Abstract
Objective
This study evaluated the dimensional and positional osseous temporomandibular joint features in normodivergent facial patterns with and without temporomandibular disorders.
Methods
A total of 165 adult patients were divided into two groups: group 1 (n = 79 patients; 158 joints): temporomandibular disorders patients and group 2 (n = 86 patients; 172 joints): non-temporomandibular disorders patients. Three-dimensional positional and dimensional temporomandibular joint characteristics, including glenoid fossa, mandibular condyles, and joint spaces, were assessed by cone beam computed tomography.
Results
The glenoid fossa positions in the three orthogonal planes and height showed statistical significance between the two studied groups. The temporomandibular disorders patients showed higher horizontal and vertical condyle inclinations while anteroposterior inclination was less, and the condyle was positioned more superior, anterior, and lateral in the glenoid fossa. The condyle width and length showed no significance between the two groups, while condyle height was smaller in temporomandibular disorders patients. Anterior and medial joint spaces increased while the superior and posterior joint spaces reduced in temporomandibular disorders patients.
Conclusion
There were significant differences between the patients with and without temporomandibular joint disorders in terms of mandibular fossa positions and height as well as condylar positions and inclinations in horizontal and vertical planes together with reduced condylar height and reduced posterior and superior joint spaces in the temporomandibular disorders patients.
Clinical relevance
The temporomandibular disorder is a multifactorial disorder in which one of these factors is the dimensional and positional characteristics of the temporomandibular joints; including or excluding this factor requires a comprehensive three-dimensional investigation of patients with TMD compared to the normal group under the condition that the facial pattern is average as a confounding factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The temporomandibular joint (TMJ) is a complex, delicate, and extensively utilized joint by humans. It articulates the mandible with the temporal bone of the human skull to regulate its movements. It has two condyles at both ends of the mandible and functions simultaneously [1]. TMJ has a unique mechanism in which there is no contact between the articular surfaces of the bones with each other. However, they are separated by a disc that serves as a cushion for stress absorption and permits the easy movement of condyles when the oral cavity is opened and closed. This disc splits TMJ into two synovial cavities, with synovial membranes lining them. The articulating surfaces of bones are covered with fibrocartilage, not hyaline cartilage [2].
Temporomandibular disorder (TMD) is a generic term comprising a heterogeneous group of complex diseases of variable and usually multifactorial etiologies affecting the masticatory musculature of the head and neck, osseous structures of the human mandible and TMJ, and soft tissue structures of TMJ such as the disc and its attached ligaments. Injuries involving the mandible, TMJ, or head and neck muscles could result in TMD. Other potential etiologies are teeth grinding or clenching, which increases the pressure on TMJ; disc dislocation; osteoarthritis or rheumatoid arthritis involving TMJ; psychosocial stress and its associated tightening of muscles of the face and jaw; and aging effects [3].
There is high inter-individual variability in TMD-related signs and symptoms; however, they are divided into six major groups: (1) pain dysfunction syndrome, non-dental pain involving the orofacial region, which is the most common TMJ disorder, and these individuals often complain of pain on mastication; (2) joint noise: clicking, crepitation, and grinding; (3) TMJ locking: incapability of complete closing or opening; (4) tender muscles in patient’s face, neck, and a shoulder; (5) ear symptoms: otalgia, tinnitus; and (6) psychosocial complaints [4, 5].
The incidence of TMD had been shown to be higher in the general population (20–75%) compared with an incidence of 2–4% in those who presented to receive therapy [6]. TMD is often presented in the second to the fourth decade, and there are no sex differences in symptoms (1:1). However, there are significantly more female patients than male patients seeking therapy, with a ratio of 7:1 [7].
