Abstract
Objectives
Analyze the association between higher added sugar exposure and periodontal disease in adolescents (18–19 years old).
Materials and methods
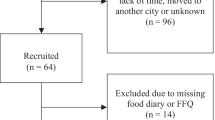
This was a cross-sectional study nested to RPS Cohorts Consortium, São Luís, Brazil (n = 2515). The exposure was percentage of daily calories from added sugar (≥ 10%), estimated from a quantitative food frequency. The outcome was periodontal disease estimated by the number of teeth affected by bleeding on probing, periodontal probing depth ≥ 4 mm, and clinical attachment level ≥ 4 mm at the same site. A theoretical model was depicted in a directed acyclic graph to identify the minimal sufficient adjustment set: household income, adolescent’s educational level, sex, alcohol use, and smoking. Periodontal disease was categorized into < 2 teeth affected, 2 to 3 teeth affected, and ≥ 4 teeth affected to estimate prevalence ratios (PR) by multinomial logistic regression. To test for consistency, means ratio (MR) were estimated using zero-inflated Poisson.
Results
High sugar intake was associated with ≥ 4 teeth affected by periodontal disease (PR = 1.42; 95% confidence interval (CI) = 1.03–1.94; p = 0.030); consistency Poisson analysis reinforced these results (MR = 1.15; 95% CI = 1.03–1.29; p = 0.011).
Conclusion
High level of added sugar intake was associated with greater extent of periodontal disease in adolescents.
Clinical relevance
High sugar intake was associated with periodontal disease in adolescents, supporting the integrated hypothesis of dental caries and periodontal disease and giving impetus to future clinical investigation on the effect of restriction of added sugar consumption in periodontal parameters, which potentially may change traditional treatment protocols of periodontal disease.

Similar content being viewed by others
References
World Health Organization (2014) Global status report on noncommunicable diseases. World Health Organization
World Health Organization (2015) Guideline: sugars intake for adults and children. World Health Organization, Geneva
Te Morenga L, Mallard S, Mann J (2012) Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 346:e7492. https://doi.org/10.1136/bmj.e7492
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (2014) Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol 2:634–647. https://doi.org/10.1016/S2213-8587(14)70102-0
Sheiham A, James WPT (2015) Diet and dental caries: the pivotal role of free sugars reemphasized. J Dent Res 94:1341–1347. https://doi.org/10.1177/0022034515590377
Lula ECO, Ribeiro CCC, Hugo FN et al (2014) Added sugars and periodontal disease in young adults: an analysis of NHANES III data. Am J Clin Nutr 100:1182–1187. https://doi.org/10.3945/ajcn.114.089656
Fann JC-Y, Lai H, Chiu SY-H et al (2016) A population-based study on the association between the intake of soft drinks and periodontal disease in Taiwanese adults aged 35-44 years (KCIS no. 33). Public Health Nutr 19:1471–1478. https://doi.org/10.1017/S1368980015002608
Song I-S, Han K, Ko Y et al (2016) Associations between the consumption of carbonated beverages and periodontal disease: The 2008-2010 Korea national health and nutrition examination survey. Medicine (Baltimore) 95:e4253. https://doi.org/10.1097/MD.0000000000004253
Nyvad B, Takahashi N (2020) Integrated hypothesis of dental caries and periodontal diseases. J Oral Microbiol 12:1710953. https://doi.org/10.1080/20002297.2019.1710953
Carmo CDS, Ribeiro MRC, Teixeira JXP et al (2018) Added sugar consumption and chronic oral disease burden among adolescents in Brazil. J Dent Res 97:508–514. https://doi.org/10.1177/0022034517745326
Shrier I, Platt RW (2008) Reducing bias through directed acyclic graphs. BMC Med Res Methodol 8:70. https://doi.org/10.1186/1471-2288-8-70
Schisterman EF, Cole SR, Platt RW (2009) Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 20:488–495. https://doi.org/10.1097/EDE.0b013e3181a819a1
Rodrigues LDS, Batista RFL, Simões VMF et al (2018) Does height catch-up in schoolchildren have an effect on bone mass in adolescents? Analysis in a Brazilian birth cohort. J Pediatr 95:607–613. https://doi.org/10.1016/j.jped.2018.05.015
