Abstract
Objectives
The aim of this study was to develop a prognostic tool to estimate long-term tooth retention in periodontitis patients at the beginning of active periodontal therapy (APT).
Material and methods
Tooth-related factors (type, location, bone loss (BL), infrabony defects, furcation involvement (FI), abutment status), and patient-related factors (age, gender, smoking, diabetes, plaque control record) were investigated in patients who had completed APT 10 years before. Descriptive analysis was performed, and a generalized linear-mixed model-tree was used to identify predictors for the main outcome variable tooth loss. To evaluate goodness-of-fit, the area under the curve (AUC) was calculated using cross-validation. A bootstrap approach was used to robustly identify risk factors while avoiding overfitting.
Results
Only a small percentage of teeth was lost during 10 years of supportive periodontal therapy (SPT; 0.15/year/patient). The risk factors abutment function, diabetes, and the risk indicator BL, FI, and age (≤ 61 vs. > 61) were identified to predict tooth loss. The prediction model reached an AUC of 0.77.
Conclusion
This quantitative prognostic model supports data-driven decision-making while establishing a treatment plan in periodontitis patients. In light of this, the presented prognostic tool may be of supporting value.
Clinical relevance
In daily clinical practice, a quantitative prognostic tool may support dentists with data-based decision-making. However, it should be stressed that treatment planning is strongly associated with the patient’s wishes and adherence. The tool described here may support establishment of an individual treatment plan for periodontally compromised patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tooth retention remains a serious challenge in periodontally compromised patients. Periodontitis patients have a higher risk of tooth loss when compared to patients without periodontitis [1]. Progressing attachment- and tooth loss pose esthetic and functional limitations and may impair patient’s quality of life and self-confidence [2, 3]. The aim of periodontal therapy is to preserve teeth as long as possible.
There is evidence that some periodontal patients suffer from greater severity early in life or experience a higher risk for disease progression. These patients require specific and individualized treatment planning [4]. Although variables such as bone loss (BL), furcation involvement (FI), probing pocket depth (PPD), number of teeth lost (due to periodontitis), and patient-related factors such as smoking, age, and diabetes affect tooth retention [5,6,7,8], it still remains a challenge for the clinician to estimate treatment outcomes. Several attempts have been made to establish a prognostic model [9,10,11,12,13]. However, these models were not based on statistical methodology, and considered mostly tooth-related variables. Current scientific consensus shows that periodontitis represents a multifactorial disease influenced by many risk factors, which individually impinge upon disease progression and treatment management [5, 8, 9, 14,15,16,17]. In addition to tooth-related factors, patient-related parameters are strongly associated with tooth loss and need to be taken into account [2, 4].
To date, only a few data-driven prognostic models to estimate long-term tooth retention have been developed [18,19,20]. The aim of this explorative analysis is to develop a data-based prognostic tool that estimates risk factors contributing to tooth loss in periodontally compromised patients and can be applied in the beginning of the active periodontal therapy (APT).
Material and methods
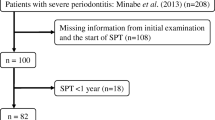
A long-term project was initiated in 2002 at the university hospital in Heidelberg to analyze tooth-retention in patients after comprehensive periodontal treatment. Detailed descriptions of the study protocol have been published [5, 6, 8, 17]. Thus, we only give a brief description of the methodologic aspects of the study.
Patients, who had received periodontal therapy (anti-infective therapy with subgingival debridement and periodontal surgery, if required) between 1992 and 1997 at the Section of Periodontology, Department of Conservative Dentistry under the lead of one periodontal specialist (PE), were re-examined 10 years ± 6 months after initiation of APT (T2) by an independent periodontal specialist (BP) [5, 6].
Radiographic examination
Every patient had obtained a complete set of periapical radiographs at the beginning of APT. A Schei-ruler was used to evaluate interproximal bone loss [21]. Teeth were assigned to one of five increments of BL (≤ 20%; 21% to < 40%; 40% to < 60%; 60% to < 80%; ≥ 80%; Pretzl et al., 2008) according to BL at the most affected site. These thresholds correspond roughly to the staging of periodontitis in the current classification with BL ≤ 20% representing stage I and BL 21% to < 40% approximately stage II. If a tooth experienced vertical bone loss, it was assigned to one of three groups: shallow (< 2 mm), moderate (2.5–4 mm), or deep (≥ 4 mm).
