Abstract
Introduction
Heat is generated and transferred to the dentine-pulp complex during various dental procedures, such as from friction during cavity preparations, exothermic reactions during the polymerisation of restorative materials and when polishing restorations. For in vitro studies, detrimental effects are possible when intra-pulpal temperature increases by more than 5.5°C (that is, the intra-pulpal temperature exceeds 42.4°C). This excessive heat transfer results in inflammation and necrosis of the pulp. Despite numerous studies stating the importance of heat transfer and control during dental procedures, there are limited studies that have quantified the significance. Past studies incorporated an experimental setup where a thermocouple is placed inside the pulp of an extracted human tooth and connected to an electronic digital thermometer.
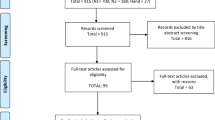
Methods
This review identified the opportunity for future research and develop both the understanding of various influencing factors on heat generation and the different sensor systems to measure the intrapulpal temperature.
Conclusion
Various steps of dental restorative procedures have the potential to generate considerable amounts of heat which can permanently damage the pulp, leading to pulp necrosis, discoloration of the tooth and eventually tooth loss. Thus, measures should be undertaken to limit pulp irritation and injury during procedures. This review highlighted the gap for future research and a need for an experimental setup which can simulate pulp blood flow, temperature, intraoral temperature and intraoral humidity to accurately simulate the intraoral conditions and record temperature changes during various dental procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human teeth consist of hard components (enamel, dentine, cementum), soft pulp tissue and sensory fibres [1]. Human teeth are regarded as a sensory tissue with the pulp, a soft connective tissue, containing nerve fibres and nerve endings extending into the dentinal tubules. These pulpal nerve terminals are crucial in sensing thermal stimuli [2,3,4]. Although heat transfer in human teeth is a common occurrence in both daily life and clinical dentistry, there is a lack of knowledge regarding the actual amount of heat transfer that takes place during dental procedures. This is important as trauma must be limited to a stressed pulp, where the accumulation of thermal, microbial, chemical and mechanical can compromise its vitality. Zach and Cohen [5] reported that an increase of 5.5°C in temperature can result in irreversible pulpitis and has since been the threshold cited by subsequent studies as the maximum temperature increase the dental pulp can endure. Although this value may have limited clinical relevance, it provides a value to which the results of other in vitro studies can be compared to. There are various stages during the dental treatment which generate heat, affecting the intrapulpal temperature: from cutting of the tooth structure by high-speed dental handpieces (HSDH), exothermic reactions during the polymerisation of light or self-cured restorative materials and during the polishing step. However, little is known about the effect of various factors which can increase the intrapulpal temperature. Moreover, since measuring the intrapulpal temperature in human subjects is both unethical and unfeasible, previous studies have adopted in vitro simulation models to conduct research on the change of intrapulpal temperature.
This review paper attempts to provide a comprehensive understanding on the heat generation during dental treatments affecting intrapulpal temperatures. To address this, firstly, the human tooth structure and heat transfer mechanism of enamel and dentine will be explained. Secondly, factors affecting the intrapulpal temperature during tooth preparation (cutting), crown fabrication, light curing and polishing will be discussed. Lastly, in vitro and in vivo methodologies used to study the intrapulpal temperature will be discussed, along with its opportunities and challenges. The objective of this review is to give an overview of the current research done on the heat generation during dental procedures and highlight the areas for future research to improve the understanding of the various factors that can affect the intrapulpal temperature.
Structure of human teeth
Enamel is the highly mineralised outermost layer, which is directly affected during restorative treatment. Below this is dentine, a mineralised connective tissue layer composed of an organic matrix of collagenous proteins [6]. Dentine accounts for most of the tooth structure by both weight and volume. It exhibits a complex hierarchical structure of organic and inorganic components, composed of approximately 70% mineral and 20% organic materials (mainly type I collagen) and 10% water by weight [6, 7]. In essence, dentine serves as the elastic foundation that supports the outermost hard and brittle enamel layer, while also acting as a protective medium for the innermost soft tissue, the pulp [1]. However, perhaps the most distinct feature of this layer’s microstructure is the network of long channels—the dentinal tubules. These extend outwards from the innermost pulp layer towards the exterior cementum or dentine-enamel junction (DEJ) [1, 6,7,8,9,10].
The dental pulp is a highly vascularised tissue encased in hard dentinal walls, containing a large amount of connective tissue, nerve fibres and sensory nerve endings [7]. Its innate ability to heal and repair itself has been previously studied, with the combination of the inflammatory response as well as both the proliferation and differentiation of numerous cell types combining to achieve the repair of the pulp-dentine tissue [11]. Regardless, the pulp is still vulnerable to impairment, particularly to heat exposure during tooth preparation and extensive restorative procedures. Pulp insults are mainly results of heat changes, desiccation, exposure to chemicals and bacterial infection [12]. Normal intrapulpal baseline temperature appears to range between 34 and 35°C [13], with increases in intrapulpal temperature exceeding 42 to 42.5°C sufficient to cause irreversible damage [13, 14]. This is of particular importance as an increase in intrapulpal temperature does not necessarily produce an increase in pulpal blood flow. Consequently, for the pulp which may already be dealing with the effect of thermal changes from tooth preparation, any previous inflammatory changes and limited perfusion may lead to the potential loss of pulpal vitality [15]. The effects of different harmful insults are cumulative, and where possible, dental clinicians must avoid materials and procedures which may contribute to the potential for iatrogenic damage to the pulp [16].
For in vitro studies, irreversible biological effects result when intra-pulpal temperature increases by more than 5.5°C (that is, the intra-pulpal temperature exceeds 42.4°C). It was found that 15% of the experimental teeth developed irreversible pulpitis or necrosis when this temperature was reached [5]. This is shared by another study which determined the temperature range for reversible damage to be between 42 and 42.5°C [17]. Overestimation of the pulp temperature changes in in vitro studies is probable, with the lack of blood and dentine fluid flow, and lack of periodontal tissues [18,19,20].
Mechanism of thermal insult to a human tooth
When heat is transferred to the pulp, it can cause various histopathological changes which may lead to irreversible injury. Unlike heat transfer to other materials, the thermal behaviour of teeth is a heat conduction process, combined with its physiological processes, such as dentinal fluid flow and pulpal blood flow [7]. The mechanism of injury includes protoplasm coagulation, expansion of the liquid in the dentinal tubules, increased outwards flow from the tubules, vascular injuries and tissue necrosis [12, 13, 16, 21]. Moreover, because of the variance in thermophysical properties and microstructure between the layers in human teeth, heat transfer may also result in thermal stresses that lead to cracking within the different layers [7, 22].
It is thought that an intrapulpal temperature rise above 43°C activates nerve fibres, leading to a reactive increase of blood circulation which assists in the dissipation of any heat advancing towards the dental pulp [7]. Additionally, the surrounding periodontal tissues could also play a significant role in promoting heat convection, thus limiting the intrapulpal temperature rise [14]. Although the flow of dentine fluid can enhance the heat transfer within the pulp upon heating, it is the pulp microcirculation of blood that plays an important role in the thermoregulation of pulpal soft tissue. In essence, the pulp blood flow rate is practically constant within the range of 33 to 42°C but increases significantly when the temperature rises above 42°C. Perfused blood works as a heat sink under heating and as a source of heat when subjected to cooling. Yet, the overall influence of pulpal blood flow on heat transfer is thought to be minimal due to its relatively low blood volume [7].
In addition, several other biological factors impact on whether the pulp tissue undergoes irreversible effects. This includes the amount of water content in the pulp, the changes in pulp blood and dentinal fluid flows, previous injury to the pulp, the health of the tissues, remaining dentine thickness and insulating quality, duration of insult and the surface area of exposed dentinal tubules [23,24,25,26,27,28]. Alternative consequences, such as necrosis and alveolar bone loss, and even ankylosis can also occur when intrapulpal temperatures increase by 3 to 10°C during tooth preparation [29, 30]. Higher and longer lasting temperature peaks, and specifically those exceeding the 5.5 °C increase threshold, may lead to pulpal necrosis, and an excessive temperature increase of 3–10 °C can lead to periodontal malformations (e.g. alveolar bone necrosis, bone loss and ankylosis) [29, 30].
Tooth heat transfer
The relatively low values for thermal conductivity (TC) and diffusivity of enamel and dentine help protect the deeper tissues from thermal insults [31]. Additionally, the characteristic arrangements of its inner structures have a significant influence on heat excursion in teeth [7]. Nevertheless, greater attention is given to dentine since it is often the layer in direct contact with provisional materials and the layer likely to be involved in the heat transfer that takes place from the surface of the tooth preparation to the pulp chamber.
Even though both enamel and dentine are hard components with a high percentage of mineral content, their thermophysical properties are different. TC indicates the ability of a material to conduct heat and the TD is the measure of the speed with which a temperature change will proceed through an object [32]. The TD and TC of enamel are approximately 2.5 and 1.6 times larger than dentine, respectively [33]. Dental pulp is involved in the maintenance of tooth vitality and is vulnerable to heat changes without the protection of the enamel and dentine layers. The TC and TD of enamel and dentine are relatively low compared to those of the pulp; therefore, these two layers are effectively thermal insulators and protect the pulp from deleterious thermal irritation [7].
The thermophysical properties of the tooth is a factor in its thermal behaviour and depends on the microstructures of each tooth layer (Fig. 1). However, because the human tooth is a living tissue, the heat conduction process occurs in conjunction with physiological processes, including the fluid motion in the DTs and blood circulation in the pulp chamber. Dentinal fluid flow could improve the heat transfer within the pulp during temperature changes. The pulpal blood flow also influences the thermoregulation of pulpal soft tissue. The increase of pulpal blood flow rate during extra heating from hot foods or rotary dental procedures (above 42°C) works as a heat sink, while during cooling, e.g. from the water jet spray of a handpiece, the blood flow would maintain the temperature as a heating source [7].