The recent high-level evidence showed that TMD prevalence in patients seeking orthodontic treatment ranged from 21.1 to 73.3%; the percentage of males and females presenting with TMD varied from 10.6 to 68.1% and 21.2 to 72.4%, respectively [8]. Another recent systematic review and meta-analysis concluded that the prevalence overall meta-analyses for adults/elderly are as follows: TMD (31.1%), disc displacements (19.1%), and degenerative joint disease (9.8%). Furthermore, for children/adolescents, they are as follows: TMD (11.3%), disc displacements (8.3%), and degenerative joint disease (0.4%) [9]. The most recent systematic review with meta-analysis evaluated the prevalence of temporomandibular disorders in children and adolescents using Diagnostic Criteria for Temporomandibular Disorders (DC/TMDs) showed that among 1093 female, 489 (44.7%) presented TMD, while 247/821 male (30%) experienced TMD and overall TMD prevalence in children and adolescence varies between 20 and 60%. Females had a higher prevalence of TMDs compared to males [10].
Many radiographic techniques have been utilized for the assessment of the morphological and positional features of soft and hard tissue components of TMJ using conventional 2D imaging, multidetector computed tomography (MDCT), magnetic resonance imaging (MRI), and computed tomography (CT) [11, 12]. However, the most common limitation of using conventional 2D radiography is the superimposition of neighboring structures of TMJ [13]. Recently, cone beam computed tomography (CBCT) has been utilized to produce high-resolution images with little distortion. It is more rapid with a smaller irradiation dose than CT. The measurement of the length and volume in multiple planes can be obtained by a three-dimensional (3D) CBCT scan, giving a correct diagnosis and good predictability of therapeutic outcomes [14].
The temporomandibular disorder is a multifactorial disorder in which one of these factors are the dimensional and positional characteristics of the temporomandibular joints; including or excluding this factor requires a comprehensive three-dimensional investigation of patients with TMD compared to the normal group under the condition that the facial pattern is normal as a confounding factor. To our knowledge, there was no comparative study conducted that evaluated comprehensively the positional and morphologic structures of TMJ in adult patients with and without TMD. Thus, the current study was designed for 3D evaluation of the dimensional and positional osseous TMJ parameters in normodivergent facial patterns with and without TMD.
Materials and methods
Study design
The current cross-sectional study obtained its approval from the research ethics committee of the Faculty of Dentistry, Cairo University, Egypt (No. 2152012). The procedures were carried out following the relevant laws and regulations. Every patient was informed about the goal and methods of study, and then they provided written consent.
Sample size and selection
The sample size was calculated based on α value of 0.05 and a power of 95% according to Al-Rawi et al. [15] study in which the mediolateral (ML) measurements of the condyle were 18.98 ± 2.55 and 15.81 ± 3.05 mm in the studied groups. The sample size was calculated to be at least 22 joints in each studied category. However, such a number was increased to at least 30 joints in each group.
Patients were considered desirable based on the following general inclusion criteria: (1) age 18–30 years; and (2) patients have all permanent teeth erupted except for the third molars, while the specific inclusion criteria for the normal group were patients without a history of TMD and/or jaw muscles, and painful or limited movement of the mandible; and the specific inclusion criteria for TMD group were patients with a history of TMD including either disc displacement with or without reduction [16]. The exclusion criteria were: (1) patients with a history of growth abnormalities, condylar degenerative illnesses (e.g., erosion, subchondral cysts, and condylar hyperplasia) [17], polyarthritis, acute trauma, or tumors of TMJ; (2) patients with a history of medications which can influence the TMDs; and (3) patients with a history of orthodontic therapy or had orthognathic or TMJ surgeries. One hundred sixty-five patients (330 joints) who met the previously mentioned inclusion and exclusion criteria were selected out of 1063 individuals who were examined at the outpatient clinic of the Orthodontic Department, Faculty of Dentistry, Cairo University, Egypt.
Clinical examination
Two operators (A.A. and M.A.) carried out the clinical examination under the direct supervision of an experienced TMD specialist (M.F.). Additionally, before the start of the research, the measurements of a pilot sample of thirty subjects, which were recorded by the three operators, were calibrated with the specialist’s measurements, and inter-observer reliability (A.A.) was statistically determined. Customized history and examination chart were utilized following the DC/TMDs [16]. Clinical evaluation of the enrolled patients included: (1) TMJ palpation; (2) masticatory muscles evaluation and palpation; (3) mandibular movements evaluation; and (4) TMJ sounds assessment.
