Abstract
Objectives
The marginal quality of ceramic inlays was evaluated after the use of three different instrumental finishing methods in mesio-occluso-distal (mod) cavity boxes in vitro after hydrothermal loading (HTL).
Materials and methods
Caries-free human molars were divided into three groups. Mod-cavities were conventionally prepared. Box finishing was performed in every group with rotating (RI), sonic (SI), or ultrasonic (USI) instruments. Surface roughness was examined. Twelve mod-cavities remained untreated. Continuous margin quality was evaluated with scanning electron microscopy (SEM). Ceramic inlays were cemented into cavities. After HTL microleakage, marginal and absolute marginal gaps were examined. All data were analyzed statistically.
Results
Significant differences were found, between cavity surface roughness of RI and SI groups, the RI and USI groups, but not between microleakage, marginal, absolute marginal gaps after HTL and in proximal marginal quality. No correlations between microleakage and marginal gaps nor between microleakage and surface roughness were found.
Conclusion
Mod-cavity proximal box finishing with SI or USI resulted in a higher surface roughness than the use of RI. The type of the finishing method did not influence the marginal quality of ceramic inlays. For the mod-cavity finishing, the use of SI and USI could be an alternative instrumental method to conventional RI methods with a lower risk of iatrogenic damage of the adjacent teeth.
Clinical relevance
This study allows the practitioner to better determine the proper indications and limitations of the sonic and ultrasonic instruments for mod-cavity proximal box finishing.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Qualitative cavity preparation without discomfort is very important in restorative dentistry [1]. The restoration geometry, design considerations, preparation methods, and loading conditions are key factors for the long-term success of dental restorations [2,3,4,5,6,7,8]. For tooth-colored ceramic inlays in esthetic dentistry, the long-term success is an actual problem [7]. Accordingly, information and discussion about the applications and effects of the different instrumental methods of cavity preparation [1, 9], technical requirements, and the effective preparation of dental tissues [7] are in demand.
According to the concept of “minimally hazardous dentistry” [7, 10], technical details about the application of different instruments for cavity preparation are clinically relevant because side effects, such as border defects and very irregular surfaces, especially in proximal box cavities [9]; cracks, especially in the enamel [1]; and iatrogenic damage to adjacent teeth [11,12,13], may occur. This mechanical damage may result in possible biological complications, such as tooth sensitivity and bacterial leakage [7]. Different types of instrumental methods for dental cavity preparation are currently in use: conventional-rotating [9], laser [1, 14, 15], sonic [9], or ultrasonic preparation [16, 17]. Mechanical damage of the teeth is more likely to occur with the use of rotating instruments [9]. Ultrasonic instruments are widely used in dentistry because of better efficiency, visualization, operative convenience, precise cutting ability [17], and success in accessing difficult areas on the preparation margin [16].
Molar esthetic restoration is in demand [18]. Ceramic inlays are indicated for tooth restoration in extended mod-cavities with a loss of proximal contacts [19]. The marginal quality of ceramic inlays, especially the quality of the proximal margins, is very important for providing highly esthetic, long-lasting, plaque-resistant restorations [2, 20, 21]. The presence of surface irregularities in the inlay proximal area can increase plaque formation, gingival irritation, recurrent caries, abrasiveness, wear kinetics, staining, and tactile perception by the patient [20, 22,23,24]. Marginal quality is of clinical importance for the process of bacterial retention [22, 25]. Therefore, the possible influence of different types of dental restorations on microleakage and marginal adaptation should be demonstrated with the use of different methods for cavity preparation [1, 2]. However, only limited information is available about the proximal margin quality of the ceramic inlays in molar teeth after mesio-occluso-distal cavity proximal box finishing with sonic and ultrasonic instruments after hydrothermal loading (HTL) in vitro [9, 21].
The marginal quality of the ceramic inlay approximal area is of clinical importance because the ceramic inlay approximal area is located in the interdental space, and tooth brushing in this area is restricted [16, 26].