Residual dentine
Dentine acts as a thermal barrier against harmful stimuli. The flow of heat through dentine is proportional to the TC of dentine and inversely proportional to the thickness of the residual dentine [34]. The key material properties for heat transfer in teeth; the TC and TD values are both low for dentine [21]. Residual dentine is a critical factor in reducing heat transfer to the pulp with its thickness seeming to be the most important factor in determining pulpal protection. A thicker residual dentin layer results in a greater insulating effect, affecting the quantum of heat transfer to the pulp chamber during dental procedures [7, 12, 13, 21, 34, 35]. Thus, factors such as the type of tooth preparation (full veneer preparation on molars, three quarter preparation on molars or premolars) should be carefully considered this ultimately determines the amount of residual dentine and therefore the level of potential risk to the pulp arising from intrapulpal temperature rise [21, 34]. However, in the clinical situation, the thickness of prepared dentine is difficult to assess and therefore cannot be used to exclude thermal damages to the pulp [21, 36].
Dentinal tubules
Factors such as the presence of dentinal tubules strongly impact the porosity, density and TC of dentine [7]. Dentinal tubules are a network of channels radiating outwards from the pulp cavity to the DEJ [1, 6, 7]. Thermal conductivity of dentine will vary with dentinal tubule density, orientation and structure (normal, transparent and reparative dentine, with reparative dentine being the formation of a tissue barrier by odontoblast-like cells following pulpal insults) [36]. For instance, the TC of dentine decreases with increasing volume fraction of dentine tubules [7]. Likewise, specific heat of dentine is said to rely on the orientation of dentine tubules [7]. These characteristics in dentine promote a better transfer of heat towards the pulp where heat dissipating mechanisms can be activated [7, 14]. Yet, these physical properties of teeth differ extensively even for a single tooth but also between different teeth (incisor, canine, molar) including age, gender, ethnicity and different donors [37,38,39].
Previous work has demonstrated that there is a notable increase in the number of dentinal tubules in regions near the pulp chamber, providing a greater overall surface area available for diffusion compared to a much smaller presence of dentinal tubules in regions closer to the DEJ [8]. This spatial variation in density of the dentinal tubules range from about 10,000 lumens/mm2 at the DEJ to about 60,000 lumens/mm2 near the pulp [6]. Therefore, it could be concluded that the microstructure of human dentine is adapting to not only withstand thermal alterations but also to dissipate heat towards the pulp chamber. Accordingly, it is postulated that the thickness of the residual dentine layer could determine the density of dentinal tubules, where small amounts of residual dentine thickness would be more prone to intrapulpal temperature increase due to a greater presence of dentinal tubules [8].
Dentine thermal conductivity
By combining the residual dentine thickness with the coefficient of thermal conductivity of dentine, it is possible to establish the rate of heat flow from a thermal exposure at the surface of the cut dentine layer and establish the potential risk to the pulp tissue. This relationship is represented by a modified thermodynamic equation [35]:
H is heat flow through dentine per unit time, K is the thermal conductivity of dentine, A is the surface area exposed to the heat stimulus, D is the thickness of the residual dentine layer and t2 − t1 is the temperature difference.
This equation demonstrates that heat flow through dentine is directly proportional to the TC and inversely proportional to the residual dentine thickness [34, 35].
Heat generated during tooth preparation
Tooth preparation
The restorative process of preparing a tooth to receive a fixed prosthetic restoration requires both clinical and technical considerations [21] as shown in Fig. 2. A critical area of concern for the clinician during this, often lengthy and involved procedure, is the minimising of external factors that lead to an increase in heat production and are potentially harmful to the vitality of the tooth [13]. Two specific heat-generating variables include the friction between the HSDH and tooth and the exothermic setting reaction of self-polymerising restorative materials used for the temporalisation of the tooth preparation or the heat generated from the light curing of dental resins [7, 13]. Studies have shown a direct relationship between the tooth preparation design and intrapulpal temperature rise, especially the thickness of the residual dentine layer [13, 21, 34,35,36].
High-speed handpiece in dentistry
In dentistry, the HSDH is a commonly used equipment in any clinical setting. It is used for fast and efficient removal of tooth structure in restorations [40]. A good high-speed handpiece should be of an ergonomic size and weight, have a suitable head size, have adequate power and speed, have adequate illumination and have sufficient cooling features. Cooling features are important because tooth cutting produces friction and heat between the bur and tooth surface. Excessive heat can transfer to the pulp, resulting in inflammation and necrosis if not dissipated efficiently, as well as structural changes in the enamel and dentine [26, 41].
Air turbine versus electrical high-speed handpieces
There are two main types of HSDHs—an electric micromotor which utilises an electric motor to generate the required rotational force, and an air turbine which utilises compressed air [42]. The main advantage of electric micromotor–driven handpieces over air turbine handpieces is the greater cutting efficiency, with a smoother and even cutting rate caused by the constant torque maintenance under high loads and lack of ‘stalling’ compared to air motor–driven handpieces [43,44,45]. While air turbine far outruns electric motor run HDSH regarding speed, reaching speeds as high as 420,000 rpm, they lack the torque stability of electric HSDHs. Low torque means that there is less rotational force, and with the rotational speed decreasing it may stall at high loads, whereas the consistently high torque will maintain a constant rotational speed that does not decrease with high loads, therefore exhibiting a greater cutting efficiency [42, 46]. The greater cutting efficiency of electric HSDHs applies to a variety of dental materials, including glass ceramic, silver amalgam and high noble alloy [43]. The torque of the handpiece is expressed by the power specification of the handpiece [46].
One study found electric handpieces resulted in greater decrease in intra-pulpal temperature in comparison to air turbine handpieces, due to the improved cutting efficiency and friction production [42]. However, with no other studies validating this result, the impact of handpiece type on intrapulpal temperatures changes cannot be concluded. In addition, evidence of the effect of input air pressure and torque on temperature increase is conflicting between studies. Ozturk et al. [47] found temperature increase with increasing air pressure, but Firoozmand et al. [24] found no difference in pulpal temperature between high torque and low torque HSDH. Both speed and power of the HSDH is related to the generated energy, so increased HSDH speed results in increased intra-pulpal temperature [48]. However, within the handpiece body itself, more heat is generated with electric HSDHs. This can result in soft tissue injuries when the handpiece is running at maximum speed without an effective cooling mechanism [49, 50].
Coolant ports to reduce the thermal shock to the tooth
Most modern HSDHs incorporate air or air-water coolant ports. These are designed to form a halo around the bur and spray high-velocity water and/or air at the tooth-bur interface. This improves visibility, cutting, polishing and cooling efficiency, as well as decreases the frictional heat and risk of pulp injury [23, 30, 40, 47, 51, 52]. Schuchard [53] conducted a photographic study looking at the action of the coolant water droplets while the bur is rotating at working speed. He found that with the water volume and pressure used in clinical setting, the coolant does not actually reach the cutting part of the bur. Instead, the coolant has a cooling effect on the entire tooth, rather than just the area of contact [53].
Dental handpieces can differ on the number and location of their coolant ports, with 1-, 3- and 4-port varieties available for air turbine, and 1- and 4-port varieties for electric. Siegel and von Fraunhofer [54] reported that the introduction of the 3- and 4-port handpieces was to allow sufficient cooling of the tooth if one or more ports become blocked. Theoretically, it would be hypothesised that the greater number of coolant ports would result in a greater cooling efficiency as the coolant would be greater distributed over the cutting surfaces. In general, manufacturers have claimed that more ports enhance cooling efficiency; however, the results from recent studies are inconclusive. Chua et al. [23] demonstrated that there was no statistical significance between the intra-pulpal temperatures following the use of high-speed air turbine handpieces with different coolant port designs (1-, 3- and 4-ports), whereas a later study, Lau et al. [55], found a statistically significant difference found between the cooling efficiency with 1- and 4-port coolant design on electric micromotor HSDHs.
The coolant port design also influences the cutting efficiency—HSDHs with a multiport coolant design exhibit greater cutting efficiency compared to those with a single coolant port, even if the 1-port handpiece has a higher coolant flow rate [54, 56]. Similarly, Lloyd et al. [57] observed that cutting with water results in cutting rates three times that of dry cutting, with Siegel and von Fraunhofer finding that 1-port HSDH had significantly lower cutting rates than 3- or 4-spray ports when making groove cuts (with intact edges) [54, 57]. However, this difference was only observed when performing groove cuts (surrounded by tooth structure), and not when performing edge cuts. Groove cuts differ as they produce greater increases in temperature, due to the concentration of generated heat at the bur interface and decreased accessibility of water spray [58]. Additionally, the position of spray ports affects water supply to cutting interface and therefore cutting rate. The authors Siegel and von Fraunhofer [54] observed in previous studies that cutting rates varied with different spray port numbers and positioning, especially if there was a blocked port. Yang and Sun [56] conducted a similar experiment on ceramic blocks, utilising both edge and groove cutting. However, they found that only the output coolant flow rate, and not the number of spray ports, affected cutting efficiency.
Type of bur used
There are a variety of burs used by the dentists with HSDHs. Studies have concluded that the type of bur used, whether it be made of diamond or carbide, and/or its shape, size and grit size, depended on clinician preference and is highly influenced by equipment used during dental school [59]. Diamond burs are the most popular, followed by tungsten carbide burs [59].