Moretti-Pires RO, Corradi-Webster CM (2011) Adaptation and validation of the Alcohol Use Disorders Identification Test (AUDIT) for a river population in the Brazilian Amazon. Cad Saude Publica 27:497–509. https://doi.org/10.1590/s0102-311x2011000300010
Ministry of Health (2012) SB Brazil 2010: National research on oral health. Main results, Ministry of Health, Brasilia
Schneider BC, Motta JVDS, Muniz LC et al (2016) Desenho de um questionário de frequência alimentar digital autoaplicado para avaliar o consumo alimentar de adolescentes e adultos jovens: Coortes de nascimentos de Pelotas, Rio Grande do Sul. Rev Bras Epidemiol 19:419–432. https://doi.org/10.1590/1980-5497201600020017
da Sousa R, S, Bragança MLBM, de Oliveira BR et al (2020) Association between the degree of processing of consumed foods and sleep quality in adolescents. Nutrients 12:462. https://doi.org/10.3390/nu12020462
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
American Academy of Periodontology (2001) Glossary of periodontal terms. https://members.perio.org/libraries/glossary?_ga = 2.171418080.19602079.1549170589-926308261.1548130467&ssopc = 1. Accessed 1 Dec 2018
Reisdorfer E, Büchele F, Pires ROM, Boing AF (2012) Prevalence and associated factors with alcohol use disorders among adults: a population-based study in southern Brazil. Rev Bras Epidemiol 15:582–594. https://doi.org/10.1590/s1415-790x2012000300012
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i–xii, 1–253. https://doi.org/10.1016/j.bbi.2016.02.019
Lin D, Qi Y, Huang C et al (2018) Associations of lipid parameters with insulin resistance and diabetes: a population-based study. Clin Nutr 37:1423–1429. https://doi.org/10.1016/j.clnu.2017.06.018
Olson K, Hendricks B (2012) Murdock DK (2012) The triglyceride to HDL ratio and its relationship to insulin resistance in pre- and postpubertal children: observation from the wausau SCHOOL project. Cholesterol. https://doi.org/10.1155/2012/794252
World Health Organization (2009) Global health risks: mortality and burden of disease attributable to selected major risks. http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf. Accessed 9 Nov 2019
Singh GM, Micha R, Khatibzadeh S et al (2015) Estimated global, regional, and national disease burdens related to sugar-sweetened beverage consumption in 2010. Circulation 132:639–666. https://doi.org/10.1161/CIRCULATIONAHA.114.010636
Moynihan PJ, Kelly SAM (2014) Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res 93:8–18. https://doi.org/10.1177/0022034513508954
Botero JE, Rösing CK, Duque A et al (2015) Periodontal disease in children and adolescents of Latin America. Periodontol 2000(67):34–57. https://doi.org/10.1111/prd.12072
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis : framework and proposal of a new classification and case definition. 89:159–172. https://doi.org/10.1002/JPER.18-0006
Aragno M, Mastrocola R (2017) Dietary sugars and endogenous formation of advanced glycation endproducts: emerging mechanisms of disease. Nutrients 9:1–16. https://doi.org/10.3390/nu9040385
Johnson RK, Appel LJ, Brands M et al (2009) Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 120:1011–1020. https://doi.org/10.1161/CIRCULATIONAHA.109.192627
Nepomuceno R, Pigossi SC, Finoti LS et al (2017) Serum lipid levels in patients with periodontal disease: a meta-analysis and meta-regression. J Clin Periodontol 44:1192–1207. https://doi.org/10.1111/jcpe.12792
Daudt LD, Musskopf ML, Mendez M et al (2018) Association between metabolic syndrome and periodontitis: a systematic review and meta-analysis. Braz Oral Res 32:1–15. https://doi.org/10.1210/jc.2012-3552
Nascimento GG, Leite FRM, Vestergaard P et al (2018) Does diabetes increase the risk of periodontitis? A systematic review and meta-regression analysis of longitudinal prospective studies. Acta Diabetol 55:653–667. https://doi.org/10.1007/s00592-018-1120-4
Chapple ILC, Bouchard P, Cagetti MG et al (2017) Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 44(Suppl 1):S39–S51. https://doi.org/10.1111/jcpe.12685