The aim of this in vitro study is to evaluate the influence of different alternative methods of shaping and finishing mod-cavity proximal boxes on the adaptation of ceramic inlays to the tooth morphology and bonding quality.
The null hypothesis for the present study was that three different finishing methods of mod-cavities in human molars would not differ in their effects on the surface roughness and border quality of the proximal boxes, microleakage, and marginal gap of the ceramic inlays within the enamel.
Materials and methods
Tooth collection
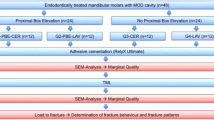
Tooth collection was approved by the ethical committee of Witten/Herdecke University (permission 116/2013). For this study, a total of 60 extracted human molar teeth were collected. They were caries-free, lacked dental calculus, and had completed root growth, comparable sizes, and absolute integrity. Immediately after extraction, the teeth were stored in 0.9% NaCl containing 0.1% thymol at room temperature (maximum 1–3 months) until use. Tissue remnants on the teeth surface were removed with a universal scaler. The teeth were randomly distributed into three groups (Fig. 1).
Cavity preparation
For the realistic simulation of tooth preparation, a specially designed original lower jaw model was constructed for precise positioning and stable fixation of the experimental teeth (Fig. 2). Initially, the roots of the experimental teeth were coated with condensation-K-Silikon (HLW Dental, Wernberg-Köblitz, Germany). Then, the experimental teeth were placed in the U-profile (the row) of the lower jaw between teeth 45 and 47 (Frasaco GmbH, Tettnang, Germany) and aligned along the occlusion. Then, teeth 45 and 47 were moved until the proximal contacts from both sides of the experimental tooth were reached. Thereafter, the original lower jaw model with the experimental tooth was placed and fixed in the head model (Frasaco GmbH, Tettnang, Germany) with the face mask P-6 GM (Frasaco GmbH, Tettnang, Germany) and the opposing upper jaw ANKA-4 (Frasaco GmbH, Tettnang, Germany).
All specimen preparations were performed by the same operator and calibrated prior to the study by one of the authors to avoid inter-examiner differences.
For the preparation, the AG ceramics guidelines of Ahlers et al. 2009 [27] for a ceramic inlay with a mod-cavity were followed. The following geometrical parameters for the mod-cavity were kept: a diverging angle of approximately 6°, a minimal depth of the occlusal box in the deepest area of the fissure of approximately 1.5 mm, a minimal width of the isthmus of approximately 1.5 mm, a cavity surface angle of approximately 90°, and a planar occlusal and proximal cavity floor. The cervical margin preparation was located in enamel with a maximum dimension of 1.5 mm above the enamel-cementum junction.
The dimensions of the mod-cavities were maintained with the preparation instruments with defined conicity and laser depth markings and were finally controlled with the CP-15 UNC periodontometer (Hu-Friedy Mfg. Co., LLC, Tuttlingen, Germany). The transitions within the mod-cavity were rounded off, and the proximal contacts to the adjacent tooth were completely separated.
The mod-cavity preparation was performed in three steps: (1) initial whole mod-cavity shaping in all groups (n = 60), (2) mod-cavity proximal box finishing within every three groups (n = 20), and (3) rounding and smoothing all sharp edges inside of the mod-cavity in all groups (n = 60). Initial whole cavity shaping for 60 teeth was performed in all groups using the same method with the Synea Vision WK-99 LT handpiece (W & H Germany GmbH, Laufen, Germany) under ca. 80% power (ratio 1:5, engine speed 32,000 rpm, speed of the instrument 160,000 rpm) and diamond instruments. Then, a purely occlusal limited cavity along the main fissure was produced with the 959KRD 314,018 non-ringed diamond conical grinder (Komet, Lemgo, Germany) (grain size ca. 100 μm, laser marking at 2 and 4 mm, conicity ca. 2°). After this, the proximal box to the dissolution of the basal contact point was created with a 6847KRD 314 016 green ringed conical diamond grinder (Komet, Lemgo, Germany) (grain size ca. 125 μm, laser marking at 2 and 4 mm, conicity ca. 2°). This was done with the protection of the adjacent tooth with steel-band matrices, which were fixed with a wooden wedge. The occlusal box was smoothed with the red-ringed conical diamond instrument 8959KR 314 018 (Komet, Lemgo, Germany) (grain size ca. 30–45 μm, conicity ca. 2°). After the initial whole mod-cavity shaping of five teeth, the used instruments were replaced with new ones. This rule was also applied to subsequent proximal box finishing within groups.