Current studies on the effect of bur type on the heat generation and cutting efficiency are inconclusive, with studies reporting contradicting findings on the differences between diamond and carbide burs. Most agree that carbide burs generate less heat and pressure [60] potentially due to the different cutting mechanisms—diamond burs tend to clog with a grinding action used to remove tooth structure [61] whereas carbide burs, with their fluted design, use a cleaving action instead. Diamond burs have been found to showcase poorer cutting efficiency when compared to carbide burs with a thicker smear layer and greater frictional heat produced [42, 48, 62]. This can be attributed to the action of a diamond bur, where a large amount of energy is applied on the small cutting surfaces of each diamond grit [58]. Watson et al. [48] found that diamond burs produced more temperature increases, as there is a greater area of contact and more friction produced. Nevertheless, several studies have found the opposite with lower heat generation with diamond burs [61], and greater increases in temperatures with deeper cavity preparations using tungsten carbide burs [62].
Numerous other factors such as the bur size, shape, coarseness and amount of surface wear can influence the amount of heat generated during mechanical tooth preparation. Diamond burs are available in different grit sizes, which produce different finishes. Coarser grit burs produce less of a smooth surface, and more friction and thus heat [63, 64]. In addition, as burs wear out and lose their grit, there is reduced cutting efficiency [65, 66]. Similarly, when the diamond bur clogs with debris or stall, their generated energy creates a significant spike in temperature [58]. In addition, there appears to be differences in the burs produced within a manufacturer and between different manufacturers [61].
Overall, however, studies found that the increase in intra-pulpal temperature was not clinically significant. In Watson et al.’s study [48], all tests with different burs resulted in a drop in intra-pulpal temperature. Ercoli et al. [51] and Lau et al. [55] also found that despite an increase in temperature for some burs, all were still below the critical value to cause pulpal damage.
Cutting technique
The cutting technique adopted by dentists can vary by either continuously cutting with no pause or intermittent cutting with periods of pauses. A study on cutting techniques showed that intermittent cutting produces greater cutting effectiveness [67]. In intermittent cutting, heat dissipation can occur during the periods of rest where the bur is not in contact, resulting in a lower overall temperature increase [64, 68, 69]. Similarly, an experimental study also showed that continuous cutting with high loads resulted in greater temperature increases [68].
Other variables of cutting technique, such as rotational speed, operator pressure, depth of the cavity preparation, duration and even the differences in the cutting medium (extracted teeth versus glass slabs), will also impact the heat generated and the results of previous in vitro studies.
Effect of water coolant on intra-pulpal temperature
Many studies found that air coolant is insufficient, and water stream or air-water spray are more appropriate forms of cooling when drilling with HSDHs. This is supported by both histological studies [70, 71] and studies measuring intra-pulpal temperature [47, 48, 71,72,73,74,75,76].
The two main variables that influence the heat absorption ability of the water coolant are its flow rate and the temperature [27]. Currently, utilisation of flow rates between 30 and 50mL/min is the standard cooling conditions [27, 47, 51, 52, 68, 77, 78], with the International Organization for Standardization recommending the upper level of the threshold at 50mL/min [79]. These coolant flow rates are necessary to decrease thermal injury with a cooling effect at both the cutting interface and the handpiece head, with maintenance of adequate operator visibility [25, 80]. If the coolant flow rate is high enough, theoretically, the pulp tissues will not exceed the temperature of the water coolant used [41]. When sufficient coolant was used, the closer the bur is to the pulp, the further the temperature dropped [72]. Leung et al. [81] also found that thermal resistivity for air-water spray was lower than for water stream cooling at the same flow rate. The maximum output flow rate of the HSDH varies with the number of spray ports, if the water pressure is kept the same [80]. The study found that HSDH with 1 spray port had the highest flow rate, followed by 2 ports, and then 3 spray ports.
Temperature of the coolant water also affects intra-pulpal temp in cooling. Lower water temperatures have both a greater cooling efficiency and a greater heat absorption capacity [41]. However, the clinical usefulness is limited due to the increased risk of pulp damage with the reduced pulp blood flow and decreased waste removal ability. This can occur if pulp temperature drops below 21°C [82]. In addition, both the operator and patient may be uncomfortable when cooler water is used, especially with prolonged appointments and patients who suffer from cold sensitivity. Several studies have recommended the use of room temperature water at between 25 and 50 mL/min coolant flow rates to effectively prevent pulp injury [47, 52]. Farah et al. [41] investigated the impact of three different water coolant temperatures, 10°C, 23°C and 35°C, at the coolant flow rate of 50 mL/min. This study concluded that water coolant was essential to prevent injury of the pulp and soft tissues, and that a coolant temperature of 35°C in electric handpieces offers only minimal protection as temperature increases were observed. Past studies have shown that electric handpieces increase the water coolant temperature, with heat gained when the water travels through the handpiece [41], which results in the possibility of soft tissue damage [50]. Friction can be generated by the motor bearings, which can create heat that results in warming of the coolant water [68].
Intrapulpal temperature increase by dental provisional crowns
After tooth preparation, the patient receives provisional crown(s) while the final dental restoration is made in the dental laboratory. The requirement for provisional crowns has been mainly derived from the methodological process that relies on the indirect fabrication of the definitive restoration in the dental laboratory. Provisional crowns must, with the exception to the type of material from which they are fabricated, resemble the planned final restoration in all regards to satisfy areas of critical concern [83]. These restorations restore function to the prepared tooth with only slight differences to the definitive restoration they precede [84].
The overarching aims of provisional crowns can be summarised as biologic, diagnostic, aesthetic and mechanical [85]. Biologically, provisional crowns must provide adequate contour that stabilises and promotes gingival health, and restore functional intercuspal and proximal contacts that prevent migration of the prepared tooth and movement of the adjacent teeth, as well as provide immediate protection to the pulpal tissues [86, 87]. The latter is of particular interest to this review as an unfavourable combination of the type of material and the method of fabrication could be detrimental to the pulp of a vital tooth. Therefore, clinicians must take extreme caution during the provisional restorative phase to ensure the health of the underlying tissues.
Fabrication methods and types of dental provisional crowns
There are two main methods for fabricating provisional crowns: the direct and the indirect method. The direct method places acrylic resin material onto the prepared tooth, with the risk of thermal injury at temperature increases of 5.6°C in the pulp [18, 36]. Most chair-side materials in use by clinicians for provisional restorations lead to a rise in temperature during polymerisation [88], and may also cause irreversible damage to the gingival and pulpal tissue [89]. Furthermore, the presence of free monomer in direct contact with open dentinal tubules can be harmful and cause pulp inflammation if it leaches towards the pulp tissue [90, 91]. For the indirect method, materials are able to be cured in a hydro flask which shields the freshly prepared tooth from the heat released from the polymerising resin [83].
Polymers used in provisional restorative materials are classified either by their chemistry or by method of curing. The chemistry group of polymers include acrylics, composite resin and polycarbonate [92]. Methods of curing include chemical, heat, light or dual-activated. Predominately available commercial options for provisional restorations are either composite resin (bis-A-glycidyl methacrylate, bis-acryl, urethane dimethacrylate) or methacrylate resin (methyl methacrylate, ethyl methacrylate, vinyl methcrylate, butylmethacrylate)–based materials. The choice of material should be based on the clinical needs and longevity of the provisional restoration.
Exothermic properties of provisional materials
Provisional crown materials available today have in common that they cure by radical polymerisation resulting in either a non (mono-methacrylates) or highly cross-linked polymer network (di- or multifunctional methacrylates) [36]. It is the exothermic character of radical curing that leads to a significant amount of heat being generated during the course of polymerisation [36]. The reaction of these polymer-based provisional materials is through additional polymerisation, where carbon-carbon double bonds are converted to new carbon single bonds. The exothermic heat released during the polymerisation process is a direct result from the difference in energy between the two bonds [21, 34]. Thus, there is variety in the amount of heat generated for different materials. For example, in a previous study examining the temperature profiles of a direct (Luxatemp) and preformed (Hi-tempo) provisional crown materials, both of which is placed directly on the tooth preparation, a higher temperature increase was noted with the preformed crown system [93].
Heat generated during the placement of the final dental restoration
The placement of the final dental restoration often requires adjustments, with the generated frictional heat transferred to the pulp chamber [44]. This heat transfer will be dependent on the thermal conductivity and diffusivity of the material/materials being used in the construction of the final restoration and the material of the bonding system.
Generally, thermal conductivities increase in the following order: polymers < ceramics < metals [94]. The higher value of thermal conductivity means that the material has greater ability to transmit thermal energy. However, if the temperature gradient changes with time, thermal diffusivity is used to determine the amount of heat transferred. Therefore, the thermal diffusivity of a dental restorative material might be more important than its thermal conductivity. This property also depends on the material’s density and heat capacity. Thermal diffusivity is not in proportion to the thermal conductivity, which means that a material might have a low thermal diffusivity and relatively high thermal conductivity.
Gold is sometimes utilised as an alloy material for dental restorations which has about 500 times the thermal conductivity (297 Wm−1K−1) and 600 times the thermal diffusivity (1.18 cm2s−1) than that of dentine. Hence, compared to dentine, gold restorations provide very little protection to the pulp against the thermal stimulation. However, the thermal conductivity of zirconia (2.5–2.8 Wm−1K−1) is extremely low compared to metallic materials and alumina (30 Wm−1K−1) [94] with lithium disilicates having a thermal conductivity of 5.2 Wm−1K−1 [95].