Sanz M, Beighton D, Curtis MA et al (2017) Role of microbial biofilms in the maintenance of oral health and in the development of dental caries and periodontal diseases. Consensus report of group 1 of the Joint EFP/ORCA workshop on the boundaries between caries and periodontal disease. J Clin Periodontol 44(Suppl 1):S5–S11. https://doi.org/10.1111/jcpe.12682
Baumgartner S, Imfeld T, Schicht O et al (2009) The impact of the stone age diet on gingival conditions in the absence of oral hygiene. J Periodontol 80:759–768. https://doi.org/10.1902/jop.2009.080376
Milne DB, Nielsen FH (2000) The interaction between dietary fructose and magnesium adversely affects macromineral homeostasis in men. J Am Coll Nutr 19:31–37. https://doi.org/10.1080/07315724.2000.10718911
Saito T, Murakami M, Shimazaki Y et al (2003) Association between alveolar bone loss and elevated serum C-reactive protein in Japanese men. J Periodontol 74:1741–1746. https://doi.org/10.1902/jop.2003.74.12.1741
Caúla AL, Lira-Junior R, Tinoco EMB, Fischer RG (2015) Serum creatinine and alkaline phosphatase levels are associated with severe chronic periodontitis. J Periodontal Res 50:793–797. https://doi.org/10.1111/jre.12266
Varela-López A, Giampieri F, Bullón P et al (2016) A systematic review on the implication of minerals in the onset, severity and treatment of periodontal disease. Molecules 21:1183. https://doi.org/10.3390/molecules21091183
Kim J-W, Kong K-A, Kim H-Y et al (2014) The association between bone mineral density and periodontitis in Korean adults (KNHANES 2008-2010). Oral Dis 20:609–615. https://doi.org/10.1111/odi.12179
Imamura F, O’Connor L, Ye Z, et al (2015) Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ h3576. https://doi.org/10.1136/bmj.h3576
Stanhope KL, Medici V, Bremer AA et al (2015) A dose-response study of consuming high-fructose corn syrup-sweetened beverages on lipid/lipoprotein risk factors for cardiovascular disease in young adults. Am J Clin Nutr 101:1144–1154. https://doi.org/10.3945/ajcn.114.100461
Lana A, Rodríguez-Artalejo F, Lopez-Garcia E (2014) Consumption of sugar-sweetened beverages is positively related to insulin resistance and higher plasma leptin concentrations in men and nonoverweight women. J Nutr 144:1099–1105. https://doi.org/10.3945/jn.114.195230
Yoshida M, McKeown NM, Rogers G et al (2007) Surrogate markers of insulin resistance are associated with consumption of sugar-sweetened drinks and fruit juice in middle and older-aged adults. J Nutr 137:2121–2127. https://doi.org/10.1093/jn/137.9.2121
Bauhoff S (2011) Systematic self-report bias in health data: impact on estimating cross-sectional and treatment effects. Heal Serv Outcomes Res Methodol 11:44–53. https://doi.org/10.1007/s10742-011-0069-3
Willett W (2012) Nutritional epidemiology. Oxford university press
Funding
This study was funded by FAPEMA (Maranhão State Foundation for Research and Scientific and Technological Development), CNPq (National Council for Scientific and Technological Development) and CAPES (Coordination for the Improvement of Higher Education Personnel).
Author information
Authors and Affiliations
Contributions
A.R.O. Moreira and C.C.C. Ribeiro contributed to conception, design, data acquisition, analysis, and interpretation, and drafted and critically revised the manuscript; R.F.L. Batista, E.B.A.F. Thomaz, C.M.C. Alves, and A.A.M. Silva contributed to conception, design and data interpretation, and drafted and critically revised the manuscript; L.L.C. Ladeira contributed to conception and drafted and critically revised the manuscript; M.C. Saraiva and M.A. Brondani contributed to conception and data interpretation and critically revised the manuscript. All authors gave final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the Federal University of Maranhão (CAAE 49096315.2.0000.5086, process number 1.302.489) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moreira, A.R.O., Batista, R.F.L., Ladeira, L.L.C. et al. Higher sugar intake is associated with periodontal disease in adolescents. Clin Oral Invest 25, 983–991 (2021). https://doi.org/10.1007/s00784-020-03387-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03387-1