Abstract
Objectives
Limited studies are available testing through multiple regression models the association between the two main oral diseases: dental caries and periodontitis. The aim of this cross-sectional population-based study was to verify whether dental caries and periodontitis co-occur in a representative sample of the South Korea population.
Materials and methods
A total of 23,405 subjects representative of 36.2 million of adults (KNHANES) were examined. Univariate and multiple regression analyses using 7 different models were applied, controlling for age, gender, smoking status, frequency of toothbrushing, use of interproximal toothbrushes and flossing, educational level, income, gum diseases treatment and tooth filling in the previous year, BMI, Vitamin D serum levels, alcoholism, diabetes status, stress and carbohydrates dietary intake.
Results
In the fully adjusted model, participants with periodontitis had, respectively, a mean of 0.82 (95% CI: 0.41–1.23) and of 0.36 (95% CI: 0.22–0.50) more untreated decayed surfaces and teeth than participants without periodontitis, with an OR to have at least one untreated decayed surface of 1.96 (95% CI: 1.66–2.32). However, cumulative caries experience (DF scores) and periodontitis were not associated.
Conclusions
In this large nationally representative population, periodontitis and untreated dental caries co-occur. However, when considering cumulative caries experience (DF scores), the two diseases do not appear related.
Clinical relevance
In light of their possible co-occurrence, clinicians should implement integrative diagnostic, preventive and treatment strategies for both diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Taken together, periodontitis and dental caries are among the most common diseases of humans and the leading cause of tooth loss [1,2,3]. They can lead to negative impacts upon quality of life, general health, and they pose a major burden on public health systems [4,5,6,7,8,9,10].
Although they exhibit a distinct pathophysiology, the emergence of a bacterial dysbiosis in genetically or environmentally susceptible individuals is the main etiologic factor for both these chronic complex diseases. Other shared determinants of susceptibility have been identified, with oral hygiene, nutrition, social, educational and economic factors providing the highest level of evidence. A plausible link between caries and periodontitis could therefore be hypothesized.
In 2017, the European Federation of Periodontology (EFP) and the European Organisation for Caries Research (ORCA) joined in the 1st European Workshop on Periodontal diseases and Dental Caries with the aim of assessing the interdependency between the two conditions and providing behavioural guidelines to clinicians, researchers and health policy-makers [11,12,13,14,15,16,17,18,19]. In the consensus report of Group 3, a paucity of studies analysing the co-occurrence of dental caries and periodontitis was highlighted [13]. Indeed, only few studies have been published on this topic showing contradictory results, which suggested either a direct association [20], an inverse association [21] or no association [22]. The most robust recent data reported a direct association [23, 24], but limited attempts were made to study whether this association is independent or entirely explainable by the common risk factors, i.e. age, socioeconomic level or access to dental care [25].
Having clear information on the epidemiological relationship between periodontitis and dental caries would result to uttermost importance in order to set individual and population-based prevention strategies, as well as to correctly plan comprehensive oral treatments. Therefore, this cross-sectional population-based study aimed to verify whether dental caries and periodontitis co-occur, and also, in case an association is found, if common risk factors can explain it.
Materials and methods
This nationally representative cross-sectional study was reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines [26, 27].
Study sample: KNHANES V and VI
Data for this study were obtained from the 2010 and 2012 sections of the Fifth Korea National Health And Nutrition Examination Survey (KNHANES V) and from the 2013–2015 sections of KNHANES VI. The 2011 section of KNHANES V was excluded as it didn’t pass the quality control for periodontal evaluation.
KNHANES is a nationwide cross-sectional survey promoted by the Korea Centre for Disease Control and Prevention (KCDC) and conducted on an annually representative sample of the total non-institutionalized South Korea population [28]. Written informed consent was obtained from all participants.
Sampling methods
KNHANES applied a clustered stratified multistage sampling protocol with a rolling survey model.
Each survey initially selected 192 Primary Sampling Units (PSUs) from around 200,000 geographically defined areas in the whole of South Korea. For each targeted PSU, 20 targeted households were chosen through systematic sampling, so that 3840 households were selected. A PSU consisted of approximately 50–60 households. The surveys included all subjects living in the enrolled households, who were at least 1 year old.
