Abstract
Objectives
This cross-sectional study determined the prevalence of painful TMD and its impact on jaw function, psychological status and oral health-related quality of life (OHRQoL) in postoperative Chinese patients. It also assessed factors influencing OHRQoL of these patients.
Materials and methods
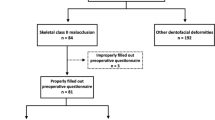
Subjects were recruited from the National Dental Centre Singapore dentofacial deformity registry. Invitations to participate in the study were sent to patients who sought treatment from March 2011 to November 2017. Patients who consented were directed to an online link to complete a series of questionnaires based on the Diagnostic Criteria for TMD (DC-TMD) and the orthognathic quality of life questionnaire (OQLQ).
Results
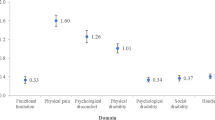
The subjects (n = 99) had a mean age of 25.2 ± 6.0 years and postoperative time of 29.4 ± 22.7 months. 18.2% were found to suffer from pain-related TMD postorthognathic surgery and these patients (n = 18) had significantly higher median JFLS-8 score than those without TMD pain (p = 0.008). Time since surgery was significantly associated with OHRQoL (p = 0.00000026).
Conclusions
Prevalence of painful TMD and psychological distress was low while prevalence of jaw functional limitation was moderately high in postoperative class III Chinese patients.
Clinical relevance
Painful TMD impacted jaw function especially when subjects open wide enough to drink, yawn, talk and smile but had no significant consequence on psychological status and OHRQoL.

Similar content being viewed by others
References
Chew MT (2006) Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angle Orthod 76:806–809
Song HC, Throckmorton GS, Ellis E, Sinn DP (1997) Functional and morphologic alterations after anterior or inferior repositioning of the maxilla. J Oral Maxillofac Surg 55:41–49 discussion 49-50
Wisth PJ (1984) Mandibular function and dysfunction in patients with mandibular prognathism. Am J Orthod 85:193–198
Katsavrias EG, Halazonetis DJ (2005) Condyle and fossa shape in class II and class III skeletal patterns: a morphometric tomographic study. Am J Orthod Dentofac Orthop 128:337–346
Ueki K, Marukawa K, Shimada M, Nakagawa K, Yamamoto E (2005) Change in condylar long axis and skeletal stability following sagittal split ramus osteotomy and intraoral vertical ramus osteotomy for mandibular prognathia. J Oral Maxillofac Surg 63:1494–1499
Costa F, Robiony M, Sembronio S, Polini F, Politi M (2001) Stability of skeletal class III malocclusion after combined maxillary and mandibular procedures. Int J Adult Orthodon Orthognath Surg 16:179–192
Farella M, Michelotti A, Bocchino T, Cimino R, Laino A, Steenks MH (2007) Effects of orthognathic surgery for class III malocclusion on signs and symptoms of temporomandibular disorders and on pressure pain thresholds of the jaw muscles. Int J Oral Maxillofac Surg 36:583–587
Aoyama S, Kino K, Kobayashi J, Yoshimasu H, Amagasa T (2005) Clinical evaluation of the temporomandibular joint following orthognathic surgery--multiple logistic regression analysis. J Med Dent Sci 52:109–114
Abrahamsson C, Henrikson T, Nilner M, Sunzel B, Bondemark L, Ekberg EC (2013) TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int J Oral Maxillofac Surg 42:752–758
Sebastiani AM, Baratto-Filho F, Bonotto D, Kluppel LE, Rebellato NLB, da Costa DJ, Scariot R (2016) Influence of orthognathic surgery for symptoms of temporomandibular dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol 121:119–125
Jung H-D, Jung Y-S, Park H-S (2009) The chronologic prevalence of temporomandibular joint disorders associated with bilateral intraoral vertical ramus osteotomy. J Oral Maxillofac Surg 67:797–803
Yoon SY, Song JM, Kim YD, Chung IK, Shin SH (2015) Clinical changes of TMD and condyle stability after two jaw surgery with and without preceding TMD treatments in class III patients. Maxillofac Plast Reconstr Surg 37. https://doi.org/10.1186/s40902-015-0008-2
Al-Riyami S, Cunningham SJ, Moles DR (2009) Orthognathic treatment and temporomandibular disorders: a systematic review. Part 2. Signs and symptoms and meta-analyses. Am J Orthod Dentofac Orthop 136:626.e1–626.16 discussion 626-627
Yazdani J, Ebrahimi H, Talesh KT, Khashabi E, Pourshahidi S, Tadbir AA (2010) Comparing the effect of 3 orthognathic surgical methods on the mandibular range of movement. J Craniofac Surg 21:703–705