Evaluation of patients’ charts
To assess tooth loss, patients’ charts were analyzed, and tooth number at baseline (T0), first SPT examination (T1), and 10-year re-evaluation (T2) was compared.
Additionally, the following variables were retrieved from patient’s medical history at baseline (T0): age, smoking status (current/former (quit smoking at least 5 years ago)/never smoker) [22], and self-reported diabetes (yes/no).
PCR-value [23] at the beginning of supportive periodontal therapy (SPT, T1) was included in this analysis.
Further tooth-related parameters were retrieved from patients’ charts (T0): localization (maxilla/mandible), tooth type (anterior/pre-molar/molar), FI (single-rooted tooth/multi-rooted tooth with/without furcation involvement), and abutment tooth (none/abutment tooth for fixed/removable prosthodontic construction).
Supportive periodontal therapy
During SPT, a standardized protocol including oral hygiene instructions and supragingival plaque removal was performed. Dental and periodontal status was obtained once to twice a year. If PPDs were 4 mm with BOP or ≥ 5 mm, subgingival scaling was performed [24]. If subgingival debridement of more than five teeth was necessary, complete re-treatment was recommended. However, only a limited number of patients received re-treatment during SPT, which complied with a non-surgical approach. Since October 1999 patients have been assigned an individual SPT interval according to the periodontal risk assessment (PRA) [5, 22].
Statistical analysis
Descriptive methods were used to summarize characteristics on patient- and tooth-level. Continuous variables were documented using mean and standard deviation, categorical variables using absolute and relative frequencies.
Third molars were not included in the analysis.
Data entry was performed using Microsoft Excel© for macOS (Version 16.29.1; Microsoft Corporation, Redmond, WA, USA). One investigator (SR-W) entered all data into one file. An independent statistician (DK) calculated the descriptive analysis and modeled the generalized linear-mixed model-tree using R version 4.0.2 [25].
Development of prognostic model
A generalized linear mixed model tree was used to develop a prognostic model for tooth loss on the basis of periodontally treated patients 10 years after APT. The generalized linear mixed model tree performs automated variable selection and allows considering the nested structure of tooth within a patient [26]. The independent variables taken into consideration were age (years), gender (female/male), PCR, smoking (active/former/never), diabetes (yes/no) on patient-level, as well as jaw (maxilla/mandible), tooth type (anterior/pre-molar/molar), FI (single-rooted/multi-rooted without/with furcation involvement), interproximal BL (≤ 20%/21% to 40%/41% to 60%/61% to 80%/ > 80%), infrabony defect (shallow/moderate/deep), and abutment tooth (no/fixed/removable dentures) on tooth-level. Because of the low counts in interproximal bone loss categories 4 and 5, these groups were merged (interproximal bone loss > 60%).
The present study evaluates primary tooth-related risk factors for tooth loss. For all analyses, the basic level tooth was clustered into the upper level patient; the patient was considered as random effect.
In terms of risk factor selection, 200 bootstrap samples of the data were used to achieve robust variable selection results. Bootstrapping is done on patient level meaning that patients are randomly drawn with replacement such that the bootstrap data includes the same number of patients as the original data set. For each bootstrap sample, a generalized linear mixed model tree is fitted, and the occurrence of the selected variables was counted. Variables on tooth-level selected by more than 50% and on patient-level by more than 25% of the bootstrap-based models were taken into consideration for the selection within the final model, because bootstrap samples are based on patients, which limit the variability in patient level characteristics. To build the final tree, the model was fitted on all samples using the variable set selected by applying the bootstrap approach.
After the set of variables was fixed, the prognostic model was internally validated in order to avoid overfitting. Ten-fold cross-validation (CV) was used to estimate the area under the receiver operating characteristic curve (AUC), sensitivity, and specificity for evaluating the model fit. Cross-validation means splitting the data in 10 parts, 9 splits are used for training the model, and each split is used for testing the model once. Cross-validation sets were split by patient, which means all teeth of a patient were included in the same fold to keep training and test set independent. Consequently, CV folds included the same number of patients, but may not include the same number of teeth, as the number of teeth differs between patients. The mean value of AUC, sensitivity, and specificity was calculated over the cross-validation sets. They were reported together with 95% Wilson confidence intervals (CI) based on the number of independent patients, which reflects a conservative approach. The generalized linear mixed model tree generates a probability for tooth loss after 10 years for each tooth individually.