Due to statistical purposes, sample weights were set for sample participants. This way the whole South Korea population was represented and the complex survey design, the null response and the post-stratification (performed either by sex and age) were considered.
Survey contents
KNHANES survey consisted of three parts: the health interview, the health examination and the nutrition survey. Further information about the study design and methods are reported elsewhere [28].
Assessment of study variables
A total of 25–30 trained and calibrated public health dentists assessed each year the dental and periodontal status of the participants according to the WHO criteria for oral health surveys [29].
Caries
Dental caries was identified using the WHO criteria as part of the dental health status examination, scoring each dental surface as sound, decayed, missing or filled [29]. They were assessed for each dental surface, evaluating the entire clinical crown including the possibly exposed root. In the fourth simulated screening test, the inter-examiner mean of Kappa values for dental health status among the included cycles was 0.945 (SD: 0.020, range: 0.919–0.981).
For the present analyses, dental caries was expressed at participant-level with measures of extent and prevalence as:
-
Untreated dental caries (decayed):
-
Number/proportion of decayed surfaces/teeth (DS/DT);
-
Presence of at least 1 decayed surface/tooth.
-
-
Treated dental caries (filled):
-
Number/proportion of filled surfaces/teeth (FS/FT);
-
Presence of at least 1 filled surface/tooth.
-
-
Cumulative caries experience (decayed and filled):
-
Number/proportion of cumulative caries experience (DFS/DFT scores);
-
Presence of cumulative caries experience (presence of a DFS/DFT score of at least 1).
-
Periodontitis
The periodontal status of the participants was assessed through the Community Periodontal Index (CPI) [29]. The measurements were performed through the walking probing method with a 0.5 mm ball tipped CPI probe. During probing calibration sessions, the examiners were calibrated to apply 20 g probing force approximately. In the fourth simulated screening test, the inter-examiner mean of Kappa values for periodontal status was 0.754 (SD: 0.120, range: 0.518–0.900).
The dentition was split into six sextants represented by the following tooth numbers (FDI system): 18–14, 13–23, 24–28, 38–34, 33–43 and 44–48. A sextant was examined just in case two or more unscheduled teeth for extraction were present. Ten index teeth were used for the examination: #17, #16, #11, #26, #27, #37, #36, #31, #46, #47 (FDI system). If a sextant missed one of the index teeth, an adjacent tooth was examined. If no adjacent tooth was even present, all remaining teeth of that sextant were considered for examination.
The Community Periodontal Index was scored from 0 to 4 as follows: 0 (healthy), 1 (gingival bleeding after probing), 2 (calculus), 3 (PPD between 3.5 and 5.5 mm) and 4 (PPD > 5.5 mm). The score of the sextant was calculated as its highest score.
For the current analysis, the periodontal status at participant-level was dichotomized into:
-
“No periodontitis” (CPI ≤ 2 in all sextants);
-
“Periodontitis” (CPI ≥ 3 in at least one sextant).
As a sensitivity analysis, a different categorization was also employed, naming it ‘severe periodontitis’, as follows:
-
“No severe periodontitis” (CPI ≤ 3 in all sextants);
-
“Severe periodontitis” (CPI = 4 in at least one sextant).
Covariates
The covariate assessment methods are reported in Appendix S1.
Statistical analyses
All statistical analyses were carried out with a statistical software (SPSS 23.0 software, IBM Corp, Armonk, NY, USA), using analysis for complex samples with a design-based approach [30]. Furthermore, the stratification, the clustering, and the appropriate sample weights were considered in order to generalize the results to the entire South Korea population. All the reported p-values are two-tailed, and the significance was in advance set at p < 0.05. All missing data with any assumption were handled with complete case analyses with covariates adjustment, as for current statistic literature orientation (Table S1) [31].
The statistical plan has been elaborated similarly to previous reports [32,33,34,35]. Briefly, descriptive characteristics regarding all the covariates were summarized for the whole population and categorized for periodontal status. Categorical data were reported as number (%), while continuous variables were reported as mean (Coefficient of Variation — CV).
