Abstract
Objective
This study investigated the shear bond strength (SBS) and interface between a resin composite and a new high-viscous glass ionomer cement (HV-GIC), a HV-GIC, a resin-modified glass ionomer cement (RM-GIC), a bulk-fill flowable composite, and a regular flowable composite bonded with various adhesive systems.
Methods and materials
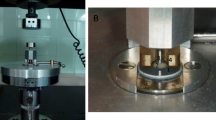
A resin composite (Filtek Z350) was bonded to a new HV-GIC (EQUIA Forte Fil) using various adhesive systems, including a universal adhesive in self-etch and etch-and-rinse mode (Scotchbond Universal), a two-step etch-and-rinse adhesive (Scotchbond 1-XT), a one-step self-etch adhesive (Optibond All-in-one) tested also after silane application (Monobond Plus), and a coating material (EQUIA Forte Coat). The resin composite was also bonded to a HV-GIC (Fuji IX GP), a RM-GIC (Fuji II LC), a bulk-fill flowable composite (SDR), and a regular flowable composite (Tetric Evo Flow) with the universal adhesive in self-etch mode (Scotchbond Universal). Two-way ANOVA followed by Dunnett’s post hoc test was used to investigate the difference in SBS. Failures were analyzed by chi-square test. Bonding interfaces were examined by environmental scanning electron microscopy (E-SEM).
Results
SBS to EQUIA Forte Fil was significantly lower with Scotchbond 1-XT than with all other adhesive systems. By using Scotchbond Universal with the self-etch technique, the SBS to EQUIA Forte Fil was significantly higher than the SBS to Fuji IX GP and significantly lower than the SBS to Fuji II LC, SDR, and Tetric Evo Flow. E-SEM images showed an intimate contact at all interfaces examined.
Conclusion
EQUIA Forte Fil showed satisfactory SBS and interfaces with all adhesives tested.
Clinical relevance
Bonding between the resin composite and HV-GIC can be achieved using a universal adhesive in self-etch mode, an easy-to-use adhesive system.



Similar content being viewed by others
References
Dietschi D, Spreafico R (2015) Evidence-based concepts and procedures for bonded inlays and onlays. Part I. Historical perspectives and clinical rationale for a biosubstitutive approach. Int J Esthet Dent 10:210–227
Rocca GT, Krejci I (2007) Bonded indirect restorations for posterior teeth: from cavity preparation to provisionalization. Quintessence Int 38:371–379
Zaruba M, Göhring TN, Wegehaupt FJ, Attin T (2013) Influence of a proximal margin elevation technique on marginal adaptation of ceramic inlays. Acta Odontol Scand 71:317–324. https://doi.org/10.3109/00016357.2012.680905
Fragkou S, Nikolaidis A, Tsiantou D, Achilias D, Kotsanos N (2013) Tensile bond characteristics between composite resin and resin-modified glass-ionomer restoratives used in the open-sandwich technique. Eur Arch Paediatr Dent 14:239–245. https://doi.org/10.1007/s40368-013-0055-2
Andersson-Wenckert IE, van Dijken JW, Kieri C (2004) Durability of extensive Class II open-sandwich restorations with a resin-modified glass ionomer cement after 6 years. Am J Dent 17:43–50
Dietschi D, Spreafico R (1998) Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthetic Dent 10:47–54 quiz 56
Kielbassa AM, Philipp F (2015) Restoring proximal cavities of molars using the proximal box elevation technique: systematic review and report of a case. Quintessence Int 46:751–764. https://doi.org/10.3290/j.qi.a34459
Ilgenstein I, Zitzmann NU, Bühler J, Wegehaupt FJ, Attin T, Weiger R, Krastl G (2015) Influence of proximal box elevation on the marginal quality and fracture behavior of root-filled molars restored with CAD/CAM ceramic or composite onlays. Clin Oral Investig 19:1021–1028. https://doi.org/10.1007/s00784-014-1325-z
Dietschi D, Olsburgh S, Krejci I, Davidson C (2003) In vitro evaluation of marginal and internal adaptation after occlusal stressing of indirect class II composite restorations with different resinous bases. Eur J Oral Sci 111:73–80
Marchesi G, Spreafico R, Frassetto A, Turco G, Di Lenarda R, Cadenaro M, Breschi L (2014) Cervical margin-relocation of CAD/CAM lithium disilicate ceramic crown using resin-composite. Dent Mater 30:e14. doi: https://doi.org/10.1016/j.dental.2014.08.029
Chuang SF, Liu JK, Chao CC, Liao FP, Chen YH (2001) Effects of flowable composite lining and operator experience on microleakage and internal voids in class II composite restorations. J Prosthet Dent 85:177–183. https://doi.org/10.1067/mpr.2001.113780