Results
Patient- and tooth-related characteristics of the sample upon which the model is based can be found in Tables 1 and 2.
In the sample 61.8% of patients were female, average age at T0 was 46.7 years (standard deviation (SD) = 10.26) and 30.0% were active, 24.5% former, and 45.5% non-smokers. Nine participants suffered from diabetes mellitus (8.2%). The average PCR at T1 was 31.3% (SD = 17.39).
At T0 2556 teeth were present. Of these 1341 teeth were in the mandible, 1215 in the maxilla, 733 teeth were pre-molars, 616 molars, and 1207 anteriors. More than two thirds were single-rooted (1770) and 431 teeth exhibited a FI. The majority of teeth had an interproximal BL of 21–40% (1078), while 160 teeth showed an interproximal BL between 61 and 80%, and 59 the most severe BL (> 80%). A total of 232 teeth were abutment teeth used for fixed (10.3%) and 67 for removable prosthetic reconstructions (2.9%). One hundred sixty-six teeth were lost during ten years of SPT (0.15/year/patient). Table 2 shows the distribution of tooth loss.
Prognostic tree model
For the final tree model, data of 110 patients with 2528 teeth were used corresponding to a complete case analysis. The final tree model, where variable selection was automatically performed based on a bootstrap approach including patient- and tooth-related variables: BL, FI, abutment tooth, age (≤ 61 versus > 61), and diabetes (Table 3 and Fig. 1).
Based on a statistical model, the tree selected the variable with the greatest impact on tooth loss in the first step. In the present analysis, periodontal BL over 60% was marked as first cut-off. Teeth in this category are at risk of being lost in 22.3%. In further steps, additional variables were chosen accordingly. In the end, teeth were split into eight categories/groups (Table 3). Teeth with a periodontal BL 41–60% and being a multi-rooted tooth with FI were lost in 16.8%, whereas teeth with a periodontal BL < 40% and being multi-rooted with FI were lost in 6.3%. In category 5 and 4 age seems to have a great impact. While teeth with a periodontal BL ≤ 60% and being single-rooted or multi-rooted without FI and have an abutment function for fixed or removable dentures were lost in only 5.0% of the cases in patients ≤ 61 years of age, patients over the age bracket of 61 years in the same category were at risk of losing these teeth in 50.0%. Teeth with an initial BL of 41–60% and being single-rooted or multi-rooted without FI and have no abutment function were at risk of being lost in 5.7%. When teeth experience a periodontal BL of < 40% and being single-rooted or multi-rooted without FI and have no abutment function and the patient suffered from diabetes, teeth had a risk of being lost in 5.7%. However, when the patient did not suffer from diabetes, teeth were only lost in 2.2% of the cases. Note that a higher category number does not correspond to higher tooth loss rate. Rates for tooth loss within each category are given in Table 3.
To evaluate the performance of the fitted model (internal validation) CV-folds were used. They reached a mean AUC-value of 0.77 (95% CI [0.68; 0.84]), a sensitivity of 0.73 (95% CI [0.64; 0.80]), and a specificity of 0.79 (95% CI [0.70; 0.86]). These values can be considered as acceptable model performance. In this setting, a higher specificity is desirable corresponding to the probability of teeth correctly classified as “no tooth loss.” The naïve model performance, i.e., evaluation measures calculated on the trainings set, reached an AUC-value of 0.95, a sensitivity of 0.80, and a specificity of 0.93. It is important to note that these naïve measures overfit the model performance and might not be reproducible in an external cohort.
Discussion
Treatment of periodontally compromised patients remains a challenge. Rather than the therapy itself, treatment planning represents a critical and important part.
The presented prognostic tool aims to support practitioners’ decision-making, while establishing a treatment plan in the beginning of periodontal therapy. To evaluate individual tooth prognosis, factors on different levels have to be taken into account: tooth, patient, dentist, and environmental level [4,5,6, 17, 27,28,29,30,31,32]. The final tree model evaluates tooth- and patient-related variables and estimates the risk for tooth loss based on a statistical model. Abutment teeth (fixed or removable) with a periodontal BL ≤ 60%, being single-rooted or multi-rooted without FI in patients > 61 years of age are considered to be at highest risk for tooth loss (50.0%). In comparison, the risk of tooth loss in teeth with the same criteria, but under the age of 61, is estimated to be ten times less (5.0%) (Table 3). Thus, increasing age plays an important role in our evaluation. This finding corresponds with previous findings from other surveys, where age was considered a risk indicator for periodontal disease progression [16, 33]. An accumulation of plaque, biological changes, and consequently a reduction of tissue regeneration and disease regression may lead to an impaired wound-healing ability with increasing age [7, 34,35,36,37].