Intraoral polishing of fixed dental restoration
Temperature rise is a common occurrence and could easily exceed the 5.5°C threshold value during the intraoral polishing procedure [96]. Zirconia, for example, has much higher hardness, elastic modulus and fracture toughness than other all-ceramic restorative materials [97]. Therefore, it requires much higher frictional forces (e.g. with higher speed and/or harder polishers) to create a smooth surface if it is not glazed, which is known to generate more heat [97, 98]. İşeri et al. [99] studied the temperature changes during clinical procedures, focusing on the periodical and continual grinding of disc-shaped zirconia specimens (15mm diameter × 1mm) with micromotor at 22,000 rpm and high-speed handpiece at 320,000 rpm. The study showed that dry grinding and adjusting zirconia produced a temperature rise of 63.4°C, by far exceeding the critical temperature which is known to cause pulp damage.
Chavali et al. [98] investigated the influence of two polishing systems and three speeds on the heat production of zirconia. In order to compare the heat generation via intraoral polishing, three different types of polishing agents were used to polish zirconia specimens into 4-mm-thick sections at either 5000, 15,000 or 40,000 rpm with slow-speed dental handpieces [98]. The results showed that no group generated surface temperature over 42°C, which is just under the critical temperature for pulp damage reported by Zach and Cohen [5].
Heat generation during direct restoration with light curing
The heat generated during photopolymerisation using visible light-curing units has the potential of causing damage to pulp tissue. The temperature elevation occurs due to increased exposure time to light during irradiation. Studies have identified photopolymerisation as a big risk to pulp health demonstrating a temperature rise between 4.3 and 7.5°C during photopolymerisation of composite discs [100]. Another study recorded intrapulpal temperature rises ranging from 1.5°C to more than 4°C during light-curing of composite resin restoration of extracted teeth. Yet, clinical experiments have demonstrated that the pulp appears to recover from transient heating from light-curing units [14]. Some consideration must be given to the combination of the temporary material and the type of light-curing unit used as its output may influence the final temperature rise. The heat emission during polymerisation may induce a temperature rise that may be of biological concern. With regard to tooth preparation in prosthodontic dentistry, the probability of damage to the pulp is real when the temperature increase due to polymerisation is greater than the physiologic heat dissipation mechanisms of the dental periodontal system [21].
Influence of light intensity on temperature raise of BCRs
As discussed previously, the increase in light intensity is associated with increasing concern of heat generation within the BCRs and subsequent pulpal injury. Balestrino et al. [101] found a difference in heat generation between various types of light curing units. They concluded that the LEDs produced higher temperature rises than the QTH, and the LED with lower irradiance causing higher temperature rises than the LED with higher irradiance [101]. However, the heat dissipation design of a light-curing unit should also be taken into account. Armellin et al. [102] provided an alternative perspective on the heat generation of BCRs, by stating that the temperature increase during resin curing is a function of the rate of polymerisation, which is not only associated with the energy from light curing units, but also due to the exothermic polymerisation reaction and time of exposure.
Par et al. [103] found that temperature rise during curing ranged from 4.4 to 9.3°C and was significantly reduced by curing with the lower intensity blue curing unit. This study also suggested that the correlating temperature rise of radiant energy, in combination of material × thickness × curing unit, revealed a highly significant linear relationship [103]. However, there is no direct evidence that support the relationship between the light intensity on heat generation of BCRs and the subsequent pulpal injury. Uhl et al. [104] argued that no considerable difference in the temperature increase within the pulp chamber model was found for the different light curing units and composites.
Methods to measure the change of pulpal temperature during dental procedures
The most used method for measuring heat generation is by measuring real time temperature change via thermocouples, which is a reliable and relatively simple method to measure temperature change within dental materials or measuring heat transfer across the tooth structure [5, 68, 74, 75, 105,106,107,108,109,110,111,112,113,114,115]. There have been variations in the methods of measuring heat generation which could potentially lead to differences in results. For example, the type of thermocouple wires used were different. Some studies used J-type thermocouples [101, 102] while others used K [104] or T-type [103]. However, there has been no evidence that suggest the types of thermocouples can have significant influence on the measurement of real-time temperature change in dental settings or dental materials.
Measurements of heat generation and related temperature change can also be affected by the position of the thermocouples placed, as a change in location of the probe, which can result in variation of measurements and inconsistent results [93]. Additionally, a silicone heat-transfer compound injected into the pulp chamber is used to help transfer the heat from the walls of the pulp chamber to the thermocouple [23, 93]. Measurements of heat transfer can be affected by the placement of the thermocouple, which needs to be in the same position at each measurement to minimise any variations that can be caused by any variant location of the probe [88]. Radiovisiography can be used to determine proper positioning of the thermocouple probe, as well as the residual dentine thickness [93]. To minimise this variation, radiovisiography can be adapted to aid in proper positioning of the thermocouple probe [102, 116].
Often specimens are prepared either in disc shapes or by using actual tooth preparations. As shown in Table 1, previous studies appear to largely employ molars for their studies with few using pre-molars and only two studies used dentine discs. In general, when using tooth specimens, the design had been shaped to represent real case applications by using tooth preparations for either crown or cavity restorations. From the literature, there also seems to be a systematic preference to using thermocouples to measure changes in temperature. Additionally, most studies have adopted some form of metallic material to fill the cavity of the pulp chamber to facilitate heat transfer to the thermocouple. On the other hand, it is surprising that most studies had a small sample size (n=5) and although two studies used water baths to simulate intraoral conditions, with only one study having attempted a model to simulate the complex intrapulpal fluid flow. Many studies listed in Tables 1, 2, 3, 4 had one thermocouple located in the pulp chamber. Thus, they were interested in only measuring the intrapulpal temperature change, rather than the heat transfer from outside the enamel down to the pulp (during dental procedures/restorative materials). The difference in methods adapted in various studies makes it difficult to compare their results. Furthermore, one common limitation of these in vitro studies is the lack of blood circulation seen in vital pulp and associated heat dissipation. Overestimation of the pulp temperature changes in in vitro studies is probable, with the lack of blood and dentine fluid flow, and lack of periodontal tissues [18,19,20]. This could limit the representativeness of the results to vital human dentition.
Experimental setup to simulate intraoral environment
Although thermogenesis during various dental procedures is extremely common, the amount of heat generation needs to be measured for providing clinical implications for better instruction and instrument application [36]. Heat transfer in teeth commonly depends on the geometry of the tooth itself, material properties and biological function. The biological function would be the biggest challenge for the experimental setup. In vivo experiments reflect the active processes within a tooth, whereas the experimental measurement of in vivo temperature changes within tooth pulp is impractical. Obviously, the in vitro test would be the only choice and the way how the simulation system is built up would influence the accurateness and reliability of the results. For mimicking the natural intraoral environment, three main factors should be considered: temperature, intra-pulpal blood fluid and humidity. Also, there are several integrated simulation systems of the intraoral environment used by previous studies, which could be referred to for setting up a more realistic and ideal experiment. Various methodologies applied across previous studies that stimulated the above three factors are summarised in Table 4.
Effect of pulpal blood flow and microcirculation model
Pulpal blood flow (PBF) which varies with external stimuli helps maintain pulpal temperature by providing circulation and absorbing or providing heat [117]. Kodonas et al. [118] reconstructed pulpal microcirculation by running 37°C water through extracted human teeth and found significantly lower temperature increase under the microcirculation model. However, PBF varies with external stimuli. It decreases when the pulp is cool and increases significantly when pulpal temperature increases above 42°C and clinically used vasoconstrictors slow or stop PBF [119].
Most studies evaluating the heat generation via dental procedures, such as Chavali et al.’s study [98], were designed and completed at room temperature (24.0 ± 0.3°C) and with ambient humidity [34, 99]. However, the surface temperatures of the dentition and soft tissues have been found between 30 to 35°C and 32 to 37°C, respectively [120]. Amsler et al. [121] showed that the temperature range of the oral cavity was 26 to 29°C.
In Dias et al.’s study [84], they investigated the real-time pulp temperature change during temporary crown fabrication, comparing the heat generation during two different temporary crown systems and at different tooth sites. In Chua et al. and Dias et al.’s studies [23, 93], the authors simulated the pulp temperature by adding 37°C water in the container where the teeth specimens were fixed during the experiment (Fig. 3). These two studies highlighted the importance of conducting the experiment with 37°C water to simulate the baseline pulp temperature as the experiments carried out at room temperature had a significant impact on the temperature profile. For example, when pulp temperature was measured with and without 37°C water during a self-polymerising temporary crown fabrication, there was almost 20°C difference in pulp temperature between the two techniques (Fig. 4). When compared to the results from a previous study by Kim and Watts [34] using the same crown material conducted at room temperature, the authors found that while the pulp temperature stabilised at 37°C, the temperature recorded in the pulp chamber was 69 times lower [34, 93].
Different temperature profile graphs found from Dias et al.’s study [93] with (37°C water bath; WT) and without (room temperature; RT) pulp temperature simulation.
In Chavali et al.’s study [98], the polishing was also assessed without pulp temperature simulation. They discussed that dry polishing had the possibility to affect the rate of evaporation and thereby cooling rate. Their results of the temperature increased to 42°C from the intraoral polishing may have come from the fact that the experiment was conducted at room temperature and may have increased when it was done under pulp temperature simulation conditions [98]. In order to determine the reference values of the two intraoral factors, Park et al. [122] assessed the accuracy of two intraoral scanners utilising a box-shaped intraoral environment simulator to mimic the temperature and humidity of the mouth (Fig. 2b). Then, in Farah’s studies [41, 123], an incubator at 37°C ± 1°C was used as the simulation chamber of the intraoral temperature to evaluate the effect of cooling water temperature on the temperature changes in the pulp chamber (Fig. 2c, d). These two studies successfully simulated the intraoral temperature, but pulp flow and intraoral humidity were not simulated in this study.