Proximal box finishing was performed with three different methods and instruments in the three groups.
Proximal box finishing in group 1
Proximal box finishing in group 1 was performed with the red high-speed angle Synea Vision WK-99 LT handpiece (W & H Germany GmbH, Laufen, Germany) under 10–20% power (ratio 1:5, engine speed 4000–8.000 rpm, speed of the instrument 20,000–40,000 rpm) and the rotating red-ringed conical diamond instrument 8847KR 314 016 (Komet, Lemgo, Germany) (grain size ca. 30–45 μm, conicity ca. 2°); the neighboring teeth were protected by steel-band matrices.
Proximal box finishing in group 2
Proximal box finishing in group 2 was performed with the SF1LM sonic handpiece (Komet, Lemgo, Germany) and with SFD7 000 1 (distal) and SFM7 000 1 (mesial) sonic tips (Komet, Lemgo, Germany) (grain size ca. 60 μm, conicity ca. 8°) on power setting 3 for shaping (amplitude of the free axial oscillation: 180–200 μm) and on power setting 1 for finishing (amplitude of the free axial oscillation: 100–140 μm).
Proximal box finishing in group 3
Proximal box finishing in group 3 was performed with the ultrasonic Sirona Perioscan drive (Sirona Dental GmbH, Wals, Austria), the ultrasound Periosonic handpiece (Sirona Dental GmbH, Wals, Austria), and the SFD7 000 1 (distal) and SFM7 000 1 (mesial) sonic tips (Komet, Lemgo, Germany) (grain size ca. 60 μm, conicity ca. 8°) at 100% power (32 kHz oscillation frequency).
Because the sonic tips on the tooth-facing surface are grainless, the protection of adjacent teeth with the steel band in groups 2 and 3 was not necessary.
In all groups, all sharp edges present inside the cavity were rounded and smoothed with the 8862 314 010 red-ringed diamond flame (Komet, Lemgo, Germany) (grain size ca. 30–45 μm).
Inlay production
The prepared teeth were imprinted with Impregum Penta H Duosoft and Impregum Garant L Duosoft (3M, Seefeld, Germany) using a double mixing technique at room temperature.
Then, the ceramic inlays were conventionally modeled, pressed, adjusted, and completed according to standard laboratory procedures.
Quality control of the ceramic inlays
Prior to cementing, two independent examiners visually inspected the ceramic inlays under a magnifying glass (× 2.5). The entire restoration margin was explicitly controlled in the mesial and distal proximal range. Only clinically acceptable inlays were added to the study. Clinically unacceptable inlays were newly manufactured and controlled again.