In order to evaluate the “crude” (unadjusted) association between periodontitis and caries measurements, the preliminary Odds Ratios (ORs) or Mean Differences (MDs) together with 95% confidence intervals (CIs) were obtained and reported together with the relative p-values deriving from an F-test.
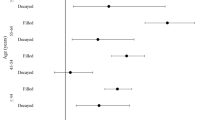
Multiple linear/logistic regression analyses were then applied to examine the association between periodontitis and each caries measure, adjusting for the potential confounders (selected according to the external knowledge) using the following 7 models:
-
a.
Model 1 (only age and gender);
-
b.
Model 2 (Model 1 + smoking status);
-
c.
Model 3 (Model 2 + frequency of toothbrushing + use of interproximal toothbrush + use of flossing);
-
d.
Model 4 (Model 3 + educational level + household income);
-
e.
Model 5 (Model 4 + gum diseases treatment previous year + tooth filling previous year);
-
f.
Model 6 (Model 5 + BMI + Vitamin D serum levels + AUDIT score + diabetes status + stress);
-
g.
Model 7 (Model 6 + carbohydrates dietary intake).
The ORs/MDs (95% CIs) obtained from the multiple regression analyses were reported, as well as the p-values derived from a F-test.
Results
The sampling strategy gave rise to the selection of 50,326 people: 39,964 (79.3%) of them accepted to participate. Of those participants, 37,842 took part to both the health interview and the health examination (75.2% of the total). As previously stated, the final sample weights considered this survey-non-response rate.
The present analysis included only adults (≥ 19 years old) who received the periodontal and caries examination, for a total of 23,405 participants representative of 36.2 million adults (Figure S1).
Descriptive characteristics of the study population
Table 1 provides descriptive statistics of the study participants, both overall and categorized for periodontal status (for both case definitions—CPI ≥ 3 and CPI = 4). Six thousand nine hundred and sixty-seven participants had periodontitis defined as CPI ≥ 3 (weighted N. 9,627,683 — weighted 26.6%) and one thousand nine hundred and sixty-nine participants had periodontitis defined as CPI = 4 (weighted N. 2,714,136 — weighted 7.5%). The mean number of decayed surfaces was 1.57 (0.026), and six thousand nine hundred and seventy-six participants had at least one decayed tooth (weighted N. 11,478,867 — weighted 31.7%).
Periodontitis and untreated dental caries (decayed)
In the unadjusted models, the presence of periodontitis (both case definitions) was directly associated with presence/number of decayed teeth/surfaces.
After controlling for the selected confounders, a significant direct association continued to be present in almost all models. In model 7, participants with periodontitis (CPI ≥ 3) had a mean of 0.82 (95% CI: 0.41–1.23) more decayed surfaces and of 0.36 (95% CI: 0.22–0.50) more decayed teeth than participants without periodontitis, with an OR to have at least one decayed surface/tooth of 1.96 (95% CI: 1.66–2.32) (Table 2). The estimates for severe periodontitis were lower, but mostly still significant (Table 3).
Periodontitis and treated dental caries (filled)
In the crude models, periodontitis (both case definitions) was inversely associated with the presence/number of filled teeth/surfaces. In the multiple regression models the association — when present — was always still inverse. In particular, in Model 7 participants with periodontitis (CPI ≥ 3) had an OR of 0.73 (95% CI: 0.60–0.88) to have at least one filled surface/tooth, while the estimate was not significant for severe periodontitis (OR = 0.81; 95% CI: 0.60–1.10).
Periodontitis and cumulative caries experience (decayed and filled)
In the univariate models, cumulative caries experience was inversely associated with both periodontitis case definitions, with the only exception of percentage of DFS with severe periodontitis.
After controlling for possible confounders, cumulative caries experience and periodontitis (both case definitions) were not associated in all the multiple regression models (Tables 2 and 3).
Discussion
In this study, periodontitis has shown to be independently associated with an increase in the number of untreated decayed teeth and with a decrease in the number of filled teeth. In particular, the subjects with periodontitis had an increase of 96% in the estimated odds to have at least one untreated caries, while they had reduced estimated odds to have at least one filled tooth. Conversely, periodontitis was not associated with cumulative caries experience after adjusting for known common risk factors. Sensitivity analyses for severe periodontitis showed mostly consistent results, however the estimates were generally lower than for CPI ≥ 3 case definition.