In the past, surveys presented prognostic systems to evaluate the risk for tooth loss [9,10,11,12,13]. However, most of these publications did not introduce an evaluated data-driven prognostic model to avoid overfitting. A recent publication introduced a nomogram to predict periodontal tooth loss based on the staging and grading system [38], but tooth loss was modeled on patient-level only.
Hirschfeld and Wasserman categorized teeth into “favorable and questionable” prognoses—based on tooth-related factors such as FI, PPD, alveolar BL, and degrees of mobility [9]. Checchi et al. (2002) distinguished “good/questionable/or hopeless” teeth based on tooth-related factors [10]. However, the assignment of prognosis in these two studies relies on p values, without focusing on model performance. Both studies conclude the highest risk for loss to be in teeth with severe periodontal BL (> 75%). Meanwhile, several studies have shown that teeth with such BL can be retained over a long period (10 years and more), implicating that both of these systems do not seem suitable for treatment planning [5, 17, 39,40,41,42]. The present prognostic tool appears to show a higher degree of differentiation, since teeth with advanced BL of 60% seem to have a low risk of tooth loss (23%; Table 3, Fig. 1), and teeth with BL < 60% without FI, used as abutment teeth in patients aged > 61, have a higher risk of being lost (50%, group 4, Table 3, Fig. 1). Additionally, patient-related factors are disregarded in the two aforementioned studies. All variables have to be interpreted within the patient, since teeth belong to a person, whose characteristics or behavior influence the outcome as well [17].
A report by Kwok and Caton (2007) considered general (compliance, plaque accumulation, smoking, diabetes, and others) and local factors (PPD, attachment loss, anatomic plaque-retentive factors, trauma from occlusion and habits, mobility) based on literature evidence. No statistical model was calculated based on clinical data, and the relative weight of each variable was not presented, which results in a prognostic proposal with uncertain recommendations [11]. A direct comparison between their narrative review and our statistical data-driven model-tree does therefore not seem feasible.
Nibali et al. proposed a different prognostic system [13]: teeth were assigned either a good, fair, questionable, or unfavorable prognosis based on a periodontal risk assessment (PRA [22]) and periodontal risk calculator (PRC [43]). Variables (such as PPD, FI, mobility, BL, periapical pathology, restorability) were taken into account from previous literature. Although their statistical methodology considers the clustered structure of the data, the prognostic system was based on risk assessment in patients after APT. In contrast to this, the prognostic tool described in this study attempts to assess the risk for tooth loss in periodontally compromised patients at the beginning of treatment in order to support treatment planning. Furthermore, the two periodontal risk assessment methods (PRA and PRC) do not seem to have a high level of agreement in terms of patient’s individual risk for disease progression [44].
Mc Gowan et al. proposed an evidence-based prognostic model in their review using previously published periodontal prognosis models [12]. Variables included tooth-level (BL/age-ratio, PPD, extent of FI, infrabony defect, compromising anatomical factors, extent of mobility) and patient-level (smoking, poorly controlled diabetes, BOP). However, they present a comparison of models and do not provide an original tool.
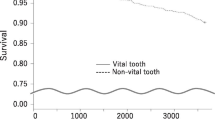
Only a few groups have developed a data-based prognostic model to estimate long-term tooth retention [18,19,20]. Faggion et al. (2017) developed a prognostic model to estimate survival rates of teeth in periodontally compromised patients over an observation period of 11.8 years. In agreement with our findings, variables such as diabetes and BL (additionally tooth mobility and root type) were identified as influential predictors for tooth loss. Their prognostic model showed that multi-rooted, vital teeth in non-diabetic patients with a periodontal bone loss of 40% have a probability of 80–89% tooth survival. In contrast patients suffering from diabetes in the same group showed a 50–59% probability of tooth survival. These results are comparable to ours (Table 3). Diabetes patients with single-rooted or multi-rooted teeth without furcation involvement and no abutment function with a periodontal bone loss ≤ 40% showed a 5.7% rate of being lost. On the other hand, the rate in patients without diabetes with the same criteria was calculated at 2.2% (Fig. 2). However, variables in Faggion et al. (2017) were identified using a backward-selection procedure based on p values. P values depend on various circumstances, i.e., higher sample sizes lead to smaller p-values (even for variables which may not help to predict the outcome). In contrast, our statistical approach relies on automatically selecting risk factors and cut-offs.