The total sample was divided into two groups: group 1: TMD group (79 patients; 158 joints) and group 2: non-TMD group (86 patients; 172 joints). Patients were examined using the examination chart following DC/TMD. The CBCT was used to assess the 3D positional and dimensional characteristics of TMJ, which included the glenoid fossa, mandibular condyles, and the TMJ spaces.
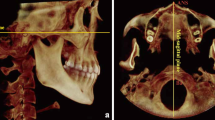
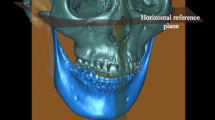
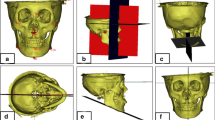
CBCT analysis
Three-dimensional images were acquired by I-CAT CBCT system (Imaging Sciences International, Hatfield, USA) at the Faculty of Dentistry, Cairo University, Egypt. The machine set with the following exposure parameters: 18.54 mAs and 120 kV, and images underwent capture for 8.9 s with a 0.30-mm voxel size, 2 mm slice thickness, and large field of view (17 cm2). CBCT images were captured in Frankfort horizontal (FH) plane reoriented parallel to the floor aided by crossing laser guide, and teeth were occluded in centric occlusion (CO). Then, the midsagittal reference plane was automatically set. This plane was perpendicular to FH plane and passed through Nasion. During the scanning process, patients were informed to avoid swallowing or movement during scanning process.
CBCT images were acquired based on Digital Imaging and Communications in Medicine (DICOM) files and then exported to Invivo Anatomage 5.01 (Anatomage, San Jose, USA) for 3D analysis. The landmarks of craniofacial structures and TMJ were recognized in a 3D view and underwent adjustment in the three orthogonal planes (Table 1 and supplementary material 1) by slice locator option (Figs. 1 and 2). The standardized innovative 3D imaging of all linear and angular measurements of craniofacial images described by Alhammadi et al. [18,19,20] was used in this study and described in Table 2 and supplementary material 2. Positional and dimensional mandibular fossa and condylar osseous parameters relative to skull base reference were evaluated. The analysis included TMJ joint spaces, anterior (AJS), superior (SJS), posterior (PJS), and medial joint space (MJS). The anteroposterior and vertical condylar position inside the joint was calculated based on the formula developed by Pullinger and Hollender [21].
To evaluate the significance of any measurement errors, 30 cases underwent random selection and were measured twice, 2 weeks apart, by the same operator (M.A.) and once by another operator (A.A.) to assess intra- and inter-observer reliability.
Statistical analysis
The data were analyzed by IBM-SPSS program (IBM Corp. Released 2019, IBM SPSS Statistics for Windows V 26.0. Armonk, NY). The reliability and reproducibility of measurements were analyzed utilizing the intra-class correlation coefficient (ICC), and the quantitative data were first tested for normality by Shapiro–Wilk’s test and were considered normally distributed if P > 0.050 and all data were represented as means ± standard deviations (SDs). An independent t-test was utilized to compare normally distributed quantitative data between both groups. The significance of a result was set at P-value less than 0.05.
Results
Regarding the baseline anteroposterior (AP) and vertical (V) skeletal measurements, no significant differences existed between both groups indicating comparable skeletal class and normodivergent facial patterns. The mean point A-Nasion-point B (ANB) angles in TMD and non-TMD groups were 3.9 ± 2.58 and 3.3 ± 2.97°, respectively, and the mean mandibular plane to Sella-Nasion (MP/SN) angles were 34.68 ± 3.39 and 34.97 ± 3.41° in TMD and non-TMD groups, respectively (Table 3).
For mandibular fossa measurements (Table 4), the mandibular fossa positions, the AP, V, and ML, revealed significant differences among both groups. The mandibular fossa parameters showed no statistical significant differences regarding glenoid fossa width (GFW), mandibular fossa anterior wall inclination (AFLHP), and mandibular fossa posterior wall inclination (PFLHP). In contrast, glenoid fossa height (GFH) showed statistical significance between both groups.