Untreated and treated dental caries demonstrated divergent associations with periodontitis in our cohort. This finding is likely to be explained by a possible residual confounding by access to dental care. Indeed, we defined periodontitis based on PPD (CPI index), which is modifiable in nature by periodontal treatment, as dental caries status can be modified by fillings. When looking however at cumulative caries experience, a higher prevalence of both decayed and filled teeth could have also been expected in individuals with periodontitis. Indeed, clinical attachment loss due to periodontal destruction may result in an increased tooth surface area exposed to the oral cavity [36, 37], which confer an intrinsic increased risk for root caries development [38, 39]. However, cumulative caries experience and periodontitis were not associated in our cohort. This finding can be again interpreted in light of the use of PPD to define periodontitis instead of CAL, as well as to the heterogeneous characteristics of supra- and subgingival plaque. Indeed, root surface exposure within a subgingival microenvironment is more likely colonized by an anaerobic proteolityc biofilm than from an acidogenic flora characteristic of dental caries.
Results of investigations on a simultaneous experience of caries and periodontitis have not been consistent so far. On the one hand, authors of the initial quantitative studies comparing the occurrence of cavities and calculus proposed the concept of an inverse relationship between caries and periodontitis [40]. However, several studies were not able to confirm this initial hypothesis, either stating an inaccuracy in supporting an inverse theory [41] or highlighting no association between cumulative caries experience and periodontitis [21, 42, 43]. Similarly to our findings, Albandar et al. highlighted a significant association between the presence of cavities, non-defective and defective fillings, and the progression of periodontitis [20]. Moreover, Mattila et al. in 2010 confirmed again that severe periodontitis and untreated dental caries tended to co-occur in the same subjects [23].
The results from this study should be regarded with caution due the above-mentioned risk of residual confounding (e.g., supragingival plaque, gingival recession) and due to its cross-sectional design, which prevent from any causal inferences. Moreover, a risk of information bias may exist in relation to the assessment of both periodontal status and dental caries. Indeed, periodontitis in KNHANES was assessed by the use of CPI, which is a partial mouth examination protocol only based on PPD [44,45,46]. Similarly, the caries assessment method applied in KNHANES may underestimate the presence and the extent of the disease, since early, non-cavitated lesions could not be detected [47], and radiographic examination was not performed in order to evaluate the involvement of approximal surfaces [48, 49]. Moreover, it does not allow to stage severity of caries and does not differentiate between active and inactive lesions [47]. Finally, part of the missing data might be missing-not-at-random, as they could be lacking due to edentulism caused by either periodontitis or caries. This could potentially have an impact on our results, as edentulous participants could have both periodontitis and dental caries, but they were systematically missing from our data because they had possibly lost their teeth as a result of both diseases. Nonetheless, this study possesses the novelty to having analysed the co-occurrence of treated and untreated dental caries through multivariate analyses. Its external validity is also maximized by the employed sampling procedures, which allow the generalizability of the present findings to the whole non-institutionalized South-Korean population.
The results presented here are advisable for further investigation. These findings need to be replicated in other populations, possibly employing a full-mouth periodontal examination protocol to allow a site-level analysis, and verifying if the results may change depending on whether clinical attachment loss affects the supra-(recession) or sub-(increased PPD) gingival environment. Moreover, the information on dental caries should be completed through radiographs, measures of severity and distinction among coronal and radicular caries [48, 50]. Researchers should take countermeasures to minimize the risk of residual confounding, particularly by collecting detailed data about exposure to periodontal and dental care. Longitudinal and mechanistic studies are also needed.
Conclusions
In this large nationally representative population, treated and untreated dental caries demonstrated divergent associations with periodontitis. However, when considering cumulative caries experience, the two diseases appeared not to be related.
In light of their possible co-occurrence, clinicians should implement integrative diagnostic, preventive and treatment strategies for both diseases.
Data availability
The data that support the findings of this study are listed in the main manuscript and supporting material.