In contrast to our tool which is applicable for all teeth, Miller et al. proposed a prognostic model for molars [19]. The selection of variables influencing the score (molar type, smoking, FI, PPD, mobility, and age) was not based on statistical methods but quantitatively. This subjective scoring may lead to poor model performance and bias. In comparison, our analysis combines variable selection and outcome prediction and allows for an impartial objective data selection.
The analysis of Martinez-Canut et al. (2018) consists of two separate models (molars and non-molars) analyzing one factor at a time as opposed to our explorative analysis, where all teeth are included simultaneously in one model. Separating teeth in different models leads to lower sample sizes, which may result in less accurate predictions. Additionally, multiple factors interact in one patient and should therefore be considered together in a data-driven tool, as well. In line with the present study, Martinez-Canut et al. calculated discrimination measurements such as AUC, sensitivity, and specificity. In their study, AUC amounts to 0.93–0.97 (molars/non-molars); with a sensitivity of 39%/43%, and a specificity of 98%/99%. The introduced prognostic tool reaches an AUC value of 0.77, a sensitivity of 73%, and a specificity of 79%. The difference may be explained by the fact that the presented analysis uses cross-validation for internal validation. These statistical methods are crucial to avoid overfitting and overoptimistic results but are occasionally used in the evaluation of already existing prediction models for tooth loss.
In Ancient Greece “prognosis” was described by Hippocrates as “foreseeing and foretelling, by the side of the sick, the present, the past, and the future” [45]. The appreciation of past and present helps to better understand the future. This concept still applies today. Treatment outcome is strongly influenced by patient’s history as well as adherence. Studies have reported the significant impact of compliance on tooth loss, emphasizing that patients, who do not adhere to treatment regimen, loose significantly more teeth than others [17, 20, 29, 31]. Unfortunately, factors such as patient adherence and dentist’s skills cannot be predicted or measured in advance of periodontal therapy. Theoretically, patient adherence could be taken into account indirectly using PCR trying to assess a patient’s oral hygiene effectiveness. Although PCR at T1 was recorded, the final tree model did not take this variable into account, since the plaque formation rate can vary widely between patients. Nonetheless, we know from numerous studies that patient adherence and dentists’ preferences play a decisive role in long-term tooth retention. Thus, they have to be taken into account apart from the tool. The same applies to the variable “smoking.” The reason why smoking was not considered may be the small difference between the number of teeth lost in smokers vs. non-smokers and the small sample size, which may have weakened the effect of smoking. Additionally, in many populations as well as in our sample, smoking prevalence decreased due to the increasing awareness campaign and frequent smoking cessation during SPT [46].
Prognosis at start of therapy is only the first step to guide treatment decisions. Prognosis means forecasting the future with the knowledge of the past and the present. This forecast will be accurate as long as past and present conditions stay the same. However, people change to the better (quit smoking) or the worse (develop diabetes or depression). Thus, prognosis at start of treatment will never 100% accurately forecast the course of periodontal disease including tooth loss. In the course of SPT the dentist will try to influence the patient to the better or to adjust treatment to ameliorate the worse. However, the result of this process cannot be exactly predicted at baseline even not by best prognosis tool.
Perspective
The presented prognostic tool was cross-validated to avoid overfitting. Whether this prognostic model is appropriate to evaluate the risk for tooth loss in other groups has yet to be verified. To review the accuracy and the general applicability, an external validation with a different cohort is already planned.
The setting of the study may represent a limitation. Practice-based studies report lower tooth loss rates [9, 15, 47] compared with university-based studies [7, 18, 41, 48]. Different patients treated in these settings may explain the difference. To verify whether the presented tool is applicable in a practice-based setting, another validation process should be conducted.
