Abstract
Objective
Successful application of deep machine learning could reduce time-consuming and labor-intensive clinical work of calculating the amount of radiographic bone loss (RBL) in diagnosing and treatment planning for periodontitis. This study aimed to test the accuracy of RBL classification by machine learning.
Materials and methods
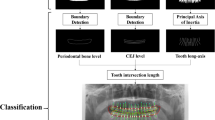
A total of 236 patients with standardized full mouth radiographs were included. Each tooth from the periapical films was evaluated by three calibrated periodontists for categorization of RBL and radiographic defect morphology. Each image was pre-processed and augmented to ensure proper data balancing without data pollution, then a novel multitasking InceptionV3 model was applied.
Results
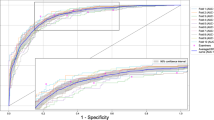
The model demonstrated an average accuracy of 0.87 ± 0.01 in the categorization of mild (< 15%) or severe (≥ 15%) bone loss with fivefold cross-validation. Sensitivity, specificity, positive predictive, and negative predictive values of the model were 0.86 ± 0.03, 0.88 ± 0.03, 0.88 ± 0.03, and 0.86 ± 0.02, respectively.
Conclusions
Application of deep machine learning for the detection of alveolar bone loss yielded promising results in this study. Additional data would be beneficial to enhance model construction and enable better machine learning performance for clinical implementation.
Clinical relevance
Higher accuracy of radiographic bone loss classification by machine learning can be achieved with more clinical data and proper model construction for valuable clinical application.





Similar content being viewed by others
References
Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ (2012) Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res 91(10):914–920. https://doi.org/10.1177/0022034512457373
Eke PI et al (2015) Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 86(5):611–622. https://doi.org/10.1902/jop.2015.140520
Page R, Schroeder H (1976) “Pathogenesis of inflammatory periodontal disease. A summary of current work,” Laboratory investigation. J Technical Methods Pathol 34(3):235–249
Richards D (2014) Review finds that severe periodontitis affects 11% of the world population. Evid Based Dent 15(3):70–71. https://doi.org/10.1038/sj.ebd.6401037
Borgnakke WS, Yl€ostalo PV, Taylor GW, Genco RJ (2013) “Effect of periodontal disease on diabetes: systematic review of epidemiologic observational evidence,.” J Periodontology 84(4S):S135–S152. https://doi.org/10.1902/jop.2013.1340013
Chapple ILC, Genco R, on behalf of working group 2 of the joint E. workshop* (2013) “Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases,.” J Periodontology 84(4S):S106–S112. https://doi.org/10.1902/jop.2013.1340011
Tonetti MS, Van Dyke TE, on behalf of working group 1 of the joint E. workshop* (2013) “Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAPWorkshop on Periodontitis and Systemic Diseases,.” J Periodontology 84(4S):S24-29. https://doi.org/10.1902/jop.2013.1340019
Schenkein HA, Loos BG (2013) Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases. J Periodontol 84(4S):S51–S69. https://doi.org/10.1902/jop.2013.134006
Gomes-Filho IS et al (2020) Periodontitis and respiratory diseases: a systematic review with meta-analysis. Oral Dis 26(2):439–446. https://doi.org/10.1111/odi.13228
Sanz M, Kornman K, on behalf of working group 3 of the joint E. workshop (2013) Periodontitis and adverse pregnancy outcomes: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Periodontol 84(4S):S164–S169. https://doi.org/10.1902/jop.2013.1340016
Noble JM, Borrell LN, Papapanou PN, Elkind MSV, Scarmeas N, Wright CB (2009) “Periodontitis is associated with cognitive impairment among older adults: analysis of NHANES-III,.” J Neurol Neurosurg Psychiatry 80(11):1206. https://doi.org/10.1136/jnnp.2009.174029
Chapple ILC et al (2018) Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(S1):S74–S84. https://doi.org/10.1002/JPER.17-0719
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol 89(S1):S159–S172. https://doi.org/10.1002/JPER.18-0006
Hausmann E, Allen K, Clerehugh V (1991) What alveolar crest level on a bite-wing radiograph represents bone loss? J Periodontol 62(9):570–572. https://doi.org/10.1902/jop.1991.62.9.570
Schei O, Waerhaug J, Lovdal A, Arno A (1959) Alveolar bone loss as related to oral hygiene and age. J Periodontology 30(1):7–16. https://doi.org/10.1902/jop.1959.30.1.7
Gelfand M, Sunderman EJ, Goldman M (1983) Reliability of radiographical interpretations. J Endodontics 9(2):71–75. https://doi.org/10.1016/S0099-2399(83)80079-X
Valachovic RW, Douglass CW, Berkey CS, McNeil BJ, Chauncey HH (1986) Examiner reliability in dental radiography. J Dent Res 65(3):432–436. https://doi.org/10.1177/00220345860650031201
Benn DK (1990) A review of the reliability of radiographic measurements in estimating alveolar bone changes. J Clin Periodontol 17(1):14–21. https://doi.org/10.1111/j.1600-051X.1990.tb01041.x
Obermeyer Z, Emanuel EJ (2016) Predicting the future - big data, machine learning, and clinical medicine. N Engl J Med 375(13):1216–1219. https://doi.org/10.1056/NEJMp1606181
McBee MP et al (2018) Deep learning in radiology. Acad Radiol 25(11):1472–1480. https://doi.org/10.1016/j.acra.2018.02.018
Lo S-CB, Chan H-P, Lin J-S, Li H, Freedman MT, Mun SK (1995) Artificial convolution neural network for medical image pattern recognition. Neural Netw 8(7):1201–1214. https://doi.org/10.1016/0893-6080(95)00061-5