Cementation of the ceramic inlays
The basal surface of the ceramic inlay was etched for 20 s with ceramic etching gel that contained 5% hydrofluoric acid IPS (Ivoclar Vivadent AG, Schaan, Liechtenstein), then rinsed for 20 s with the multifunctional syringe, dried and covered for 60 s with the single-component adhesion primer Monobond Plus (Ivoclar Vivadent AG, Schaan, Liechtenstein). Enamel and dentine in the mod-cavity were etched for 30 and 15 s, respectively, with 37% phosphoric acid (Ivoclar Vivadent AG, Schaan, Liechtenstein), then rinsed for 30 s with the multifunctional syringe, dried and covered for 20 s with Universal Adhesive (Ivoclar Vivadent AG, Schaan, Liechtenstein). Adhesive was blown into a uniformly thin film and cured for 10 s with the Satelec Mini Led SP dental curing light (Acteon Germany GmbH, Mettmann, Germany) at a distance of approximately 1 mm. Then, the basal surface of the inlay was covered with the dual-curing luting composite Variolink esthetic DC (Ivoclar Vivadent AG, Schaan, Liechtenstein) and inserted into the mod-cavity with uniform pressure. The excess composite was removed with a foam pellet. Then, the ceramic inlay was kept in the correct position with a Heidemann-spatula under gentle pressure. The inlay was cured for 10 s with the Satelec Mini Led SP dental curing light (Acteon Germany GmbH, Mettmann, Germany) from the occlusal-mesial and occlusal-distal sides at an angle of approximately 45° to the occlusal plane, at a distance of approximately 1 mm from the tooth. To avoid an oxygen-inhibiting layer, the gap between the inlay and the tooth-hard substance before polymerization was covered with a glyceringel liquid strip (Ivoclar Vivadent AG, Schaan, Liechtenstein).
Artificial aging of the ceramic inlays
Immediately after cementation, the teeth (n = 16 from every group) were subjected to thermocycling in the Thermocycler THE1000 (SD Mechatronics, Feldkirchen-Westerham, Germany) with 5000 cycles in water baths at 5 and 55 °C (resistance time 30 s, dripping time 15 s) to simulate hydrothermal stress for the subsequent microleakage and marginal gap examination.
Silver nitrate (AgNO3) penetration
After removal from the thermocycler, the teeth were rinsed with distilled water and dried with a paper towel. The dry teeth were sealed with two layers of Pattex Mini Trio superglue (Henkel AG & Co. KGaA, Dusseldorf, Germany). The basal proximal preparation margin and 0.5 mm circular remained unsealed. After drying for 30 min, the teeth were immersed in AgNO3 (56.62 g/1 L H2O) for 6 h. Subsequently, the teeth were exposed to four illuminants of 100 W for 4 h. After exposure, AgNO3 was developed in liquid Periomat Intra developer (Dürr Dental, Bietigheim-Bissingen, Germany). The depth of silver precipitation was measured in the sections (Fig. 3).
Preparation of sections
All specimens were embedded in Technovit 9100 (Heraeus Kulzer, Werheim, Germany). Then, the specimens were cut in the middle of the sagittal plane through the ceramic inlay with a Leica SP1600 Saw Microtome (Leica Biosystems GmbH, Wetzlar, Germany).
Assessment of surface roughness of the proximal box floor
After preparation and before taking an impression, the surface roughness of each proximal box floor was determined with an Alicona Infinite Focus optical measuring system and Alicona IFM 3.2 computer software (Alicona Imaging GmbH, Raaba/Graz, Austria). In three areas of each proximal box floor, five measurements were taken, and the mean roughness (Ra) was determined.
Assessment of marginal gap
The measurement of the marginal gap as defined by Holmes et al. (1989) of the individual specimens was carried out with a scanning electron microscope (Sigma VP, Carl Zeiss AG, Oberkochen, Germany) in low vacuum mode (VP) at 20 Pa at 20 kV and 500-fold magnification. The marginal gap was measured with the “point-to-point-measure” function of the SmartSEM computer software (Carl Zeiss AG, Oberkochen, Germany). The mesial and distal proximal areas of inlays were investigated with respect to the marginal gap and the absolute marginal discrepancy (aMOP gap) [28]. Since the inlay is suitably contoured, the marginal gap and the absolute marginal discrepancy (MOP gap) are equal—in this case, 98.37 μm (Fig. 4).