References
GBD 2017 Oral Disorders Collaborators, Bernabe E, Marcenes W et al (2020) Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res 99:362–373. https://doi.org/10.1177/0022034520908533
Frencken JE, Sharma P, Stenhouse L et al (2017) Global epidemiology of dental caries and severe periodontitis - a comprehensive review. J Clin Periodontol 44(Suppl 18):S94-s105. https://doi.org/10.1111/jcpe.12677
Morales A, Strauss FJ, Hämmerle CHF et al (2021) Performance of the 2017 AAP/EFP case definition compared with the CDC/AAP definition in population-based studies. J Periodontol. https://doi.org/10.1002/JPER.21-0276
Marruganti C, Baima G, Aimetti M et al (2023) Periodontitis and low cognitive performance: a population-based study. J Clin Periodontol 50:418–429. https://doi.org/10.1111/jcpe.13779
Antonoglou GN, Romandini M, Meurman JH et al (2023) Periodontitis and edentulism as risk indicators for mortality: results from a prospective cohort study with 20 years of follow-up. J Periodontal Res 58:12–21. https://doi.org/10.1111/jre.13061
Romandini M, Baima G, Antonoglou G et al (2021) Periodontitis, edentulism, and risk of mortality: a systematic review with meta-analyses. J Dent Res 100:37–49. https://doi.org/10.1177/0022034520952401
Baima G, Marruganti C, Sanz M et al (2022) Periodontitis and COVID-19: biological mechanisms and meta-analyses of epidemiological evidence. J Dent Res 00220345221104725. https://doi.org/10.1177/00220345221104725
Ferreira MC, Dias-Pereira AC, Branco-de-Almeida LS et al (2017) Impact of periodontal disease on quality of life: a systematic review. J Periodontal Res 52:651–665. https://doi.org/10.1111/jre.12436
Sabharwal A, Stellrecht E, Scannapieco FA (2021) Associations between dental caries and systemic diseases: a scoping review. BMC Oral Health 21:472. https://doi.org/10.1186/s12903-021-01803-w
Kastenbom L, Falsen A, Larsson P et al (2019) Costs and health-related quality of life in relation to caries. BMC Oral Health 19:187. https://doi.org/10.1186/s12903-019-0874-6
Sanz M, Beighton D, Curtis MA et al (2017) Role of microbial biofilms in the maintenance of oral health and in the development of dental caries and periodontal diseases. Consensus report of group 1 of the Joint EFP/ORCA workshop on the boundaries between caries and periodontal disease. J Clin Periodontol 44(Suppl 18):S5-s11. https://doi.org/10.1111/jcpe.12682
Chapple ILC, Bouchard P, Cagetti MG et al (2017) Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 44:S39–S51. https://doi.org/10.1111/jcpe.12685
Jepsen S, Blanco J, Buchalla W et al (2017) Prevention and control of dental caries and periodontal diseases at individual and population level: consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 44(Suppl 18):S85-s93. https://doi.org/10.1111/jcpe.12687
Tonetti MS, Bottenberg P, Conrads G et al (2017) Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well-being as an essential component of healthy ageing - consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 44(Suppl 18):S135–S144. https://doi.org/10.1111/jcpe.12681
Hujoel PP, Lingström P (2017) Nutrition, dental caries and periodontal disease: a narrative review. J Clin Periodontol 44(Suppl 18):S79–S84. https://doi.org/10.1111/jcpe.12672
Carmo CDS, Ribeiro MRC, Teixeira JXP et al (2018) Added sugar consumption and chronic oral disease burden among adolescents in Brazil. J Dent Res 97:508–514. https://doi.org/10.1177/0022034517745326
Shungin D, Haworth S, Divaris K et al (2019) Genome-wide analysis of dental caries and periodontitis combining clinical and self-reported data. Nat Commun 10:2773. https://doi.org/10.1038/s41467-019-10630-1
Marruganti C, Baima G, Grandini S et al (2023) Leisure-time and occupational physical activity demonstrate divergent associations with periodontitis: a population-based study. J Clin Periodontol. https://doi.org/10.1111/jcpe.13766
Marruganti C, Romandini M, Gaeta C et al (2023) Healthy lifestyles are associated with a better response to periodontal therapy: a prospective cohort study. J Clin Periodontol. https://doi.org/10.1111/jcpe.13813