Y. Yu, (2016) “Machine learning for dental image analysis,” ArXiv, abs/1611.09958.
P. Rajpurkar et al., (2017) “CheXNet: radiologist-level pneumonia detection on chest X-rays with deep learning,” CoRR, abs/1711.05225, [Online]. Available: http://arxiv.org/abs/1711.05225
Lee J-H, Kim D-H, Jeong S-N, Choi S-H (2018) Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. J Dent 77:106–111. https://doi.org/10.1016/j.jdent.2018.07.015
Krois J et al (2019) “Deep learning for the radiographic detection of periodontal bone loss,.” Sci Rep 9(1):8495. https://doi.org/10.1038/s41598-019-44839-3
Chang H-J et al (2020) “Deep learning hybrid method to automatically diagnose periodontal bone loss and stage periodontitis,.” Scientific Rep 10(1):7531. https://doi.org/10.1038/s41598-020-64509-z
Kim J, Lee H-S, Song I-S, Jung K-H (2019) “DeNTNet: Deep Neural Transfer Network for the detection of periodontal bone loss using panoramic dental radiographs,.” Scientific Rep 9(1):17615. https://doi.org/10.1038/s41598-019-53758-2
MBH. Moran, M. Faria, G. Giraldi, L. Bastos, B. da S. Inacio, A. Conci, (2020) “On using convolutional neural networks to classify periodontal bone destruction in periapical radiographs,” in 2020 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), 2036–2039. https://doi.org/10.1109/BIBM49941.2020.9313501
Burman P (1989) “A comparative study of ordinary cross-validation, v-fold cross-validation and the repeated learning-testing methods,.” Biometrika 76(3):503–514. https://doi.org/10.1093/biomet/76.3.503
Russell (2008) LabelMe. https://github.com/wkentaro/labelme/releases/tag/v4.5.7. Accessed 15 March 2021.
Reza AM (2004) Realization of the contrast limited adaptive histogram equalization (CLAHE) for real-time image enhancement. J VLSI signal Process Syst signal, Image Video Technol 38(1):35–44. https://doi.org/10.1023/B:VLSI.0000028532.53893.82
Pizer SM et al (1987) Adaptive histogram equalization and its variations. Computer Vision, Graphics, Image Process 39(3):355–368. https://doi.org/10.1016/S0734-189X(87)80186-X
Szegedy, (2016) “Rethinking the inception architecture for computer vision,” roceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR).
Caton JG et al (2018) A new classification scheme for periodontal and peri-implant diseases and conditions – Introduction and key changes from the 1999 classification. J Periodontol 89(S1):S1–S8. https://doi.org/10.1002/JPER.18-0157
Saunders MB, Gulabivala K, Holt R, Kahan RS (2000) Reliability of radiographic observations recorded on a proforma measured using inter- and intra-observer variation: a preliminary study. Int Endod J 33(3):272–278. https://doi.org/10.1046/j.1365-2591.1999.00304.x
McHugh M (2012) Interrater reliability: the kappa statistic. Biochem Med 22:276–281
Pepelassi EA, Diamanti-Kipioti A (1997) Selection of the most accurate method of conventional radiography for the assessment of periodontal osseous destruction. J Clin Periodontol 24(8):557–567. https://doi.org/10.1111/j.1600-051X.1997.tb00229.x
Acknowledgements
The authors would like to acknowledge the supports from the University of Texas Health Science Center at Houston School of Dentistry and the Taiwan National Yangming Chiaotung University.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the study. JC, MFC, NA, AG, YBL, BYW, and SA contributed to the design of the study. JC, HWM, SS, and KC have been involved in clinical data collection. MFC, CYH, and YRH dedicated to convolutional neural networks construction and application. JC and MFC worked on data interpretation and manuscript preparation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Committee for Protection of Human Subjects of the University of Texas Health Science Center at Houston (HSC-DB-19-0994).
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chang, J., Chang, MF., Angelov, N. et al. Application of deep machine learning for the radiographic diagnosis of periodontitis. Clin Oral Invest 26, 6629–6637 (2022). https://doi.org/10.1007/s00784-022-04617-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04617-4