin Oral Invest 27, 7285–7293 (2023). https://doi.org/10.1007/s00784-023-05319-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05319-1