Ko WCE, Huang CS, Lo LJ, Chen YR (2012) Longitudinal observation of mandibular motion pattern in patients with skeletal class III malocclusion subsequent to orthognathic surgery. J Oral Maxillofac Surg 70:e158–e168
Nagamine T, Kobayashi T, Nakajima T, Hanada K (1993) The effects of surgical-orthodontic correction of skeletal class III malocclusion on mandibular movement. J Oral Maxillofac Surg 51:385–389
Al-Belasy FA, Tozoglu S, Dolwick MF (2013) Mandibular hypomobility after orthognathic surgery: a review article. J Oral Maxillofac Surg 71:1967.e1–1967.e11
Phillips C, Bennett ME, Broder HL (1998) Dentofacial disharmony: psychological status of patients seeking treatment consultation. Angle Orthod 68:547–556
Kim SO, Jin MY, Yu BC (2015) Psychological state of the patients according to skeletal class III malocclusion symptoms. J Korean Soc Dent Hyg 15:205–216
Reissmann DR, John MT, Schierz O, Wassell RW (2007) Functional and psychosocial impact related to specific temporomandibular disorder diagnoses. J Dent 35:643–650
Silvola A-S, Tolvanen M, Rusanen J, Sipilä K, Lahti S, Pirttiniemi P (2016) Do changes in oral health-related quality-of-life, facial pain and temporomandibular disorders correlate after treatment of severe malocclusion? Acta Odontol Scand 74:44–50
Song YL, Yap AUJ (2017) Orthognathic treatment of dentofacial disharmonies: its impact on temporomandibular disorders, quality of life, and psychosocial wellness. Cranio J Craniomandib Pract 35:52–57
Sun H, Shang H-T, He L-S, Ding M-C, Su Z-P, Shi Y-L (2018) Assessing the quality of life in patients with dentofacial deformities before and after orthognathic surgery. J Oral Maxillofac Surg 76:2192–2201. https://doi.org/10.1016/j.joms.2018.03.026
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, Ettlin D, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache 28:6–27
Cunningham SJ, Garratt AM, Hunt NP (2000) Development of a condition-specific quality of life measure for patients with dentofacial deformity: I. Reliability of the instrument. Community Dent Oral Epidemiol 28:195–201
Gonzalez YM, Schiffman E, Gordon SM, Seago B, Truelove EL, Slade G, Ohrbach R (2011) Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity. J Am Dent Assoc 1939 142:1183–1191
Ohrbach R, Larsson P, List T (2008) The jaw functional limitation scale: development, reliability, and validity of 8-item and 20-item versions. J Orofac Pain 22:219–230
Kroenke K, Spitzer RL, Williams JBW, Löwe B (2009) An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 50:613–621
Cunningham SJ, Garratt AM, Hunt NP (2002) Development of a condition-specific quality of life measure for patients with dentofacial deformity: II. Validity and responsiveness testing. Community Dent Oral Epidemiol 30:81–90
di Paolo C, Pompa G, Arangio P, di Nunno A, Di Carlo S, Rosella D, Papi P, Cascone P (2017) Evaluation of temporomandibular disorders before and after orthognathic surgery: therapeutic considerations on a sample of 76 patients. J Int Soc Prev Community Dent 7:125–129
Kadir K, Khor K, Loh Y (2015) The association of temporomandibular disorders and orthognathic surgery. Ann Dent Univ Malaya 22:6–14
Pow EH, Leung KC, McMillan AS (2001) Prevalence of symptoms associated with temporomandibular disorders in Hong Kong Chinese. J Orofac Pain 15:228–234
Al-Moraissi EA, Perez D, Ellis E (2017) Do patients with malocclusion have a higher prevalence of temporomandibular disorders than controls both before and after orthognathic surgery? A systematic review and meta-analysis. J Cranio-Maxillo-fac Surg 45:1716–1723
Fang B, Shen G-F, Yang C, Wu Y, Feng Y-M, Mao L-X, Xia Y-H (2009) Changes in condylar and joint disc positions after bilateral sagittal split ramus osteotomy for correction of mandibular prognathism. Int J Oral Maxillofac Surg 38:726–730
Feinerman DM, Piecuch JF (1995) Long-term effects of orthognathic surgery on the temporomandibular joint: comparison of rigid and nonrigid fixation methods. Int J Oral Maxillofac Surg 24:268–272
Lei J, Fu J, Yap AUJ, Fu K-Y (2016) Temporomandibular disorders symptoms in Asian adolescents and their association with sleep quality and psychological distress. Cranio J Craniomandib Pract 34:242–249