Limitations
The results have to be interpreted with caution. There might be other patient- or tooth-related characteristics that influence tooth survival not observed in the present study.
The tool presented here relies on mathematical models allocating relative weight to the presented variables. It does not differentiate in different categories (good/questionable/hopeless) or scores, because such cutoffs result in a loss of information and are difficult to choose. Therefore, the probability of tooth loss rather than a category is reported.
Conclusions
In clinical practice, a quantitative prognostic tool may support dentists with data-based decision-making and enable an individual treatment plan for periodontally compromised patients. However, it should be stressed that treatment planning is strongly associated with patient’s wishes and adherence. In light of this, the presented prognostic tool may be of supporting value.
References
Pullen F, Folberth R, Ruhmann C, Eickholz P (2013) Tooth extractions in general and due to periodontal reasons in three dental practices: a case-control study. Quintessence Int 44:327–338. https://doi.org/10.3290/j.qi.a29155
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol 89(Suppl 1):S173-s182. https://doi.org/10.1002/jper.17-0721
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreno CC, Kearns C, Benzian H, Allison P, Watt RG (2019) Oral diseases: a global public health challenge. Lancet 394:249–260. https://doi.org/10.1016/s0140-6736(19)31146-8
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodont 89(Suppl 1):S159-s172. https://doi.org/10.1002/jper.18-0006
Eickholz P, Kaltschmitt J, Berbig J, Reitmeir P, Pretzl B (2008) Tooth loss after active periodontal therapy. 1: patient-related factors for risk, prognosis, and quality of outcome. J Clin Periodontol 35:165–174. https://doi.org/10.1111/j.1600-051X.2007.01184.x
Pretzl B, Kaltschmitt J, Kim TS, Reitmeir P, Eickholz P (2008) Tooth loss after active periodontal therapy. 2: tooth-related factors. J Clin Periodontol 35:175–182. https://doi.org/10.1111/j.1600-051X.2007.01182.x
Graetz C, Plaumann A, Schlattmann P, Kahl M, Springer C, Salzer S, Gomer K, Dorfer C, Schwendicke F (2017) Long-term tooth retention in chronic periodontitis - results after 18 years of a conservative periodontal treatment regimen in a university setting. J Clin Periodontol 44:169–177. https://doi.org/10.1111/jcpe.12680
Pretzl B, El Sayed S, Weber D, Eickholz P, Baumer A (2018) Tooth loss in periodontally compromised patients: results 20 years after active periodontal therapy. J Clin Periodontol 45:1356–1364. https://doi.org/10.1111/jcpe.13010
Hirschfeld L, Wasserman B (1978) A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol 49:225–237. https://doi.org/10.1902/jop.1978.49.5.225
Checchi L, Montevecchi M, Gatto MR, Trombelli L (2002) Retrospective study of tooth loss in 92 treated periodontal patients. J Clin Periodontol 29:651–656
Kwok V, Caton J (2007) Prognosis revisited: a system for assigning periodontal prognosis. J Periodontol 78:2063–2071. https://doi.org/10.1902/jop.2007.070210
McGowan T, McGowan K, Ivanovski S (2017) A novel evidence-based periodontal prognosis model. J Evid Based Dent Pract 17:350–360. https://doi.org/10.1016/j.jebdp.2017.05.006
Nibali L, Sun C, Akcali A, Meng X, Tu YK, Donos N (2017) A retrospective study on periodontal disease progression in private practice. J Clin Periodontol 44:290–297. https://doi.org/10.1111/jcpe.12653
McFall WT Jr (1982) Tooth loss in 100 treated patients with periodontal disease A long-term study. J Periodontol 53:539–549. https://doi.org/10.1902/jop.1982.53.9.539
McGuire MK, Nunn ME (1996) Prognosis versus actual outcome. II. The effectiveness of clinical parameters in developing an accurate prognosis. J Periodontol 67:658–665. https://doi.org/10.1902/jop.1996.67.7.658
Billings M, Holtfreter B, Papapanou PN, Mitnik GL, Kocher T, Dye BA (2018) Age-dependent distribution of periodontitis in two countries: findings from NHANES 2009 to 2014 and SHIP-TREND 2008 to 2012. J Periodontol 89(Suppl 1):S140-s158. https://doi.org/10.1002/jper.17-0670