Boruziniat A, Gharaee S, Sarraf Shirazi A, Majidinia S, Vatanpour M (2016) Evaluation of the efficacy of flowable composite as lining material on microleakage of composite resin restorations: a systematic review and meta-analysis. Quintessence Int 47:93–101. https://doi.org/10.3290/j.qi.a35260
Hernandes NMAP, Catelan A, Soares GP, Ambrosano GM, Lima DA, Marchi GM, Martins LR, Aguiar FH (2014) Influence of flowable composite and restorative technique on microleakage of class II restorations. J Investig Clin Dent 5:283–288. https://doi.org/10.1111/jicd.12058
Baroudi K, Rodrigues JC (2015) Flowable resin composites: a systematic review and clinical considerations. J Clin Diagn Res JCDR 9:ZE18–ZE24. https://doi.org/10.7860/JCDR/2015/12294.6129
Baroudi K, Silikas N, Watts DC (2009) In vitro pulp chamber temperature rise from irradiation and exotherm of flowable composites. Int J Paediatr Dent 19:48–54. https://doi.org/10.1111/j.1365-263X.2007.00899.x
Koubi S, Raskin A, Dejou J, About I, Tassery H, Camps J, Proust JP (2009) Effect of dual cure composite as dentin substitute on marginal integrity of class II open-sandwich restorations. Oper Dent 34:150–156. https://doi.org/10.2341/08-29
Roggendorf MJ, Krämer N, Dippold C, Vosen VE, Naumann M, Jablonski-Momeni A, Frankenberger R (2012) Effect of proximal box elevation with resin composite on marginal quality of resin composite inlays in vitro. J Dent 40:1068–1073. https://doi.org/10.1016/j.jdent.2012.08.019
Heintze SD, Rousson V (2012) Clinical effectiveness of direct class II restorations - a meta-analysis. J Adhes Dent 14:407–431. https://doi.org/10.3290/j.jad.a28390
Khoroushi M, Keshani F (2013) A review of glass-ionomers: from conventional glass-ionomer to bioactive glass-ionomer. Dent Res J (Isfahan) 10:411–420
Lazaridou D, Belli R, Krämer N, Petschelt A, Lohbauer U (2015) Dental materials for primary dentition: are they suitable for occlusal restorations? A two-body wear study. Eur Arch Paediatr Dent 16:165–172. https://doi.org/10.1007/s40368-014-0151-y
Gurgan S, Kutuk ZB, Ergin E, Oztas SS, Cakir FY (2015) Four-year randomized clinical trial to evaluate the clinical performance of a glass ionomer restorative system. Oper Dent 40:134–143. https://doi.org/10.2341/13-239-C
Fukegawa D, Hayakawa S, Yoshida Y, Suzuki K, Osaka A, Van Meerbeek B (2006) Chemical interaction of phosphoric acid ester with hydroxyapatite. J Dent Res 85:941–944. https://doi.org/10.1177/154405910608501014
Kadoma Y (2002) Surface treatment agent for dental metals using a thiirane monomer and a phosphoric acid monomer. Dent Mater J 21:156–169. https://doi.org/10.4012/dmj.21.156
Chen L, Suh BI, Brown D, Chen X (2012) Bonding of primed zirconia ceramics: evidence of chemical bonding and improved bond strengths. Am J Dent 25:103–108
Kim RJ, Woo JS, Lee IB, Yi YA, Hwang JY, Seo DG (2015) Performance of universal adhesives on bonding to leucite-reinforced ceramic. Biomater Res 19:11. https://doi.org/10.1186/s40824-015-0035-1
Lee Y, Kim JH, Woo JS, Yi YA, Hwang JY, Seo DG (2015) Analysis of self-adhesive resin cement microshear bond strength on leucite-reinforced glass-ceramic with/without pure silane primer or universal adhesive surface treatment. Biomed Res Int 2015:361893. https://doi.org/10.1155/2015/361893
Yoshida Y, Nagakane K, Fukuda R, Nakayama Y, Okazaki M, Shintani H, Inoue S, Tagawa Y, Suzuki K, De Munck J, Van Meerbeek B (2004) Comparative study on adhesive performance of functional monomers. J Dent Res 83:454–458. https://doi.org/10.1177/154405910408300604
Çolak H, Tokay U, Uzgur R, Uzgur Z, Ercan E, Hamidi MM (2016) The effect of different adhesives and setting times on bond strength between Biodentine and composite. J Appl Biomater Funct Mater 14:e217–e222. https://doi.org/10.5301/jabfm.5000266
Odabaş ME, Bani M, Tirali RE (2013) Shear bond strengths of different adhesive systems to biodentine. Sci World J 2013:626103–626105. https://doi.org/10.1155/2013/626103
Zhang Y, Burrow MF, Palamara JEA, Thomas CDL (2011) Bonding to glass ionomer cements using resin-based adhesives. Oper Dent 36:618–625. https://doi.org/10.2341/10-140-L
Wexler G, Beech DR (1988) Bonding of a composite restorative material to etched glass ionomer cement. Aust Dent J 33:313–318. https://doi.org/10.1111/j.1834-7819.1988.tb04185.x
Hinoura K, Moore BK, Phillips RW (1988) Tensile bond strength between glass ionomer cements and composite resins. J Am Dent Assoc 114:167–172. https://doi.org/10.14219/jada.archive.1987.0021