The mean mandibular condyle inclination (Table 5) in horizontal (HCI) and vertical (VCI) planes demonstrated highly significant differences between both groups with P < 0.000, while anteroposterior mandibular condyle inclination (APCI) showed no significance in which horizontal and vertical condyle inclinations relative to horizontal (HP) and vertical planes (VP) were higher in the TMD group (6.32 ± 3.60 and 79.39 ± 6.20°, respectively) than the non-TMD group (4.41 ± 2.48 and 75.08 ± 6.60°, respectively). However, anteroposterior condyle inclination relative to the midsagittal plane (MSP) was lesser in the TMD group (73.76 ± 6.50°) than in the non-TMD group (75.50 ± 5.29°).
As regards condylar positions (Table 5), relative to the basal reference, our results revealed highly significant differences between both groups in all planes; the TMD group showed more superior (VCP), posterior (APCP), and lateral (MLCP) condyle positions (1.80 ± 1.24, 4.51 ± 2.37, and 41.48 ± 4.04 mm, respectively) as compared to the non-TMD group (3.42 ± 1.57, 5.73 ± 2.41, and 39.18 ± 2.36 mm, respectively).
For the mandibular condyle parameters (Table 5), the results showed no statistical significant differences in the condyle length and width in both groups, while the condyle height was statistically significant, although all the condylar parameters were greater among non-TMD patients than the TMD patients. Regarding the intra-joint condylar positions, the anteroposterior (APJCP) and vertical (VJCP) condyle positions showed highly significant differences among groups in which the condylar position was more superior (3.28 ± 1.05 mm) in the TMD group in comparison with the non-TMD group (3.74 ± 0.93 mm) and more posterior in the TMD group (− 7.09 ± 20.84 mm) than in the non-TMD group (11.88 ± 17.75 mm).
In the measurements of joint spaces (Table 6), our findings revealed significant differences between the two groups. TMD group showed increased anterior (AJS) (2.73 ± 0.70 mm) and medial (MJS) (3.95 ± 1.08 mm) joint spaces relative to non-TMD patients (2.20 ± 0.73 and 2.73 ± 0.88 mm, respectively). In comparison, the superior (SJS) and posterior (PJS) joint spaces were reduced in the TMD group (3.74 ± 0.93 and 2.41 ± 0.82 mm) as compared to the non-TMD group (4.27 ± 1.37 and 2.84 ± 1.04 mm).
Discussion
TMD is a common health issue, and it is an umbrella term that includes a variety of signs and symptoms influencing muscles of mastication, TMJ, and dentoalveolar components [22]. In this aspect, it is considered a musculoskeletal disorder causing orofacial pain of non-dental origin affecting the head, face, and related structures [23]. TMD is a multifactorial disease with numerous direct and indirect causal factors [24].
The present study investigated, in a 3D view, dimensional and positional osseous characteristics of TMJ structures in normodivergent facial patterns with and without temporomandibular disorders following an established method by Alhammadi et al. [20, 25].
Several studies [19, 26, 27] evaluated the association between the condyle and mandibular fossa in the hypodivergent and hyperdivergent skeletal patterns. On the other hand, other studies [15, 16, 28] evaluated TMJ features in patients with different forms of TMD: myalgia, disc displacement with reduction, and disc displacement without reduction. However, 3D dimensional and positional osseous characteristics of TMJ structures in normodivergent skeletal patterns have not been evaluated comprehensively in patients with or without TMDs. In this study, all participants have comparable skeletal patterns without anteroposterior or vertical discrepancies to ensure skeletal demographic standardization with minimal variations.
In the current study, the mandibular condyle inclination in horizontal and vertical planes revealed highly significant differences between both groups. This is partly similar to De Stefano et al. [29] study who indicated that mandibular condyle inclination might differ in TMJs with different disc positions, and they stated that a more medial horizontal condylar inclination and a more posterior sagittal condylar inclination were linked to TMDs like disc displacement without reduction. Also, Busato et al. [30] and Raustia et al. [31] considered that horizontal condyle inclinations were significantly different between subjects with normal joints and those having disc incoordination, whereas Amorin et al. [32] revealed no association between the horizontal inclination of the mandibular condyle and disc displacement. This finding infers that the change in the disc position in TMD patients is mainly by displacement in the anterior and medial direction leading to horizontal and vertical inclination changes as a result of the bone remodeling, respectively. This change is reflected in the remodeling of the glenoid fossa in the three dimensions, as shown in the current results too.