Rahim-Wöstefeld S, El Sayed N, Weber D, Kaltschmitt J, Bäumer A, El-Sayed S, Eickholz P, Pretzl B (2020) Tooth-related factors for tooth loss 20 years after active periodontal therapy–a partially prospective study. J Clin Periodontol 47:1227–1236. https://doi.org/10.1111/jcpe.13348
Faggion CM Jr, Petersilka G, Lange DE, Gerss J, Flemmig TF (2007) Prognostic model for tooth survival in patients treated for periodontitis. J Clin Periodontol 34:226–231. https://doi.org/10.1111/j.1600-051X.2006.01045.x
Miller PD Jr, McEntire ML, Marlow NM, Gellin RG (2014) An evidenced-based scoring index to determine the periodontal prognosis on molars. J Periodontol 85:214–225. https://doi.org/10.1902/jop.2013.120675
Martinez-Canut P, Alcaraz J, Alcaraz J Jr, Alvarez-Novoa P, Alvarez-Novoa C, Marcos A, Noguerol B, Noguerol F, Zabalegui I (2018) Introduction of a prediction model to assigning periodontal prognosis based on survival time. J Clin Periodontol 45:46–55. https://doi.org/10.1111/jcpe.12810
Schei O, Waerhaug J, Lovdal A, Arno A (1959) Alveolar bone loss as related to oral hygiene and age. J Periodontol 30:7–16. https://doi.org/10.1902/jop.1959.30.1.7
Lang NP, Tonetti MS (2003) Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev Dent 1:7–16
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38. https://doi.org/10.1902/jop.1972.43.1.38
Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D (2002) A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol 29(Suppl 3):92–102. https://doi.org/10.1034/j.1600-051x.29.s3.5.x (discussion 160-2)
R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Hajjem A, Bellavance F, Larocque D (2011) Mixed effects regression trees for clustered data. Stat Probab Lett 81:451–459. https://doi.org/10.1016/j.spl.2010.12.003
Matuliene G, Studer R, Lang NP, Schmidlin K, Pjetursson BE, Salvi GE, Bragger U, Zwahlen M (2010) Significance of periodontal risk assessment in the recurrence of periodontitis and tooth loss. J Clin Periodontol 37:191–199. https://doi.org/10.1111/j.1600-051X.2009.01508.x
Bäumer A, El Sayed N, Kim TS, Reitmeir P, Eickholz P, Pretzl B (2011) Patient-related risk factors for tooth loss in aggressive periodontitis after active periodontal therapy. J Clin Periodontol 38:347–354. https://doi.org/10.1111/j.1600-051X.2011.01698.x
Lee CT, Huang HY, Sun TC, Karimbux N (2015) Impact of patient compliance on tooth loss during supportive periodontal therapy: a systematic review and meta-analysis. J Dent Res 94:777–786. https://doi.org/10.1177/0022034515578910
Schwendicke F, Dorfer CE, Meier T (2018) Global smoking-attributable burden of periodontal disease in 186 countries in the year 2015. J Clin Periodontol 45:2–14. https://doi.org/10.1111/jcpe.12823
Helal O, Gostemeyer G, Krois J, Fawzy El Sayed K, Graetz C, Schwendicke F (2019) Predictors for tooth loss in periodontitis patients: Systematic review and meta-analysis. J Clin Periodontol 46:699–712. https://doi.org/10.1111/jcpe.13118
Bäumer A, Weber D, Staufer S, Pretzl B, Korner G, Wang Y (2020) Tooth loss in aggressive periodontitis: results 25 years after active periodontal therapy in a private practice. J Clin Periodontol 47:223–232. https://doi.org/10.1111/jcpe.13225
Renvert S, Persson RE, Persson GR (2013) Tooth loss and periodontitis in older individuals: results from the Swedish national study on aging and care. J Periodontol 84:1134–1144. https://doi.org/10.1902/jop.2012.120378
Benatti BB, Neto JB, Casati MZ, Sallum EA, Sallum AW, Nociti FH Jr (2006) Periodontal healing may be affected by aging: a histologic study in rats. J Periodontal Res 41:329–333. https://doi.org/10.1111/j.1600-0765.2006.00872.x
Schätzle M, Faddy MJ, Cullinan MP, Seymour GJ, Lang NP, Bürgin W, Anerud A, Boysen H, Löe H (2009) The clinical course of chronic periodontitis: V. Predictive factors in periodontal disease. J Clin Periodontol 36:365–371. https://doi.org/10.1111/j.1600-051X.2009.01391.x