Natu VP, Yap AU-J, Su MH, Irfan Ali NM, Ansari A (2018) Temporomandibular disorder symptoms and their association with quality of life, emotional states and sleep quality in South-East Asian youths. J Oral Rehabil 45:756–763
Miles TS, Flavel SC, Nordstrom MA (2004) Stretch reflexes in the human masticatory muscles: a brief review and a new functional role. Hum Mov Sci 23:337–349
Luo Y, Svensson P, Jensen JD, Jensen T, Neumann B, Arendt-Nielsen L, Wang K (2014) Jaw-stretch reflex is weaker in patients after orthognathic surgery. Arch Oral Biol 59:1321–1327
Teng TT-Y, Ko EW-C, Huang CS, Chen Y-R (2015) The effect of early physiotherapy on the recovery of mandibular function after orthognathic surgery for class III correction: part I--jaw-motion analysis. J Cranio-Maxillo-fac Surg 43:131–137
Ko EW-C, Teng TT-Y, Huang CS, Chen Y-R (2015) The effect of early physiotherapy on the recovery of mandibular function after orthognathic surgery for class III correction. Part II: electromyographic activity of masticatory muscles. J Cranio-Maxillo-fac Surg 43:138–143
Eslamipour F, Najimi A, Tadayonfard A, Azamian Z (2017) Impact of orthognathic surgery on quality of life in patients with dentofacial deformities. Int J Dent 2017:1–6. https://doi.org/10.1155/2017/4103905
Soh CL, Narayanan V (2013) Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery—a systematic review. Int J Oral Maxillofac Surg 42:974–980
Lei J, Liu M-Q, Yap AUJ, Fu K-Y (2015) Sleep disturbance and psychologic distress: prevalence and risk indicators for temporomandibular disorders in a Chinese population. J Oral Facial Pain Headache 29:24–30
Osório FL, Lima MP, Chagas MHN (2015) Screening tools for psychiatry disorders in cancer setting: caution when using. Psychiatry Res 229:739–742
Yap AUJ, Chua EK, Tan KBC, Chan YH (2004) Relationships between depression/somatization and self-reports of pain and disability. J Orofac Pain 18:220–225
Egleston BL, Miller SM, Meropol NJ (2011) The impact of misclassification due to survey response fatigue on estimation and identifiability of treatment effects. Stat Med 30:3560–3572
Almoznino G, Zini A, Zakuto A, Sharav Y, Haviv Y, Avraham H, Chweidan H, Noam Y, Benoliel R (2015) Oral health-related quality of life in patients with temporomandibular disorders. J Oral Facial Pain Headache 29:231–241
Song YL, Yap AU-J (2018) Outcomes of therapeutic TMD interventions on oral health related quality of life: a qualitative systematic review. Quintessence Int Berl Ger 1985 49:487–496
Durham J, Steele JG, Wassell RW, Exley C, Meechan JG, Allen PF, Moufti MA (2011) Creating a patient-based condition-specific outcome measure for temporomandibular disorders (TMDs): Oral Health Impact Profile for TMDs (OHIP-TMDs). J Oral Rehabil 38:871–883
Nichols GAL, Antoun JS, Fowler PV, Al-Ani AH, Farella M (2018) Long-term changes in oral health-related quality of life of standard, cleft, and surgery patients after orthodontic treatment: a longitudinal study. Am J Orthod Dentofac Orthop 153:224–231
Al-Asfour A, Waheedi M, Koshy S (2018) Survey of patient experiences of orthognathic surgery: health-related quality of life and satisfaction. Int J Oral Maxillofac Surg 47:726–731
Emadian Razvadi ES, Soheilifar S, Esmaeelinejad M, Naghdi N (2017) Evaluation of the changes in the quality of life in patients undergoing orthognathic surgery: a multicenter study. J Craniofac Surg 28:e739–e743
Acknowledgements
We would like to thank Assistant Professor Fan Qiao and Nadkarni Nivedita Vikas from the Duke-National University of Singapore Medical School for their help in statistical analysis.
Funding
Cost of printing the invitation letters and postage for the study were provided by the National Dental Centre Singapore.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research was approved by the SingHealth Centralized Institutional Review Board (CIRB Ref 2016/2232).
Informed consent
There is implied consent when participants logged on to fill up the online questionnaires.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Song, Y.L., Yap, A.Uj. Impact of pain-related temporomandibular disorders on jaw functional limitation, psychological distress and quality of life in postoperative class III East Asian patients. Clin Oral Invest 24, 953–961 (2020). https://doi.org/10.1007/s00784-019-02994-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02994-x