Our study revealed that the condyle in TMD patients was more superiorly, posteriorly, and laterally positioned in the glenoid fossa; this is shown in both aspects, the position relative to the fixed basal reference planes and within the joint measurements. This might indicate that the long-standing positioning of the disc in the anteromedial position pushes the condyle into posterior and lateral position, and the superior joint space that was occupied by the disc above the condyle head becomes less due to the same dynamic effect, so the condyle moved vertically to occupy this space. This is in agreement with Dalili et al. [33] who stated that the centric location of the condyle in the mandibular fossa was a common position. But, this disagreed with Alhammadi et al. [20] who reported that the condyles in non-TMD individuals were more positioned in a non-centric location in the glenoid fossa. Also, Imanimoghaddam et al. [34] and Incesu et al. [35] sated that the posterior condylar position was the most common position among TMD cases. These significant changes also reflected by the significant differences of the mandibular fossa position in the three planes of space between both groups; this might have occurred as a secondary change in the form of bone remodeling following the condylar positional changes in the three planes. The most significant condylar positional change was in the vertical direction, which was also demonstrated by the significant increase in the mandibular fossa height in the TMD group in comparison with the normal patients.
The current findings showed no statistically significant differences in the condyle width in both studied groups. Likewise, Imanimoghaddam et al. [34] reported a non-significant relationship between anterior disc displacement with reduction and alterations in condylar width too. On the contrary, Okur et al. [36] evaluated condylar width by CT, and a significant difference was revealed between normal and symptomatic cases. Also, Seo et al. [37] demonstrated that the condyle width was less in anterior disc displacement with reduction in comparison with asymptomatic patients.
Regarding the condylar length, our findings did not demonstrate any significant difference between normal subjects and TMD patients, similar to Imanimoghaddam et al. [34] results who reported a non-significant difference regarding condyle length between normal TMJs and patients with anterior disc displacement with reduction. However, these results are not consistent with the study conducted by Yasa and Akgül [28]; they revealed that the condylar length was smaller among anterior disc displacement with reduction patients than in asymptomatic patients.
In our study, condyle height was less among TMD cases compared with normal subjects; this is consistent with Mohamed et al. [38] who reported that condylar height was decreased in TMD group in comparison with normal subjects and disagreed with the finding of Seo et al. [37] who stated that condyle height did not show a significant difference between healthy joints and patients with anterior disc displacement with reduction. Mathematically, this change is considered as false positive due to the use of the local reference line in this measurement aided by a change in the vertical condylar position relative to this line rather than the actual change in the condylar length.
The superior and posterior joint spaces showed a significant reduction, while anterior and medial joint space increased among TMD patients. This was in agreement with Yasa and Akgül [28] who reported a significant difference in joint space measurements between normal and TMJ dysfunction cases but was inconsistent with Imanimoghaddam et al. [34] who conducted that superior and posterior joint spaces showed no significant differences between normal subjects and TMD patients (P = 0.36 and P = 0.7, respectively). This is another indication that the changes in the disc position affect the whole TMJ system. In this case, the reduction in superior and posterior joint spaces is another indication of the condyle’s superior and anterior reactive positioning, respectively. At the same time, the increased anterior and medial joint spaces reflect the posterior and lateral change in the condyle position, as evident elsewhere.
One of the limitations of this study is that it is limited to adult patients, and including growing patients may change the finding of this study; another limitation is that it is limited to specific ethnic groups, and the finding cannot be generalized to other ethnicities or populations. The assessment was limited to the osseous structures; the use of MRI to examine the soft tissue component is recommended in similar future studies.
Conclusion
The findings of this study revealed a significant association between TMDs and TMJ positional and morphological osseous characteristics; the patients diagnosed with TMD showed significantly different mandibular fossa positions in all planes, fossa height, condylar positions, and the horizontal and vertical condylar inclinations. The AJS and MJS increased while the SJS and PJS reduced in TMDs patients.
