Abstract
Objectives
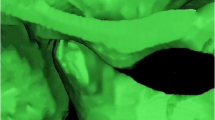
Orthodontic treatment may be associated with temporomandibular disorders through changes in the condylar position. This study aimed to evaluate changes in the condylar position among different amounts of maxillary incisor retraction during orthodontic treatment using cone-beam computed tomography images.
Materials and methods
Fifty-four participants were enrolled and divided into minimal (n = 14), moderate (n = 20), and maximal (n = 20) retraction groups based on the amount of incisor retraction (< 1, 1–6, and > 6 mm, respectively). Changes in condylar position before (T0) and after (T1) orthodontic treatment were assessed for the superior, anterior, posterior, and medial joint spaces (SJS, AJS, PJS, and MJS, respectively). Changes in joint spaces were compared between T0 and T1 in each group using paired t-tests and among the three groups using analysis of variance.
Results
Anterior movement of the condyle was observed in the maximal retraction group with a 0.2 mm decrease in ΔAJS and a 0.2 mm increase in ΔPJS, significantly greater than those in the minimal retraction group. The AJS and PJS showed statistically significant differences between T0 and T1 (P < 0.05) in the maximal retraction group.
Conclusions
The condyle may show a statistically significant but clinically insignificant forward movement in the maximal incisor retraction group, whereas it was relatively stable in the minimal and moderate incisor retraction groups.
Clinical relevance
More attention should be paid to the signs and symptoms of the condyle in patients with excessive incisor retraction during orthodontic treatment.




Similar content being viewed by others
Data Availability
The data underlying this article cannot be publicly shared to protect the privacy of the individuals participating in the study. The data will be shared at a reasonable request to the corresponding author.
References
Liu F, Steinkeler A (2013) Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am 57:465–479
Fraga MR, Rodrigues AF, Ribeiro LC, Campos MJ, Vitral RW (2013) Anteroposterior condylar position: a comparative study between subjects with normal occlusion and patients with Class I, Class II Division 1, and Class III malocclusions. Med Sci Monit 19:903–907
Weinberg LA (1979) Role of condylar position in TMJ dysfunction-pain syndrome. J Prosthet Dent 41:636–643
Imanimoghaddam M, Madani AS, Mahdavi P, Bagherpour A, Darijani M, Ebrahimnejad H (2016) Evaluation of condylar positions in patients with temporomandibular disorders: A cone-beam computed tomographic study. Imaging Sci Dent 46:127–131
Paknahad M, Shahidi S, Iranpour S, Mirhadi S, Paknahad M (2015) Cone-Beam Computed Tomographic Assessment of Mandibular Condylar Position in Patients with Temporomandibular Joint Dysfunction and in Healthy Subjects. Int J Dent 2015:301796
Major P, Kamelchuk L, Nebbe B, Petrikowski G, Glover K (1997) Condyle displacement associated with premolar extraction and nonextraction orthodontic treatment of Class I malocclusion. Am J Orthod Dentofacial Orthop 112:435–440
Artun J, Hollender LG, Truelove EL (1992) Relationship between orthodontic treatment, condylar position, and internal derangement in the temporomandibular joint. Am J Orthod Dentofacial Orthop 101:48–53
Farrar WB, McCarty WL (1982) A Clinical outline of temporomandibular joint diagnosis and treatment, 7th edn. Normandie Study Group for TMJ Dysfunction, pp 84–85
Vasconcelos Filho JO, Menezes AV, Freitas DQ, Manzi FR, Bóscolo FN, de Almeida SM (2007) Condylar and disk position and signs and symptoms of temporomandibular disorders in stress-free subjects. J Am Dent Assoc 138:1251–1255
Sadowsky C (1992) The risk of orthodontic treatment for producing temporomandibular mandibular disorders: a literature overview. Am J Orthod Dentofacial Orthop 101:79–83
McNamara JA Jr (1997) Orthodontic treatment and temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83:107–117
Leite RA, Rodrigues JF, Sakima MT, Sakima T (2013) Relationship between temporomandibular disorders and orthodontic treatment: a literature review. Dental Press J Orthod 18:150–157
Macfarlane TV, Kenealy P, Kingdon HA, Mohlin BO, Pilley JR, Richmond S et al (2009) Twenty-year cohort study of health gain from orthodontic treatment: temporomandibular disorders. Am J Orthod Dentofacial Orthop 135(692):691–698
Alhammadi MS, Fayed MS, Labib A (2017) Three-dimensional assessment of condylar position and joint spaces after maxillary first premolar extraction in skeletal Class II malocclusion. Orthod Craniofac Res 20:71–78
John ZAS, Shrivastav SS, Kamble R, Jaiswal E, Dhande R (2020) Three-dimensional comparative evaluation of articular disc position and other temporomandibular joint morphology in Class II horizontal and vertical cases with Class I malocclusion. Angle Orthod 90:707–714
Lin Y, Lin Y, Fang F, Chen X, He T (2021) The effect of orthodontic treatment on temporomandibular joint morphology in adult skeletal class II deep overbite patients. Am J Transl Res 13:9070–9075