Intra-pulpal blood flow and intraoral humidity
Surveys such as that conducted by Goodis et al. [124] and Mülle and Raab [125] showed that the pulp blood flow probably mediated the effective homeostatic mechanism within human teeth, while many in vitro heat transfer studies of human teeth were carried out with cleaned and empty pulp chambers. Linsuwanont et al. [126] reported that, under temperature fluctuations, any fluid movement either away from or towards the pulp would inevitably result in the redistribution of the pulp chamber temperature. Lin et al. [7] also briefly stated that the TC and heat capacity of teeth of empty pulp chambers were significantly different from filled chamber with pulp soft tissue.
In Kodonas et al.’s research [118], it found that the heat transfer experiments conducted without pulpal simulation would result in temperature increase of a greater magnitude than those with pulpal simulation. In order to simulate the vital dental pulp, Hannig and Bott [14] filled the pulp chamber with warm water to mimic heat transfer through soft tissue in the pulp chamber. Attrill et al. [127] filled the dead space of pulp chamber with a ‘pulp phantom’ which provided a thermal conduction environment similar to the vital dental pulp and Chua et al. [23] and Farah [41] utilised a high-density polysynthetic silver thermal compound inside the pulp cavity to improve conductivity. Nevertheless, Hannig and Bott [14] reported that the influence of pulpal blood flow on the thermal behaviour of the dentine-pulp complex cannot be simulated by stationary water inside the testing container. Chua et al. [23] also suggested that a better pulpal simulation experimental setup would help to find the more exact results of the temperature change. However, this will be challenging to accurately replicate due to its dynamic nature and changes in flow following different stimulations, such as temperature increases causing an increase in blood circulation [14]. Previous studies have many attempts to simulate this flow. An earlier research, Daronch et al. [13], noticed the deficiency of empty pulp chambers, which limited the direct application of the measurement data of in vivo situations, and employed an infusion pump connected to the tooth roots through a small diameter tube. This device delivered water at a speed of 0.0125 ml/min to simulate the pulpal blood flow. At the same time, the tooth was immersed into a water bath up to the cement-enamel junction. Then, Farah [123] used a curved needle connected to a peristaltic pump with a controlled fluid flow rate to simulate the pulp blood flow. This study also concluded that simulated pulpal blood flow resulted in a lower increase in the pulp chamber temperature, compared to when pulpal blood flow was simulated [123] (Fig. 5).
Temperature recorded in the pulp chamber during fabrication of temporary crowns; note the effect of different conditions of water flow rate [123]
The relative humidity of the oral cavity has been found to vary in the range 78 to 94% during operative dental procedures [120, 121, 128]. Breathing through either nose or mouth showed no significant effect on the relative humidity [121]; however, the relative humidity would have decreased once the use of the rubber dam was completed [120]. Bicalho et al. [129] constructed a chamber to mimic the oral environment and evaluated the effect of the temperature and humidity. They controlled the humidity by a water spray system which was activated automatically to maintain a pre-set humidity value of either 50 or 90% at 22 or 37 °C. According to their study, the temperature and humidity had a significant influence on the mechanical properties of restored teeth with composite resins [129]. In another study, the flexural modulus and flexural strength properties of composite were not negatively influenced by the simulated intraoral conditions of 35°C at 90% relative humidity [130].
Conclusion
Various steps of dental restorative procedures have the potential to generate considerable amounts of heat which can permanently damage the pulp, leading to pulp necrosis, discoloration of the tooth and eventually tooth loss. Thus, measures should be undertaken to limit pulp irritation and injury during procedures. This is especially true as damage to the pulp is accumulative and past insults affect the restorability of the tooth. Despite the importance of this topic, there are limited studies available which investigate the influencing factors and dental procedures. Experimental setups of simulating intraoral environment have been employed by most previous studies using an incubator at 37°C to mimic the intraoral temperature [23, 93, 123]. However, there is limited research which simulated the pulp blood flow using the peristaltic tubing pump and temperature [123]. The use of intraoral humidity chamber was employed by one study to simulate the relative humidity around natural teeth, which is an important variable [122]. This highlights the gap for future research and a need for an experimental setup which can simulate pulp blood flow, temperature, intraoral temperature and intraoral humidity to accurately simulate the intraoral conditions and record temperature changes during various dental procedures.
Data availability
Data will be available upon request.
References
Nazari A, Bajaj D, Zhang D, Romberg E, Arola D (2009) Aging and the reduction in fracture toughness of human dentin. Journal of the mechanical behavior of biomedical materials 2:550–559. https://doi.org/10.1016/j.jmbbm.2009.01.008
Frank RM (1999) Ultrastructure of human dentine 40 years ago-progress and perspectives. Archives of Oral Biology 44:979–984. https://doi.org/10.1016/s0003-9969(99)00109-0
Graf W, Bjorlin G (1951) Diameters of nerve fibers in human tooth pulps. The Journal of the American Dental Association 43:186–193. https://doi.org/10.14219/jada.archive.1951.0180
Hildebrand C, Fried K, Tuisku F, Johansson CS (1995) Teeth and tooth nerves. Progress in neurobiology 45:165–222. https://doi.org/10.1016/0301-0082(94)00045-j
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530. https://doi.org/10.1016/0030-4220(65)90015-0
Ryou H, Romberg E, Pashley DH, Tay FR, Arola D (2015) Importance of age on the dynamic mechanical behavior of intertubular and peritubular dentin. Journal of the mechanical behavior of biomedical materials 42:229–242. https://doi.org/10.1016/j.jmbbm.2014.11.021
Lin M, Xu F, Lu TJ, Bai BF (2010) A review of heat transfer in human tooth--experimental characterization and mathematical modeling. Dental Materials 26:501–513. https://doi.org/10.1016/j.dental.2010.02.009
Carda C, Peydró A (2006) Ultrastructural patterns of human dentinal tubules, odontoblasts processes and nerve fibres. Tissue and Cell 38:141–150. https://doi.org/10.1016/j.tice.2006.01.002
Pashley DH (1996) Dynamics of the pulpo-dentin complex. Critical Reviews in Oral Biology & Medicine 7:104–133. https://doi.org/10.1177/10454411960070020101
Sumikawa DA, Marshall GW, Gee L, Marshall SJ (1999) Microstructure of primary tooth dentin. Pediatric Dentistry 21:439–444
Shah D, Lynd T, Ho D, Chen J, Vines J, Jung HD, Kim JH, Zhang P, Wu H, Jun HW, Cheon K (2020) Pulp-dentin tissue healing response: a discussion of current biomedical approaches. Journal of clinical medicine 9:434. https://doi.org/10.3390/jcm9020434
Castelnuovo J, Tjan AH (1997) Temperature rise in pulpal chamber during fabrication of provisional resinous crowns. The Journal of Prosthetic Dentistry 78:441–446. https://doi.org/10.1016/s0022-3913(97)70057-x
Daronch M, Rueggeberg FA, Hall G, De Goes MF (2007) Effect of composite temperature on in vitro intrapulpal temperature rise. Dental Materials 23:1283–1288. https://doi.org/10.1016/j.dental.2006.11.024
Hannig M, Bott B (1999) In-vitro pulp chamber temperature rise during composite resin polymerization with various light-curing sources. Dental Materials 15:275–281. https://doi.org/10.1016/S0109-5641(99)00047-0
Abbott PV, Yu C (2007) A clinical classification of the status of the pulp and the root canal system. Australian Dental Journal 52:S17–S31. https://doi.org/10.1111/j.1834-7819.2007.tb00522.x
Langeland K, Langeland LK (1965) Pulp reactions to crown preparation, impression, temporary crown fixation and permanent cementation. The Journal of Prosthetic Dentistry 15:129–143. https://doi.org/10.1016/0022-3913(65)90073-9
Pohto M, Scheinin A (1958) Microscopic observations on living dental pulp II. The effect of thermal irritants on the circulation of the pulp in the lower rat incisor. Acta Odontologica Scandinavica 16:315–327. https://doi.org/10.3109/00016355809064116
Altintas SH, Yondem I, Tak O, Usumez A (2008) Temperature rise during polymerization of three different provisional materials. Clinical Oral Investigations 12:283–286. https://doi.org/10.1007/s00784-007-0163-7
Kells BE, Kennedy JG, Biagioni PA, Lamey PJ (2000) Computerized infrared thermographic imaging and pulpal blood flow: part 1. A protocol for thermal imaging of human teeth. International Endodontic Journal 33:442–447. https://doi.org/10.1046/j.1365-2591.2000.00257.x