Assessment of microleakage
For the measurement of AgNO3 penetration, photographs of the cut samples were taken with a Leica Wild 3ZM stereomicroscope (Leica Camera AG, Wetzlar, Germany). For the computer-assisted measurement of AgNO3 penetration, the images were examined with AutoCAD 2011 computer software (Autodesk GmbH, Munich, Germany). The distance between the extreme point of the preparation edge and the central point of AgNO3 penetration was measured. These measurements were repeated by an additional independent examiner.
Assessment of the ceramic inlay proximal box margin quality
For the evaluation of the ceramic inlay proximal box margin quality, the tooth crowns with the ceramic inlays (n = 4 from every group) were cut into two halves in the bucco-oral direction with a diamond disk, sputtered from the proximal side with gold-palladium and investigated with a scanning electron microscope (Sigma VP, Carl Zeiss AG, Oberkochen, Germany) in high vacuum mode at 20-kV acceleration voltage and the secondary electron detector (SE) at 75-fold magnification. Then, the quality of proximal box margin preparation was visually defined, as seen in Table 1 [9, 29]. Finally, the length of the ceramic inlay proximal box margin sections with the different qualities was measured via SEM (× 75) with the “point-to-point-measure” function of the SmartSEM computer software (Carl Zeiss AG, Oberkochen, Germany).
Statistics
Prior to statistical calculations, the normality of the data was checked using the Kolmogorov-Smirnov test. As the data were not normally distributed, non-parametric tests were applied. For the comparison of group differences, the Mann-Whitney U test was applied. As multiple comparisons were calculated, the Bonferroni correction of the alpha error resulted in a p value of 0.016. Correlations were calculated with the non-parametric Spearman-Rho test. The Statistical Package for Social Sciences program (SPSS, IBM, Amronk, NJ, USA) Vers. 23 was used.
Results
Comparison of the proximal box floor surface roughness after using different proximal box finishing methods
Microscopically qualitative differences in the surface texture were found after preparation with the different instrumental methods (Fig. 5). A significant increase in the surface roughness of the proximal box floor was found in samples that underwent rotating preparation and sonic preparation and ultrasonic preparation (p < 0.001). No significant differences were found in the surface roughness of samples subjected to sonic and ultrasonic preparation (p = 0.016) (Fig. 6).
Comparison of the ceramic inlay proximal microleakage after using the different proximal box finishing methods
No statistically significant differences were found between any of the groups regarding the ceramic inlay proximal microleakage (Fig. 7).
Comparison of the ceramic inlay proximal marginal gap after using different proximal box finishing methods
No statistically significant differences were found between any of the groups regarding proximal marginal gap (Fig. 8).
Comparison of the ceramic inlay proximal absolute marginal gaps after using different proximal box finishing methods
No statistically significant differences were found between any of the groups regarding absolute marginal gap (Fig. 9).
Correlation between microleakage, marginal, and absolute marginal gaps
No statistically significant correlations were found between microleakage and marginal gap (r = − 0.103; p = 0.704), microleakage and absolute marginal gap (r = − 0.024; p = 0.931), or microleakage and roughness (r = − 0.103; p = 0.704) in all three groups.
Quality of the ceramic inlay proximal margin after using different proximal box finishing methods
The distribution of the defined qualities at the ceramic inlay proximal margin was similar in all three groups. Qualities A1 and A2 were most common, and qualities A3 and B were the least common (Fig. 10).
Discussion
The strategies for prolonging the clinical lifetime of esthetic tooth-colored ceramic restorations are timely [21]. A simple, convenient, and safe way to achieve adjacent tooth preparation (finishing) is a major point of interest for clinicians. Different instruments must be used to stabilize and improve the adhesive interface and the overall dental restoration quality [7]. However, their effects on the dentin and enamel surfaces are contradictory [16]. It is known that rotating instruments, compared to sonic and ultrasonic instruments, result in more mod-cavity proximal box border defects, very irregular surfaces [9], and iatrogenic damage to adjacent teeth. Clinically, changes in the marginal quality of ceramic inlays are important because aging (wear) may influence bacterial plaque retention.