Albandar JM, Buischi YA, Axelsson P (1995) Caries lesions and dental restorations as predisposing factors in the progression of periodontal diseases in adolescents. A 3-year longitudinal study. J Periodontol 66:249–254. https://doi.org/10.1902/jop.1995.66.4.249
Sewon LA, Parvinen TH, Sinisalo TV et al (1988) Dental status of adults with and without periodontitis. J Periodontol 59:595–598. https://doi.org/10.1902/jop.1988.59.9.595
Kinane DF, Jenkins WM, Adonogianaki E, Murray GD (1991) Cross-sectional assessment of caries and periodontitis risk within the same subject. Community Dent Oral Epidemiol 19:78–81
Mattila PT, Niskanen MC, Vehkalahti MM et al (2010) Prevalence and simultaneous occurrence of periodontitis and dental caries. J Clin Periodontol 37:962–967. https://doi.org/10.1111/j.1600-051X.2010.01620.x
de Araújo NM, Maló P (2017) Prevalence of periodontitis, dental caries, and peri-implant pathology and their relation with systemic status and smoking habits: results of an open-cohort study with 22009 patients in a private rehabilitation center. J Dent 67:36–42. https://doi.org/10.1016/j.jdent.2017.07.013
Strauss F-J, Espinoza I, Stähli A et al (2019) Dental caries is associated with severe periodontitis in Chilean adults: a cross-sectional study. BMC Oral Health 19:278. https://doi.org/10.1186/s12903-019-0975-2
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond Engl 370:1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Vandenbroucke JP, von Elm E, Altman DG et al (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 18:805–835. https://doi.org/10.1097/EDE.0b013e3181577511
Kweon S, Kim Y, Jang M et al (2014) Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43:69–77. https://doi.org/10.1093/ije/dyt228
World Health Organization (1997) Oral health survey: basic methods. World Health Organization, Geneva, Switzerland
Kim Y, Park S, Kim N-S, Lee B-K (2013) Inappropriate survey design analysis of the Korean National Health and Nutrition Examination Survey may produce biased results. J Prev Med Public Health Yebang Uihakhoe Chi 46:96–104. https://doi.org/10.3961/jpmph.2013.46.2.96
Groenwold RHH, Donders ART, Roes KCB et al (2012) Dealing with missing outcome data in randomized trials and observational studies. Am J Epidemiol 175:210–217. https://doi.org/10.1093/aje/kwr302
Romandini M, Shin H-S, Romandini P et al (2020) Hormone-related events and periodontitis in women. J Clin Periodontol 47:429–441. https://doi.org/10.1111/jcpe.13248
Romandini M, Laforí A, Romandini P et al (2018) Periodontitis and platelet count: a new potential link with cardiovascular and other systemic inflammatory diseases. J Clin Periodontol 45:1299–1310. https://doi.org/10.1111/jcpe.13004
Romandini M, Gioco G, Perfetti G et al (2017) The association between periodontitis and sleep duration. J Clin Periodontol 44:490–501. https://doi.org/10.1111/jcpe.12713
Marruganti C, Shin H-S, Sim S-J et al (2023) Air pollution as a risk indicator for periodontitis. Biomedicines 11:443. https://doi.org/10.3390/biomedicines11020443
Romandini M, Soldini MC, Montero E, Sanz M (2020) Epidemiology of mid-buccal gingival recessions in NHANES according to the 2018 World Workshop Classification System. J Clin Periodontol 47:1180–1190. https://doi.org/10.1111/jcpe.13353
Romano F, Perotto S, Baima G et al (2022) Estimates and multivariable risk assessment of mid-buccal gingival recessions in an Italian adult population according to the 2018 World Workshop Classification System. Clin Oral Investig 26:4769–4780. https://doi.org/10.1007/s00784-022-04441-w
Heasman PA, Ritchie M, Asuni A et al (2017) Gingival recession and root caries in the ageing population: a critical evaluation of treatments. J Clin Periodontol 44(Suppl 18):S178-s193. https://doi.org/10.1111/jcpe.12676
Lopez R, Smith PC, Gostemeyer G, Schwendicke F (2017) Ageing, dental caries and periodontal diseases. J Clin Periodontol 44(Suppl 18):S145-s152. https://doi.org/10.1111/jcpe.12683