Lipski M, Wozniak K, Szyszka-Sommerfeld L, Borawski M, Drozdzik A, Nowicka A (2020) In vitro infrared thermographic assessment of temperature change in the pulp chamber during provisionalization: effect of remaining dentin thickness. Journal of Healthcare Engineering 2020:1–5. https://doi.org/10.1155/2020/8838329
Singh R, Tripathi A, Dhiman RK, Kumar D (2015) Intrapulpal thermal changes during direct provisionalization using various autopolymerizing resins: ex-vivo study. Medical Journal Armed Forces India 71:S313–S320. https://doi.org/10.1016/j.mjafi.2013.02.005
Jacobs HR, Thompson RE, Brown WS (1973) Heat transfer in teeth. Journal of Dental Research 52:248–252. https://doi.org/10.1177/00220345730520021101
Chua H, Choi JJE, Ramani RS, Ganjigatti R, Waddell JN (2019) The cooling efficiency of different dental high-speed handpiece coolant port designs. Heliyon 5:e02185. https://doi.org/10.1016/j.heliyon.2019.e02185
Firoozmand L, Faria R, Araujo MA, di Nicoló R, Huthala MF (2008) Temperature rise in cavities prepared by high and low torque handpieces and Er:YAG laser. British Dental Journal 205:E1. https://doi.org/10.1038/sj.bdj.2008.491
Fouad AF, Levin L (2011) Pulpal reactions to caries and dental procedures. In: Hargreaves KM, Cohen S (eds) Cohen's pathways of the pulp, 10th edn. Mosby Elsevier, St. Louis, pp 504–528
Kwon SJ, Park YJ, Jun SH, Ahn JS, Lee IB, Cho BH, Son HH, Seo DG (2013) Thermal irritation of teeth during dental treatment procedures. Restor Dent Endod 38:105–112. https://doi.org/10.5395/rde.2013.38.3.105
Lauer HC, Kraft E, Rothlauf W, Zwingers T (1990) Effects of the temperature of cooling water during high-speed and ultrahigh-speed tooth preparation. The Journal of Prosthetic Dentistry 63:407–414. https://doi.org/10.1016/0022-3913(90)90228-5
Vanderlei AD, Borges AL, Cavalcanti BN, Rode SM (2008) Ultrasonic versus high-speed cavity preparation: analysis of increases in pulpal temperature and time to complete preparation. The Journal of Prosthetic Dentistry 100:107–109. https://doi.org/10.1016/S0022-3913(08)60158-4
Lempel E, Őri Z, Kincses D, Lovász BV, Kunsági-Máté S, Szalma J (2021) Degree of conversion and in vitro temperature rise of pulp chamber during polymerization of flowable and sculptable conventional, bulk-fill and short-fibre reinforced resin composites. Dental Materials 37:983–997. https://doi.org/10.1016/j.dental.2021.02.013
Szalma J, Vajta L, Olasz L, Lempel E (2019) Tooth sectioning for coronectomy: how to perform? Clinical Oral Investigations 23:519–527. https://doi.org/10.1007/s00784-018-2466-2
Helmer J, Driskell T (1969) Research on bioceramics: symposium on use of ceramics as surgical implants. Clemson University
Shen C, Rawls HR, Esquivel-Upshaw JF (2021) Physical and chemical properties of solids. In: Phillips’ Science of Dental Materials, 13th edn. Elsevier, St. Louis, pp 49–63
Brown WS, Dewey WA, Jacobs HR (1970) Thermal properties of teeth. Journal of Dental Research 49:752–755. https://doi.org/10.1177/00220345700490040701
Kim SH, Watts DC (2004) Exotherm behavior of the polymer-based provisional crown and fixed partial denture materials. The Journal of Prosthetic Dentistry 91:569–569. https://doi.org/10.1016/j.prosdent.2004.04.006
Tjan AH, Grant BE, Godfrey MF III (1989) Temperature rise in the pulp chamber during fabrication of provisional crowns. The Journal of Prosthetic Dentistry 62:622–626. https://doi.org/10.1016/0022-3913(89)90578-7
Seelbach P, Finger WJ, Ferger P, Balkenhol M (2010) Temperature rise on dentin caused by temporary crown and fixed partial denture materials: influencing factors. Journal of Dentistry 38:964–973. https://doi.org/10.1016/j.jdent.2010.08.008
Soori A, Soori F, Kowsary F, Kasraei S (2022) Thermal conductivity and diffusivity of human enamel and dentin measured by the laser flash method. International Journal of Thermophysics 43:158. https://doi.org/10.1007/s10765-022-03083-0
Lancaster P, Brettle D, Carmichael F, Clerehugh V (2017) In-vitro thermal maps to characterize human dental enamel and dentin. Frontiers in physiology 8:461. https://doi.org/10.3389/fphys.2017.00461
de Magalhaes MF, Ferreira RAN, Grossi PA, de Andrade RM (2008) Measurement of thermophysical properties of human dentin: effect of open porosity. Journal of dentistry 36:588–594. https://doi.org/10.1016/j.jdent.2008.04.006
Bhandary N, Desai A, Shetty YB (2014) High speed handpieces. Journal of International Oral Health 6:130–132
Farah RI (2019) Effect of cooling water temperature on the temperature changes in pulp chamber and at handpiece head during high-speed tooth preparation. Restor Dent Endod 44:e3. https://doi.org/10.5395/rde.2019.44.e3
Ercoli C, Rotella M, Funkenbusch PD, Russell S, Feng C (2009) In vitro comparison of the cutting efficiency and temperature production of ten different rotary cutting instruments. Part II: electric handpiece and comparison with turbine. The Journal of Prosthetic Dentistry 101:319–331. https://doi.org/10.1016/S0022-3913(09)60064-0
Choi C, Driscoll CF, Romberg E (2010) Comparison of cutting efficiencies between electric and air-turbine dental handpieces. The Journal of Prosthetic Dentistry 103:101–107. https://doi.org/10.1016/S0022-3913(10)60013-3
Christensen GJ (2002) Are electric handpieces an improvement? The Journal of the American Dental Association 133:1433–1434. https://doi.org/10.14219/jada.archive.2002.0061
Kenyon BJ, Van Zyl I, Louie KG (2005) Comparison of cavity preparation quality using an electric motor handpiece and an air turbine dental handpiece. The Journal of the American Dental Association 136:1101–1166. https://doi.org/10.14219/jada.archive.2005.0313
KaVo (2021) https://www.kavo.com/en-us/handpieces-small-equipment
Öztürk B, Üşümez A, Öztürk AN, Ozer F (2004) In vitro assessment of temperature change in the pulp chamber during cavity preparation. The Journal of Prosthetic Dentistry 91:436–440. https://doi.org/10.1016/j.prosdent.2004.02.022
Watson TF, Flanagan D, Stone DG (2000) High and low torque handpieces: cutting dynamics, enamel cracking and tooth temperature. British Dental Journal 188:680–686. https://doi.org/10.1038/sj.bdj.4800576
Center for Devices and Radiological Health (2017) Letter to electric dental handpiece manufacturers regarding reports of overheating and patient burns: notice of safety concern for electric dental handpieces and accessories. U.S. Food And Drug Administration. http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm226986.htm
Sarrett DC (2014) A laboratory evaluation of electric handpiece temperature and the associated risk of burns. ADA Prof Prod Rev 9:18–24
Ercoli C, Rotella M, Funkenbusch PD, Russell S, Feng C (2009) In vitro comparison of the cutting efficiency and temperature production of 10 different rotary cutting instruments. Part I: Turbine. The Journal of Prosthetic Dentistry 101:248–261. https://doi.org/10.1016/S0022-3913(09)60049-4
Galindo DF, Ercoli C, Funkenbusch PD, Greene TD, Moss ME, Lee H-J, Ben-Hanan U, Graser GN, Barzilay I (2004) Tooth preparation: a study on the effect of different variables and a comparison between conventional and channeled diamond burs. Journal of Prosthodontics 13:3–16. https://doi.org/10.1111/j.1532-849X.2004.04003.x
Schuchard A (1962) Action of water coolants with ultra-high rotating speeds. The Journal of Prosthetic Dentistry 12:559–565. https://doi.org/10.1016/0022-3913(62)90140-3
Siegel SC, von Fraunhofer JA (2002) The effect of handpiece spray patterns on cutting efficiency. The Journal of the American Dental Association 133:184–188. https://doi.org/10.14219/jada.archive.2002.0142
Lau XE, Ma S, Choi JJE (2023) New aerosol-decreasing dental handpiece functions sufficiently decrease pulp temperature: an in vitro study. J Prosthodont. https://doi.org/10.1111/jopr.13672
Yang WJ, Sun J (2013) Effect of the spray pattern, water flow rate, and cutting position on the cutting efficiency of high-speed dental handpieces. The International Journal of Prosthodontics 26:85–87. https://doi.org/10.11607/ijp.3008
Lloyd BA, Rich JA, Brown WS (1978) Effect of cooling techniques on temperature control and cutting rate for high-speed dental drills. Journal of Dental Research 57:675–684. https://doi.org/10.1177/00220345780570050201
Morrant GA (1977) Dental instrumentation and pulpal injury. Part II-Clinical Considerations. Journal of the British Endodontic Society 10:55–63. https://doi.org/10.1111/j.1365-2591.1977.tb00644.x
Sharma S, Shankar R, Srinivas K (2014) An epidemiological study on the selection, usage and disposal of dental burs among the dental practioner's. Journal of Clinical and Diagnostic Research 8:250–254. https://doi.org/10.7860/JCDR/2014/5916.3946
Evans CD, Wilson PR (1999) The effects of tooth preparation on pressure measured in the pulp chamber: a laboratory study. International Journal of Prosthodontics 12:439–443
Siegel SC, von Fraunhofer JA (1996) Assessing the cutting efficiency of dental diamond burs. The Journal of the American Dental Association 127:763–772. https://doi.org/10.14219/jada.archive.1996.0312