Kandaswamy D, Rajan KJ, Venkateshbabu N, Porkodi I (2012) Shear bond strength evaluation of resin composite bonded to glass-ionomer cement using self-etching bonding agents with different pH: in vitro study. J Conserv Dent JCD 15:27–31. https://doi.org/10.4103/0972-0707.92602
Nurrohman H, Nakashima S, Takagaki T, Sadr A, Nikaido T, Asakawa Y, Uo M, Marshall SJ, Tagami J (2015) Immobilization of phosphate monomers on collagen induces biomimetic mineralization. Biomed Mater Eng 25:89–99. https://doi.org/10.3233/BME-141243
Shimazu K, Karibe H, Ogata K (2014) Effect of artificial saliva contamination on adhesion of dental restorative materials. Dent Mater J 33:545–550. https://doi.org/10.4012/dmj.2014-007
Park J, Chang J, Ferracane J, Lee IB (2008) How should composite be layered to reduce shrinkage stress: incremental or bulk filling? Dent Mater 24:1501–1505. https://doi.org/10.1016/j.dental.2008.03.013
Cebe MA, Cebe F, Cengiz MF, Cetin AR, Arpag OF, Ozturk B (2015) Elution of monomer from different bulk fill dental composite resins. Dent Mater 31:e141–e149. https://doi.org/10.1016/j.dental.2015.04.008
Dursun E, Fron-Chabouis H, Attal JP, Raskin A (2016) Bisphenol a release: survey of the composition of dental composite resins. Open Dent J 10:446–453. https://doi.org/10.2174/1874210601610010446
Sideridou ID, Achilias DS (2005) Elution study of unreacted Bis-GMA, TEGDMA, UDMA, and Bis-EMA from light-cured dental resins and resin composites using HPLC. J Biomed Mater Res B Appl Biomater 74:617–626. https://doi.org/10.1002/jbm.b.30252
Calesini G, Micarelli C, Fabianelli A, Papacchini F (2014) The evaluation of marginal gap with and without optical aids: clinicians versus technicians. Int J Prosthodont 27:161–164. https://doi.org/10.11607/ijp.3649
Mamoun J (2015) Preparing and restoring composite resin restorations. The advantage of high magnification loupes or the dental surgical operating microscope. N Y State Dent J 81:18–23
Magne P (2014) IDS: Immediate Dentin Sealing (IDS) for tooth preparations. J Adhes Dent 16:594. https://doi.org/10.3290/j.jad.a33324
Panahandeh N, Torabzadeh H, Ghassemi A, Mahdian M, Akbarzadeh Bagheban A, Moayyedi S (2015) Effect of bonding application time on bond strength of composite resin to glass ionomer cement. J Dent (Tehran) 12:859–867
Beriat NC, Nalbant D (2009) Water absorption and HEMA release of resin-modified glass-ionomers. Eur J Dent 3:267–272
Cattani-Lorente MA, Dupuis V, Payan J, Moya F, Meyer JM (1999) Effect of water on the physical properties of resin-modified glass ionomer cements. Dent Mater 15:71–78. https://doi.org/10.1016/S0109-5641(99)00016-0
Karaoğlanoğlu S, Akgül N, Ozdabak HN, Akgül HM (2009) Effectiveness of surface protection for glass-ionomer, resin-modified glass-ionomer and polyacid-modified composite resins. Dent Mater J 28:96–101. https://doi.org/10.4012/dmj.28.96
Gopikrishna V, Abarajithan M, Krithikadatta J, Kandaswamy D (2009) Shear bond strength evaluation of resin composite bonded to GIC using three different adhesives. Oper Dent 34:467–471. https://doi.org/10.2341/08-009-L
Tanumiharja M, Burrow MF, Tyas MJ (2000) Microtensile bond strengths of glass ionomer (polyalkenoate) cements to dentine using four conditioners. J Dent 28:361–366. https://doi.org/10.1016/S0300-5712(00)00009-9
Knight GM, McIntyre JM, Mulyani (2006) Bond strengths between composite resin and auto cure glass ionomer cement using the co-cure technique. Aust Dent J 51:175–179. https://doi.org/10.1111/j.1834-7819.2006.tb00423.x
Coutinho E, Yoshida Y, Inoue S, Fukuda R, Snauwaert J, Nakayama Y, De Munck J, Lambrechts P, Suzuki K, Van Meerbeek B (2007) Gel phase formation at resin-modified glass-ionomer/tooth interfaces. J Dent Res 86:656–661. https://doi.org/10.1177/154405910708600714
Tay KCY, Loushine BA, Oxford C, Kapur R, Primus CM, Gutmann JL, Loushine RJ, Pashley DH, Tay FR (2007) In vitro evaluation of a Ceramicrete-based root-end filling material. J Endod 33:1438–1443. https://doi.org/10.1016/j.joen.2007.07.038
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Rights and permissions
About this article
Cite this article
Francois, P., Vennat, E., Le Goff, S. et al. Shear bond strength and interface analysis between a resin composite and a recent high-viscous glass ionomer cement bonded with various adhesive systems. Clin Oral Invest 23, 2599–2608 (2019). https://doi.org/10.1007/s00784-018-2678-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2678-5