References
Iturriaga V, Bornhardt T, Velasquez N (2023) Temporomandibular joint: review of anatomy and clinical implications. Dent Clin North Am 67(2):199–209
Wadhwa S, Kapila S (2008) TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ 72(8):930–947
Ingawalé S, Goswami T (2009) Temporomandibular joint: disorders, treatments, and biomechanics. Ann Biomed Eng 37(5):976–996
Detamore MS, Athanasiou KA (2003) Structure and function of the temporomandibular joint disc: implications for tissue engineering. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 61(4):494–506
Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF (2005) Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain 9(6):613–633
Kapos FP, Exposto FG, Oyarzo JF, Durham J (2020) Temporomandibular disorders: a review of current concepts in aetiology, diagnosis and management. Oral Surg 13(4):321–334
Gray RJ, Davies SJ, Quayle AA (1994) A clinical approach to temporomandibular disorders. 1. Classification and functional anatomy. Br Dent J 176(11):429–435
Lai YC, Yap AU (2020) Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: a systematic review. J Oral Rehabil 47(2):270–280
Valesan LF, Da-Cas CD, Réus JC, Denardin ACS, Garanhani RR, Bonotto D, Januzzi E, de Souza BDM (2021) Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Invest 25(2):441–453
Minervini G, Franco R (2023) Prevalence of temporomandibular disorders in children and adolescents evaluated with Diagnostic Criteria for Temporomandibular Disorders: a systematic review with meta-analysis. J Oral Rehabil 50(6):522–530
Almashraqi AA, Ahmed EA, Mohamed NS, Halboub ES (2018) An MRI evaluation of the effects of qat chewing habit on the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol 126(3):272-282.e272
Jian-rong C, Shui-qing D, Liang C, Jia-jia H, Rong-xing Q (2022) Imaging features of temporomandibular joint disorder: comparison of the efficacy of cone-beam CT, MRI. China J Oral Maxillofac Surg 20(3):273
Kurita H, Kojima Y, Nakatsuka A, Koike T, Kobayashi H, Kurashina K (2004) Relationship between temporomandibular joint (TMJ)-related pain and morphological changes of the TMJ condyle in patients with temporomandibular disorders. Dentomaxillofac Radiol 33(5):329–333
Sümbüllü MA, Cağlayan F, Akgül HM, Yilmaz AB (2012) Radiological examination of the articular eminence morphology using cone beam CT. Dentomaxillofac Radiol 41(3):234–240
Al-Rawi NH, Uthman AT, Sodeify SM (2017) Spatial analysis of mandibular condyles in patients with temporomandibular disorders and normal controls using cone beam computed tomography. Eur J Dent 11(1):99–105
Aboalnaga AA, Amer NM, Alhammadi MS, Fayed MMS (2022) Positional and dimensional TMJ characteristics in different temporomandibular disorders: a cross-sectional comparative study. Cranio 21:1–9
Barngkgei I, Halboub E (2019) Effect of bisphosphonate treatment on the jawbone: an exploratory study using periapical and panoramic radiographic evaluation. Oral Radiol 35(2):159–170
Abdulqader AA, Ren L, Alhammadi M, Abdu ZA, Mohamed AAS (2019) Three-dimensional analysis of temporomandibular joint in Chinese adults with normal occlusion and harmonious skeleton. Oral Radiol 36(4):371–382
Alhammadi MS, Fayed MMS, Labib A (2016) Comprehensive three-dimensional cone beam computed tomography analysis of the temporomandibular joint in different vertical skeletal facial patterns. J World Fed Orthod 5(1):9–17
Alhammadi MS, Fayed MS, Labib A (2016) Three-dimensional assessment of temporomandibular joints in skeletal class I, class II, and class III malocclusions: cone beam computed tomography analysis. J World Fed Orthod 5(3):80–86
Pullinger A, Hollender L (1986) Variation in condyle-fossa relationships according to different methods of evaluation in tomograms. Oral Surg Oral Med Oral Pathol 62(6):719–727
Sari S, Sonmez H (2002) Investigation of the relationship between oral parafunctions and temporomandibular joint dysfunction in Turkish children with mixed and permanent dentition. J Oral Rehabil 29(1):108–112
Christidis N, Lindström Ndanshau E, Sandberg A, Tsilingaridis G (2019) Prevalence and treatment strategies regarding temporomandibular disorders in children and adolescents—a systematic review. J Oral Rehabil 46(3):291–301