Boyde A (1976) Enamel structure and cavity margins. Operative Dentistry 1:13–28
Funkenbusch PD, Rotella M, Chochlidakis K, Ercoli C (2016) Multivariate evaluation of the cutting performance of rotary instruments with electric and air-turbine handpieces. The Journal of Prosthetic Dentistry 116:558–563. https://doi.org/10.1016/j.prosdent.2016.03.002
Ottl P, Lauer HC (1998) Temperature response in the pulpal chamber during ultrahigh-speed tooth preparation with diamond burs of different grit. The Journal of Prosthetic Dentistry 80:12–19. https://doi.org/10.1016/s0022-3913(98)70085-x
Chung EM, Sung EC, Wu B, Caputo AA (2006) Comparing cutting efficiencies of diamond burs using a high-speed electric handpiece. General dentistry 54:254–257
Siegel SC, von Fraunhofer JA (1997) Effect of handpiece load on the cutting efficiency of dental burs. Machining Science and Technology 1:1–13. https://doi.org/10.1080/10940349708945634
Ohmoto K, Taira M, Shintani H, Yamaki M (1994) Studies on dental high-speed cutting with carbide burs used on bovine dentin. The Journal of Prosthetic Dentistry 71:319–323. https://doi.org/10.1016/0022-3913(94)90475-8
Cavalcanti BN, Otani C, Rode SM (2002) High-speed cavity preparation techniques with different water flows. The Journal of Prosthetic Dentistry 87:158–161. https://doi.org/10.1067/mpr.2002.120655
Stanley HR (1961) Traumatic capacity of high-speed and ultrasonic dental instrumentation. The Journal of the American Dental Association 63:749–766. https://doi.org/10.14219/jada.archive.1961.0303
Marsland E, Shovelton D (1970) Repair in the human dental pulp following cavity preparation. Archives of Oral Biology 15:411–422. https://doi.org/10.1016/0003-9969(70)90068-3
Schuchard A (1975) A histologic assessment of low-torque, ultrahigh-speed cutting technique. The Journal of Prosthetic Dentistry 34:644–651. https://doi.org/10.1016/0022-3913(75)90062-1
Bhaskar S, Lilly GE (1965) Intrapulpal temperature during cavity preparation. Journal of Dental Research 44:644–647. https://doi.org/10.1177/00220345650440040601
Brown WS, Christensen DO, Lloyd B (1978) Numerical and experimental evaluation of energy inputs, temperature gradients, and thermal stresses during restorative procedures. The Journal of the American Dental Association 96(3):451–458. https://doi.org/10.14219/jada.archive.1978.0116
Cavalcanti BN, Lage-Marques JL, Rode SM (2003) Pulpal temperature increases with Er:YAG laser and high-speed handpieces. The Journal of Prosthetic Dentistry 90:447–451. https://doi.org/10.1016/j.prosdent.2003.08.022
Peyton FA (1955) Temperature rise in teeth developed by rotating instruments. The Journal of the American Dental Association 50:629–632. https://doi.org/10.14219/jada.archive.1955.0117
Zach L, Cohen G (1962) Thermogenesis in operative techniques: comparison of four methods. The Journal of Prosthetic Dentistry 12:977–984. https://doi.org/10.1016/0022-3913(62)90051-3
Siegel SC, von Fraunhofer JA (2000) Irrigation rates and handpieces used in prosthodontic and operative dentistry: results of a survey of North American dental school teaching. Journal of Prosthodontics 9:82–86. https://doi.org/10.1111/j.1532-849x.2000.00082.x
von Fraunhofer JA, Siegel SC, Feldman S (2000) Handpiece coolant flow rates and dental cutting. Operative Dentistry 25:544–548
International Organization for Standardization (2012) ISO 14457:2012 Dentistry – handpieces and motors. https://www.iso.org/standard/54805.html
Cavalcanti BN, Serairdarian PI, Rode SM (2005) Water flow in high-speed handpieces. Quintessence international 36:361–364
Leung BT, Dyson JE, Darvell BW (2012) Coolant effectiveness in dental cutting with air-turbine handpieces. New Zealand Dental Journal 108:25–29
Raab WH (1992) Temperature related changes in pulpal microcirculation. Proc Finn Dent Soc 88:469–479
Wassell RW, St George G, Ingledew RP, Steele JG (2002) Crowns and other extra-coronal restorations: provisional restorations. British Dental Journal 192:619–630. https://doi.org/10.1038/sj.bdj.4801443
Burns DR, Beck DA, Nelson SK (2003) A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. The Journal of Prosthetic Dentistry 90:474–497. https://doi.org/10.1016/s0022-3913(03)00259-2
Michalakis K, Pissiotis A, Hirayama H, Kang K, Kafantaris N (2006) Comparison of temperature increase in the pulp chamber during the polymerization of materials used for the direct fabrication of provisional restorations. The Journal of Prosthetic Dentistry 96:418–423. https://doi.org/10.1016/j.prosdent.2006.10.005
Abdullah AO, Tsitrou EA, Pollington S (2016) Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. Journal of Applied Oral Science 24:258–263. https://doi.org/10.1590/1678-775720150451
Tjan AH, Castelnuovo J, Shiotsu G (1997) Marginal fidelity of crowns fabricated from six proprietary provisional materials. The Journal of Prosthetic Dentistry 77:482–485. https://doi.org/10.1016/s0022-3913(97)70140-9
Khajuria RR, Madan R, Agarwal S, Gupta R, Vadavadgi SV, Sharma V (2015) Comparison of temperature rise in pulp chamber during polymerization of materials used for direct fabrication of provisional restorations: an in-vitro study. European journal of dentistry 9:194–200. https://doi.org/10.4103/1305-7456.156807
Ramkumar V, Sangeetha A, Kumar V (2012) Effect of water temperature on the fit of provisional crown margins during polymerization: an in vitro study. Journal of Pharmacy & Bioallied Sciences 4:376–383. https://doi.org/10.4103/0975-7406.100288
Bouillaguet S (2004) Biological risks of resin-based materials to the dentin-pulp complex. Critical Reviews in Oral Biology & Medicine 15:47–60. https://doi.org/10.1177/154411130401500105
Fuks AB, Funnell B, Cleaton-Jones P (1990) Pulp response to a composite resin inserted in deep cavities with and without a surface seal. The Journal of prosthetic dentistry 63:129–134. https://doi.org/10.1016/0022-3913(90)90094-s
Chalifoux PR (2015) Acrylic and other resins: provisional restorations. In: Aschheim KW (ed) Esthetic Dentistry, 3rd edn. Elsevier, Mosby, pp 197–230. https://doi.org/10.1016/b978-0-323-09176-3.00019-x
Dias M, Choi JJE, Uy CE, Ramani RS, Ganjigatti R, Waddell JN (2019) Real-time pulp temperature change at different tooth sites during fabrication of temporary resin crowns. Heliyon 5:e02971. https://doi.org/10.1016/j.heliyon.2019.e02971
Anusavice KJ, Shen C, Rawls HR (2013) Dental ceramics. In: Phillips’ Science of Dental Materials, 12th edn. Saunders, London, pp 418–473
Salama SN, Salman SM, Gharib S (1987) Thermal conductivity of some silicate glasses and their respective crystalline products. Journal of Non-Crystalline Solids 93:203–214. https://doi.org/10.1016/s0022-3093(87)80039-x
Baldissara P, Catapano S, Scotti R (2008) Clinical and histological evaluation of thermal injury thresholds in human teeth: a preliminary study. Journal of Oral Rehabilitation 24:791–801. https://doi.org/10.1111/j.1365-2842.1997.tb00278.x
Dupriez ND, Von Koeckritz AK, Kunzelmann KH (2014) A comparative study of sliding wear of nonmetallic dental restorative materials with emphasis on micromechanical wear mechanisms. Journal of Biomedical Materials Research Part B: Applied Biomaterials 103:925–934. https://doi.org/10.1002/jbm.b.33193
Chavali R, Lin CP, Lawson NC (2017) Evaluation of different polishing systems and speeds for dental zirconia. Journal of Prosthodontics 26:410–418. https://doi.org/10.1111/jopr.12396
İşeri U, Özkurt Z, Yalnız A, Kazazoğlu E (2012) Comparison of different grinding procedures on the flexural strength of zirconia. The Journal of Prosthetic Dentistry 107:309–315. https://doi.org/10.1016/s0022-3913(12)60081-x
Trujillo M, Newman SM, Stansbury JW (2004) Use of near-IR to monitor the influence of external heating on dental composite photopolymerization. Dental Materials 20:766–777. https://doi.org/10.1016/j.dental.2004.02.003
Balestrino A, Veríssimo C, Tantbirojn D, Garcia-Godoy F, Soares CJ, Versluis A (2016) Heat generated during light-curing of restorative composites: effect of curing light, exotherm, and experiment substrate. American Journal of Dentistry 29:234–2240
Armellin E, Bovesecchi G, Coppa P, Pasquantonio G, Cerroni L (2016) LED curing lights and temperature changes in different tooth sites. BioMed Research International 2016:1–10. https://doi.org/10.1155/2016/1894672
Par M, Gamulin O, Marovic D, Klaric E, Tarle Z (2014) Effect of temperature on post-cure polymerization of bulk-fill composites. Journal of Dentistry 42:1255–1260. https://doi.org/10.1016/j.jdent.2014.08.004
Uhl A, Mills RW, Jandt KD (2003) Photoinitiator dependent composite depth of cure and Knoop hardness with halogen and LED light curing units. Biomaterials 24:1787–1795. https://doi.org/10.1016/s0142-9612(02)00532-x
Anić I, Vidović D, Luić M, Tudja M (1992) Laser induced molar tooth pulp chamber temperature changes. Caries Research 26:165–169. https://doi.org/10.1159/000261437
Burkes EJ Jr, Hoke J, Gomes E, Wolbarsht M (1992) Wet versus dry enamel ablation by Er:YAG laser. The Journal of Prosthetic Dentistry 67:847–851. https://doi.org/10.1016/0022-3913(92)90599-6