Caceres M, Oyarzun A, Smith PC (2014) Defective wound-healing in aging gingival tissue. J Dent Res 93:691–697. https://doi.org/10.1177/0022034514533126
Eickholz P, Hausmann E (1998) Evidence for healing of interproximal intrabony defects after conventional and regenerative therapy: digital radiography and clinical measurements. J Periodontal Res 33:156–165. https://doi.org/10.1111/j.1600-0765.1998.tb02306.x
Ravidà A, Troiano G, Qazi M, Saleh M, Russo L, Greenwell H, Giannobile W, Wang H-L (2020) Development of a nomogram for the prediction of periodontal tooth loss using the staging and grading system: a long-term cohort study. J Clin Periodontol. https://doi.org/10.1111/jcpe.13362
Muzzi L, Nieri M, Cattabriga M, Rotundo R, Cairo F, Pini Prato GP (2006) The potential prognostic value of some periodontal factors for tooth loss: a retrospective multilevel analysis on periodontal patients treated and maintained over 10 years. J Periodontol 77:2084–2089. https://doi.org/10.1902/jop.2006.050227
Pretzl B, Kim TS, Steinbrenner H, Dorfer C, Himmer K, Eickholz P (2009) Guided tissue regeneration with bioabsorbable barriers III 10-year results in infrabony defects. J Clin Periodontol 36:349–356. https://doi.org/10.1111/j.1600-051X.2009.01378.x
Dannewitz B, Zeidler A, Husing J, Saure D, Pfefferle T, Eickholz P, Pretzl B (2016) Loss of molars in periodontally treated patients: results 10 years and more after active periodontal therapy. J Clin Periodontol 43:53–62. https://doi.org/10.1111/jcpe.12488
Graetz C, Baumer A, Eickholz P, Kocher T, Petsos H, Pretzl B, Schwendicke F, Holtfreter B (2020) Long-term tooth retention in periodontitis patients in four German university centres. J Dent 94:103307. https://doi.org/10.1016/j.jdent.2020.103307
Page RC, Krall EA, Martin J, Mancl L, Garcia RI (2002) Validity and accuracy of a risk calculator in predicting periodontal disease. J Am Dent Assoc 133:569–76. https://doi.org/10.14219/jada.archive.2002.0232
Petsos H, Arendt S, Eickholz P, Nickles K, Dannewitz B (2020) Comparison of two different periodontal risk assessment methods with regard to their agreement: periodontal risk assessment versus periodontal risk calculator. J Clin Periodontol 47:921–932. https://doi.org/10.1111/jcpe.13327
Thomas JM, Cooney LM Jr, Fried TR (2019) Prognosis reconsidered in light of ancient insights—from hippocrates to modern medicine. JAMA Intern Med 179:820–823. https://doi.org/10.1001/jamainternmed.2019.0302
Zeiher J, Finger JD, Kuntz B, Hoebel J, Lampert T, Starker A (2018) Trends in smoking among adults in Germany : evidence from seven population-based health surveys from 1991–2015. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 61:1365–1376. https://doi.org/10.1007/s00103-018-2817-9
Chambrone LA, Chambrone L (2006) Tooth loss in well-maintained patients with chronic periodontitis during long-term supportive therapy in Brazil. J Clin Periodontol 33:759–764. https://doi.org/10.1111/j.1600-051X.2006.00972.x
Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Bragger U, Zwahlen M, Lang NP (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35:685–695. https://doi.org/10.1111/j.1600-051X.2008.01245.x
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was self-funded by the authors and their institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Sonja Rahim-Wöstefeld declares that she has no conflict of interest. Dorothea Kronsteiner declares that she has no conflict of interest. Shirin ElSayed declares that she has no conflict of interest. Nihad ElSayed declares that she has no conflict of interest. Peter Eickholz reports fees, grants, and non-financial support outside the submitted work. Bernadette Pretzl declares that she has no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rahim-Wöstefeld, S., Kronsteiner, D., ElSayed, S. et al. Development of a prognostic tool: based on risk factors for tooth loss after active periodontal therapy. Clin Oral Invest 26, 813–822 (2022). https://doi.org/10.1007/s00784-021-04060-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04060-x