Tariq QUA, Jan A (2023) Condylar Size and Position, Comparison among Different Sagittal Skeletal Relationships: A CBCT Study. J Coll Physicians Surg Pak 33:509–515
Noh KJ, Baik HS, Han SS, Jang W, Choi YJ (2021) Differences in mandibular condyle and glenoid fossa morphology in relation to vertical and sagittal skeletal patterns: A cone-beam computed tomography study. Korean J Orthod 51:126–134
Ikeda M, Miyamoto JJ, Takada JI, Moriyama K (2017) Association between 3-dimensional mandibular morphology and condylar movement in subjects with mandibular asymmetry. Am J Orthod Dentofacial Orthop 151:324–334
Roh YC, Shin SH, Kim SS, Sandor GK, Kim YD (2014) Skeletal stability and condylar position related to fixation method following mandibular setback with bilateral sagittal split ramus osteotomy. J Craniomaxillofac Surg 42:1958–1963
Kuroda S, Yamada K, Deguchi T, Kyung HM, Takano-Yamamoto T (2009) Class II malocclusion treated with miniscrew anchorage: comparison with traditional orthodontic mechanics outcomes. Am J Orthod Dentofacial Orthop 135:302–309
Weissheimer A, Menezes LM, Koerich L, Pham J, Cevidanes LH (2015) Fast three-dimensional superimposition of cone beam computed tomography for orthopaedics and orthognathic surgery evaluation. Int J Oral Maxillofac Surg 44:1188–1196
Feragalli B, Rampado O, Abate C, Macri M, Festa F, Stromei F et al (2017) Cone beam computed tomography for dental and maxillofacial imaging: technique improvement and low-dose protocols. Radiol Med 122:581–588
Liou EJ, Chang PM (2010) Apical root resorption in orthodontic patients with en-masse maxillary anterior retraction and intrusion with miniscrews. Am J Orthod Dentofacial Orthop 137:207–212
Kim JY, Lee SJ, Kim TW, Nahm DS, Chang YI (2005) Classification of the skeletal variation in normal occlusion. Angle Orthod 75:311–319
Janson G, Sathler R, Fernandes TM, Branco NC, Freitas MR (2013) Correction of Class II malocclusion with Class II elastics: a systematic review. Am J Orthod Dentofacial Orthop 143:383–392
Luecke PE 3rd, Johnston LE Jr (1992) The effect of maxillary first premolar extraction and incisor retraction on mandibular position: testing the central dogma of “functional orthodontics.” Am J Orthod Dentofacial Orthop 101:4–12
Wyatt WE (1987) Preventing adverse effects on the temporomandibular joint through orthodontic treatment. Am J Orthod Dentofacial Orthop 91:493–499
Gianelly AA, Hughes HM, Wohlgemuth P, Gildea G (1988) Condylar position and extraction treatment. Am J Orthod Dentofacial Orthop 1988:201–205
Gianelly AA, Cozzani M, Boffa J (1991) Condylar position and maxillary first premolar extraction. Am J Orthod Dentofacial Orthop 99:473–476
De Stefano AA, Guercio-Monaco E, Hernández-Andara A, Galluccio G (2020) Association between temporomandibular joint disc position evaluated by magnetic resonance imaging and mandibular condyle inclination evaluated by computed tomography. J Oral Rehabil 47:743–749
Cho BH, Jung YH (2012) Osteoarthritic changes and condylar positioning of the temporomandibular joint in Korean children and adolescents. Imaging Sci Dent 42:169–174
Paknahad M, Shahidi S (2015) Association between mandibular condylar position and clinical dysfunction index. J Craniomaxillofac Surg 43:432–436
Dalili Z, Khaki N, Kia SJ, Salamat F (2012) Assessing joint space and condylar position in the people with normal function of temporomandibular joint with cone-beam computed tomography. Dent Res J (Isfahan) 9:607–612
Ikeda K, Kawamura A (2009) Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop 135:495–501
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (No. NRF-2020R1F1A1069316).
Author information
Authors and Affiliations
Contributions
Data collection: Sang Ah Cho and Beom-Yon Ko; Data analysis and visualization: Sang Ah Cho, Pi-En Chang, and Yoon Jeong Choi; Writing – original draft: Sang Ah Cho, Pi-En Chang, Yoon Jeong Choi; Writing – review & editing: Pi-En Chang, Beom-Yon Ko, Younjung Park, Jung Jin Park, Yoon Jeong Choi.
All the authors have read and approved the final manuscript. This manuscript has not been published or presented elsewhere in part or in its entirety and is not under consideration by another journal.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board (IRB Approval No.:2-2017-0060) of Yonsei University Dental Hospital.
Owing to the retrospective nature of the study, the review board waived the requirement for written informed consent from the participants.
Conflict of interests
All authors have no financial disclosures or conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, S.A., Chang, PE., Koh, B. et al. Changes in condylar position during orthodontic treatment depending on the amount of incisor retraction: a cone-beam computed tomography study. Clin Oral Invest 27, 5297–5307 (2023). https://doi.org/10.1007/s00784-023-05149-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05149-1