Chang JC, Wilder-Smith P (1998) Laser-induced thermal events in empty and pulp-filled dental pulp chambers. Lasers in Surgery and Medicine 22:46–50. https://doi.org/10.1002/(SICI)1096-9101(1998)22:1%3C46::AID-LSM11%3E3.0.CO;2-6
Glockner K, Rumpler J, Ebeleseder K, Städtler P (1998) Intrapulpal temperature during preparation with the Er:YAG laser compared to the conventional burr: an in vitro study. Journal of Clinical Laser Medicine & Surgery 16(3):153–157. https://doi.org/10.1089/clm.1998.16.153
Gow AM, McDonald AV, Pearson GJ, Setchell DJ (1999) An in vitro investigation of the temperature rises produced in dentine by Nd:YAG laser light with and without water cooling. The European Journal of Prosthodontics and Restorative Dentistry 7:71–77
Hoke JA, Burkes EJ Jr, Gomes ED, Wolbarsht ML (1990) Erbium:YAG (2.94 μm) laser effects on dental tissues. Journal of Laser Applications 2:61–65. https://doi.org/10.2351/1.4745270
Laforgia PD, Milano V, Morea C, Desiate A (1991) Temperature change in the pulp chamber during complete crown preparation. The Journal of Prosthetic Dentistry 65:56–61. https://doi.org/10.1016/0022-3913(91)90048-2
Neev J, Pham K, Lee JP, White JM (1996) Dentin ablation with three infrared lasers. Lasers in Surgery and Medicine 18:121–128. https://doi.org/10.1002/(SICI)1096-9101(1996)18:2%3C121::AID-LSM1%3E3.0.CO;2-U
Paghdiwala AF, Vaidyanathan TK, Paghdiwala MF (1993) Evaluation of erbium:YAG laser radiation of hard dental tissues: analysis of temperature changes, depth of cuts and structural effects. Scanning Microscopy 7:989–997
Schuchard A, Watkins CE (1965) Thermal and histologic response to high-speed and ultrahigh-speed cutting in tooth structure. The Journal of the American Dental Association 71:1451–1458. https://doi.org/10.14219/jada.archive.1965.0009
Visuri SR, Walsh JT Jr, Wigdor HA (1996) Erbium laser ablation of dental hard tissue: effect of water cooling. Lasers in Surgery and Medicine 18:294–300. https://doi.org/10.1002/(SICI)1096-9101(1996)18:3%3C294::AID-LSM11%3E3.0.CO;2-6
Uhl A, Völpel A, Sigusch BW (2006) Influence of heat from light curing units and dental composite polymerization on cells in vitro. Journal of Dentistry 34:298–306. https://doi.org/10.1016/j.jdent.2005.07.004
Xu HHK, Kelly JR, Jahanmir S, Thompson VP, Rekow ED (1997) Enamel subsurface damage due to tooth preparation with diamonds. Journal of Dental Research 76:1698–1706. https://doi.org/10.1177/00220345970760101201
Kodonas K, Gogos C, Tziafa C (2009) Effect of simulated pulpal microcirculation on intrachamber temperature changes following application of various curing units on tooth surface. Journal of Dentistry 37:485–490. https://doi.org/10.1016/j.jdent.2009.03.006
Goodis HE, Winthrop V, White JM (2000) Pulpal responses to cooling tooth temperatures. Journal of Endodontics 26:263–267. https://doi.org/10.1097/00004770-200005000-00001
Plasmans PJMM, Creugers NHJ, Hermsen RJ, Vrijhoef MMA (1994) Intraoral humidity during operative procedures. Journal of Dentistry 22:89–91. https://doi.org/10.1016/0300-5712(94)90007-8
Amsler F, Peutzfeldt A, Lussi A, Flury S (2015) Bond strength of resin composite to dentin with different adhesive systems: influence of relative humidity and application time. Journal of Adhesive Dentistry 17:249–256. https://doi.org/10.3290/j.jad.a34400
Park HN, Lim YJ, Yi WJ, Han JS, Lee SP (2018) A comparison of the accuracy of intraoral scanners using an intraoral environment simulator. The Journal of Advanced Prosthodontics 10:58–64. https://doi.org/10.4047/jap.2018.10.1.58
Farah RI (2017) Effect of simulated pulpal blood flow rate on the rise in pulp chamber temperature during direct fabrication of exothermic provisional restorations. International Endodontic Journal 50:1097–1103. https://doi.org/10.1111/iej.12735
Goodis HE, Schein B, Stauffer P (1988) Temperature changes measured in vivo at the dentinoenamel junction and pulpodentin junction during cavity preparation in the Macaca fascicularis monkey. Journal of Endodontics 14:336–339. https://doi.org/10.1016/S0099-2399(88)80194-8
Mülle H, Raab WHM (1990) Einfluß der Lokalanästhesie auf die Thermoregulation der Zahnpulpa. Deutsche Zahnarztliche Zeitschrift 45:216–218
Linsuwanont P, Palamara JEA, Messer HH (2007) An investigation of thermal stimulation in intact teeth. Archives of Oral Biology 52:218–227. https://doi.org/10.1016/j.archoralbio.2006.10.009
Attrill DC, Davies RM, King TA, Dickinson MR, Blinkhorn AS (2004) Thermal effects of the Er:YAG laser on a simulated dental pulp: a quantitative evaluation of the effects of a water spray. Journal of Dentistry 32:35–40. https://doi.org/10.1016/S0300-5712(03)00137-4
Amsler F, Peutzfeldt A, Lussi A, Flury S (2017) Long-term bond strength of self-etch adhesives to normal and artificially eroded dentin: effect of relative humidity and saliva contamination. Journal of Adhesive Dentistry 19:169–176. https://doi.org/10.3290/j.jad.a38101
Bicalho AA, de Souza SJB, de Rosatto CMP, Tantbirojn D, Versluis A, Soares CJ (2015) Effect of temperature and humidity on post-gel shrinkage, cusp deformation, bond strength and shrinkage stress – construction of a chamber to simulate the oral environment. Dental Materials 31:1523–1532. https://doi.org/10.1016/j.dental.2015.09.023
Walker MP, Haj-Ali R, Wang Y, Hunziker D, Williams KB (2006) Influence of environmental conditions on dental composite flexural properties. Dental Materials 22:1002–1007. https://doi.org/10.1016/j.dental.2005.11.023
Funkenbusch PD, Rotella M, Ercoli C (2015) Designed experiment evaluation of key variables affecting the cutting performance of rotary instruments. The Journal of Prosthetic Dentistry 113:336–342. https://doi.org/10.1016/j.prosdent.2014.10.002
Gross DJ, Dávila-Sánchez A, Runnacles P, Zarpellon DC, Kiratcz F, Campagnoli EB, Alegría-Acevedo LF, Coelho U, Rueggeberg FA, Arrais CAG (2020) In vivo temperature rise and acute inflammatory response in anesthetized human pulp tissue of premolars having Class V preparations after exposure to Polywave® LED light curing units. Dental Materials 36:1201–1213. https://doi.org/10.1016/j.dental.2020.05.015
Haenel T, Hausnerová B, Steinhaus J, Price RB, Sullivan B, Moeginger B (2015) Effect of the irradiance distribution from light curing units on the local micro-hardness of the surface of dental resins. Dental Materials 31:93–104. https://doi.org/10.1016/j.dental.2014.11.003
Alkhudhairy FI (2017) The effect of curing intensity on mechanical properties of different bulk-fill composite resins. Clinical, Cosmetic and Investigational Dentistry 9:1–6. https://doi.org/10.2147/CCIDE.S130085
Daugherty MM, Lien W, Mansell MR, Risk DL, Savett DA, Vandewalle KS (2018) Effect of high-intensity curing lights on the polymerization of bulk-fill composites. Dental Materials 34:1531–1541. https://doi.org/10.1016/j.dental.2018.06.005
Shimokawa CAK, Turbino ML, Giannini M, Braga RR, Price RB (2018) Effect of light curing units on the polymerization of bulk fill resin-based composites. Dental Materials 34:1211–1221. https://doi.org/10.1016/j.dental.2018.05.002
Sahadi BO, Price RB, André CB, Sebold M, Bermejo GN, Palma-Dibb RG, Faraoni JJ, Soares CJ, Giannini M (2018) Multiple-peak and single-peak dental curing lights comparison on the wear resistance of bulk-fill composites. Brazilian oral research 32:e122. https://doi.org/10.1590/1807-3107bor-2018.vol32.0122
Germscheid W, de Gorre LG, Sullivan B, O'Neill C, Price RB, Labrie D (2018) Post-curing in dental resin-based composites. Dental Materials 34:1367–1377. https://doi.org/10.1016/j.dental.2018.06.021
Par M, Repusic I, Skenderovic H, Milat O, Spajic J, Tarle Z (2019) The effects of extended curing time and radiant energy on microhardness and temperature rise of conventional and bulk-fill resin composites. Clinical Oral Investigations 23:3777–3788. https://doi.org/10.1007/s00784-019-02807-1
Marzouk AM, Niazi HAA, Mohammed MN, Afifi RH (2019) Effect of curing time on top to bottom microhardness of bulk-fill composite. Egyptian Dental Journal 65:1733–1739. https://doi.org/10.21608/edj.2019.72929
Ilie N, Watts DC (2020) Outcomes of ultra-fast (3 s) photo-cure in a RAFT-modified resin-composite. Dental Materials 36:570–579. https://doi.org/10.1016/j.dental.2020.02.007
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
Conceptualisation: JJEC; data curation: XEL, XL, HC, WJW, MD, JJEC; formal analysis: XEL, XL, HC, WJW, MD, JJEC; investigation: XEL, XL, HC, WJW, MD, JJEC; methodology: JJEC; project administration: JJEC; writing—original draft: XEL, XL, HC, WJW, MD, JJEC; writing—review and editing: XEL, XL, HC, WJW, MD, JJEC.
Corresponding author
Ethics declarations
Ethical approval
Not applicable as this is a literature review
Competing interests
The authors declare no competing interests
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lau, X.E., Liu, X., Chua, H. et al. Heat generated during dental treatments affecting intrapulpal temperature: a review. Clin Oral Invest 27, 2277–2297 (2023). https://doi.org/10.1007/s00784-023-04951-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04951-1