Thus, the aim of this in vitro study was to evaluate the marginal quality of the ceramic inlays in human molars after the use of three different instrumental finishing methods. Rotating, sonic, and ultrasonic instruments were used for mod-cavity proximal box finishing in vitro, and their effects on the proximal box floor surface roughness, percentage of continuous margin quality (% of total proximal margin length), microleakage, marginal and absolute marginal gaps after hydrothermal loading (HTL) were assessed. The samples were analyzed via scanning electron microscopy (SEM) and surface roughness analysis.
The data in this study showed a significant increase (p < 0.001) in the surface roughness of the proximal box floor after finishing with the sonic and ultrasonic instruments compared to finishing with the rotating instrument. The quality of the dentin surface has influenced the bond strength of the restauration [30]. Differences in the quality of dentin surface and the bond strength after preparation with different kinds of ultrasonic preparation tips have also been reported [16].
The data of this study also clearly demonstrated that microleakage, marginal, absolute marginal gaps after HTL and proximal marginal quality were not significantly different (p > 0.05) among the three different instrumental finishing methods. No correlations between microleakage, marginal and absolute marginal gaps or between microleakage and surface roughness were found. This is in accordance with the results of Ellis et al. (2012) that the use of ultrasonic instruments for dentin preparation resulted in bond strengths that were comparable to those obtained with the use of diamond burs [16, 28]. Zaruba et al. (2014) concluded that the preparation design of mod-cavities for ceramic inlays does not influence marginal adaption [31]. Hopp et al. (2013) summarized in their review that the preparation design considerations, fabrication methods, and material choice of ceramic inlays do not influence tooth wear [32]. During the analysis of the finishing protocols, some peculiarities for different instrumental methods were determined. The finishing procedure with the sonic and ultrasonic instruments was more simple and convenient for the operator because finishing was performed without the help of the steel-band matrices and was safe for the adjustment of teeth because of the grainless tips.
The limitations of this study are that artificial aging was performed only with HTL, the qualitative lower proximal marginal gap was only evaluated by one investigator, and this evaluation was not compared with the evaluation of another investigator.
Proximal box finishing of mod-cavities in human molars with SI or USI resulted in a higher value of surface roughness than with RI as a result of the coarser grid of the SI and USI. The type of finishing method did not significantly influence microleakage, marginal or absolute marginal gaps, or proximal box marginal quality.
The data showed that SI and USI increased the surface roughness of the proximal boxes and did not increase microleakage or marginal discrepancy of the ceramic inlays. Therefore, the inlay internal fit, and the proximal marginal quality after the proximal box finishing with SI and USI corresponded to the proximal marginal quality after finishing with RI.
The null hypothesis for the present study, that three different finishing methods of the mod-cavities in human molars will not differ in their influence on the surface roughness and border quality of the proximal boxes, microleakage, and marginal gap of the ceramic inlays within enamel, was partly confirmed.
For the proximal box mod-cavity finishing, the use of SI and USI could be an alternative instrumental method to conventional RI methods, with a lower risk of iatrogenic damage of the adjacent teeth. Clinical research is needed to confirm these findings.
Conclusion
Ceramic inlays inserted in mod-cavities with proximal boxes finished with SI und USI result in margins of the same quality as those of inlays placed in the mod-cavity after conventional finishing with RI. The advantage of SI und USI is the reduction in the risk of damaging neighboring teeth in comparison to finishing with RI. Therefore, SI and USI are suitable and harmless to neighboring teeth while proximal boxes are being finished. Finishing with SI and USI for mod ceramic inlays results in a marginal quality that are equal to those of conventional mod ceramic inlay finishing with RI.