Karshan M, Rosebury T, Waugh LM (1939) Dental caries among Eskimos of the Kuskokwim area of Alaska: II. Biochemical characteristics of stimulated saliva correlated with dental caries and occurrence of salivary calculus. Am J Dis Child 57:1026–1034. https://doi.org/10.1001/archpedi.1939.01990050032003
Little MF, Scott Wiley H, Dirksen TR (1960) Concomitant calculus and caries. J Dent Res 39:1151–1162. https://doi.org/10.1177/00220345600390061001
Miller SC, Seidler BB (1940) A correlation between periodontal disease and caries. J Dent Res 19:549–562. https://doi.org/10.1177/00220345400190060601
Massler M, Ludwick W, Schour I (1952) Dental caries and gingivitis in males 17 to 20 years old (at the Great Lakes Naval training Center). J Dent Res 31:195–199. https://doi.org/10.1177/00220345520310020501
Kingman A, Albandar JM (2002) Methodological aspects of epidemiological studies of periodontal diseases. Periodontol 2000 29:11–30. https://doi.org/10.1034/j.1600-0757.2002.290102.x
Albandar JM (2011) Underestimation of periodontitis in NHANES surveys. J Periodontol 82:337–341. https://doi.org/10.1902/jop.2011.100638
Tran DT, Gay I, Du XL et al (2014) Assessment of partial-mouth periodontal examination protocols for periodontitis surveillance. J Clin Periodontol 41:846–852. https://doi.org/10.1111/jcpe.12285
Nyvad B, Machiulskiene V, Baelum V (2003) Construct and predictive validity of clinical caries diagnostic criteria assessing lesion activity. J Dent Res 82:117–122. https://doi.org/10.1177/154405910308200208
Ismail AI, Pitts NB, Tellez M et al (2015) The International Caries Classification and Management System (ICCMS) an example of a caries management pathway. BMC Oral Health 15(Suppl 1):S9. https://doi.org/10.1186/1472-6831-15-s1-s9
Becker T, Levin L, Shochat T, Einy S (2007) How much does the DMFT index underestimate the need for restorative care? J Dent Educ 71:677–681
Tonetti MS, Claffey N (2005) Advances in the progression of periodontitis and proposal of definitions of a periodontitis case and disease progression for use in risk factor research. Group C consensus report of the 5th European Workshop in Periodontology. J Clin Periodontol 32(Suppl 6):210–3. https://doi.org/10.1111/j.1600-051X.2005.00822.x
Acknowledgements
The authors wish to kindly thank Dr. Sanghui Kweon (KCDC) and Dr. Yoonjung Kim (KCDC) for providing some precious information about the data collection. The authors also wish to kindly thank the KCDC for providing the data for this study and all its data collectors for their precious work.
The authors declare no conflicts of interest related to this study. This study was self-funded by the authors; however, the data of the Fifth and Sixth Korea National Health And Nutrition Examination Survey (KNHANES V and VI) have been provided from the Korea Center for Disease Control and Prevention (KCDC). KNHANES V and VI have been financially supported by the Health Promotion Fund of Korea (Seoul, South Korea) with administrative support from the Korean Ministry of Health and Welfare (Sejong, South Korea).
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital)
Author information
Authors and Affiliations
Contributions
GB contributed to data interpretation, and to manuscript drafting. HSS contributed to data analysis, and critically revised the manuscript. MA and AL contributed to data interpretation, and to manuscript drafting. MC contributed to data interpretation, and critically revised the manuscript. MR contributed to study conception and design, to data analysis and interpretation, and manuscript drafting. All the authors gave their final approval of the version to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Written informed consent was obtained from all participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Giacomo Baima and Hye-Sun Shin have contributed equally to the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baima, G., Shin, HS., Arrica, M. et al. The co-occurrence of the two main oral diseases: periodontitis and dental caries. Clin Oral Invest 27, 6483–6492 (2023). https://doi.org/10.1007/s00784-023-05253-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05253-2