Michelotti A, Iodice G (2010) The role of orthodontics in temporomandibular disorders. J Oral Rehabil 37(6):411–429
Almaqrami BS, Alhammadi MS, Tang B, ALyafrusee ES, Hua F, He H, (2021) Three-dimensional morphological and positional analysis of the temporomandibular joint in adults with posterior crossbite: a cross-sectional comparative study. J Oral Rehabil 48(6):666–677
Al-Hadad SA, Alyafrusee ES, Abdulqader AA, Al-Gumaei WS, Al-Mohana R, Ren L (2022) Comprehensive three-dimensional positional and morphological assessment of the temporomandibular joint in skeletal class II patients with mandibular retrognathism in different vertical skeletal patterns. BMC Oral Health 22(1):149
Park IY, Kim JH, Park YH (2015) Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern. Korean J Orthod 45(2):66–73
Yasa Y, Akgül HM (2018) Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol 34(1):31–39
De Stefano AA, Guercio-Monaco E, Hernández-Andara A, Galluccio G (2020) Association between temporomandibular joint disc position evaluated by magnetic resonance imaging and mandibular condyle inclination evaluated by computed tomography. J Oral Rehabil 47(6):743–749
Busato A, Vismara V, Bertele L, Zollino I, Carinci F (2010) Relation between disk/condyle incoordination and joint morphological changes: a retrospective study on 268 TMJs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110(3):e34-40
Raustia AM, Pyhtinen J (1990) Morphology of the condyles and mandibular fossa as seen by computed tomography. J Prosthet Dent 63(1):77–82
Amorim MY, Alves MGO, Almeida JD, Montesinos GAP, Costa ALF (2019) Inclination of the condylar long axis is not related to temporomandibular disc displacement. J Investig Clin Dent 10(1):e12375
Dalili Z, Khaki N, Kia SJ, Salamat F (2012) Assessing joint space and condylar position in the people with normal function of temporomandibular joint with cone-beam computed tomography. Dent Res J 9(5):607–612
Imanimoghaddam M, Madani AS, Mahdavi P, Bagherpour A, Darijani M, Ebrahimnejad H (2016) Evaluation of condylar positions in patients with temporomandibular disorders: a cone-beam computed tomographic study. Imaging Sci Dent 46(2):127–131
Incesu L, Taşkaya-Yilmaz N, Oğütcen-Toller M, Uzun E (2004) Relationship of condylar position to disc position and morphology. Eur J Radiol 51(3):269–273
Okur A, Ozkiris M, Kapusuz Z, Karaçavus S, Saydam L (2012) Characteristics of articular fossa and condyle in patients with temporomandibular joint complaint. Eur Rev Med Pharmacol Sci 16(15):2131–2135
Seo BY, An JS, Chang MS, Huh KH, Ahn SJ (2020) Changes in condylar dimensions in temporomandibular joints with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol 129(1):72–79
Mohamed HN, Ashmawy MS, Ekladious MEY, Farid MM (2023) Analysis of the relationship between condylar changes and anterior disc displacement with reduction: a preliminary study. Oral Radiol 39(1):154–163
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
Conceptualization: MSA, MMSF, AAA. Methodology: MSA, AAA. Data curation: MSA, AAA, AAA. Investigation: AAA. Validation: MSA, AAA. Formal analysis: MSA, AAT. Supervision: MMSF. Writing — original draft: AAA, AAT. Writing — review and editing: MSA, MMSF, AAA.
Corresponding author
Ethics declarations
Ethics approval
The methods followed in this study were according to the ethical standards of the responsible committee on human experiments (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consents were taken from the entire participants. Approval was obtained from research ethics committee of the Faculty of Dentistry, Cairo University, Egypt (No. 2152012).
Informed consent
Every patient was informed about the goal and methods of the study and then they provided written consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alhammadi, M.S., Almashraqi, A.A., Thawaba, A.A. et al. Dimensional and positional temporomandibular joint osseous characteristics in normodivergent facial patterns with and without temporomandibular disorders. Clin Oral Invest 27, 5011–5020 (2023). https://doi.org/10.1007/s00784-023-05120-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05120-0