References
Bader C, Krejci I (2006) Indications and limitations of Er:YAG laser applications in dentistry. Am J Dent 19(3):178–186
Stappert CF, Ozden U, Att W, Gerds T, Strub JR (2007) Marginal accuracy of press-ceramic veneers influenced by preparation design and fatigue. Am J Dent 20(6):380–384
Seo D, Yi Y, Roh B (2009) The effect of preparation designs on the marginal and internal gaps in Cerec3 partial ceramic crowns. J Dent 37(5):374–382
Clausen JO, Abou Tara M, Kern M (2010) Dynamic fatigue and fracture resistance of non-retentive all-ceramic full-coverage molar restorations. Influence of ceramic material and preparation design. Dent Mater 26(6):533–538
Guess PC, Schultheis S, Wolkewitz M, Zhang Y, Strub JR (2013) Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J Prosthet Dent 110(4):264–273
Zhang Y, Sailer I, Lawn BR (2013) Fatigue of dental ceramics. J Dent 41(12):1135–1147
Rocca GT, Rizcalla N, Krejci I, Dietschi D (2015) Evidence-based concepts and procedures for bonded inlays and onlays. Part II. Guidelines for cavity preparation and restoration fabrication. Int J Esthet Dent 10(3):392–413
Mounajjed R, Layton MD, Azar B (2016) The marginal fit of E.Max press and E.Max CAD lithium disilicate restorations: a critical review. Dent Mater J 35(6):835–844
Hugo BSA, Konopik V, Hotz P, Klaiber B (2000) Die approximale Präparation bei Adhäsivinlays – Vergleich sonoabrasiver und konventioneller Verfahren. Acta Med Dent Helv 5(9):111–118
Lopes RM, Trevelin LT, da Cunha SRB, de Oliveira RF, de Andrade Salgado DMR, de Freitas PM, de Paula Eduardo C, Aranha ACC (2015) Dental adhesion to erbium-lased tooth structure: a review of the literature. Photomed Laser Surg 33(8):393–403
Lussi A (1995) Damage to neighboring teeth during the preparation of proximal cavities. An in-vivo study. Schweiz Monatsschr Zahnmed 105(10):1259–1264
Opdam NJ, Roeters JJ, van Berghem E, Eijsvogels E, Bronkhorst E (2002) Microleakage and damage to adjacent teeth when finishing class II adhesive preparations using either a sonic device or bur. Am J Dent 15(5):317–320
Lenters M, van Amerongen WE, Mandari GJ (2006) Iatrogenic damage to the adjacent surfaces of primary molars, in three different ways of cavity preparation. Eur Arch Paediatr Dent 7(1):6–10
De Moor RJ, Delme KI (2009) Laser-assisted cavity preparation and adhesion to erbium-lased tooth structure: part 1. Laser-assisted cavity preparation. J Adhes Dent 11(6):427–438
De Moor RJ, Delme KI (2010) Laser-assisted cavity preparation and adhesion to erbium-lased tooth structure: part 2. Present-day adhesion to erbium-lased tooth structure in permanent teeth. J Adhes Dent 12(2):91–102
Ellis R, Bennani V, Purton D, Chandler N, Lowe B (2012) The effect of ultrasonic instruments on the quality of preparation margins and bonding to dentin. J Esthet Restor Dent 24(4):278–285
Chen YL, Chang HH, Chiang YC, Lin CP (2013) Application and development of ultrasonics in dentistry. J Formos Med Assoc 112(11):659–665
Mangani F, Marini S, Barabanti N, Preti A, Cerutti A (2015) The success of indirect restorations in posterior teeth: a systematic review of the literature. Minerva Stomatol 64(5):231–240
Mehl A, Kunzelmann KH, Folwaczny M, Hickel R (2004) Stabilization effects of CAD/CAM ceramic restorations in extended MOD cavities. J Adhes Dent 6(3):239–245
LeSage B (2011) Finishing and polishing criteria for minimally invasive composite restorations. Gen Dent 59(6):422–428 quiz 429-30
Muller V, Friedl KH, Friedl K, Hahnel S, Handel G, Lang R (2017) Influence of proximal box elevation technique on marginal integrity of adhesively luted Cerec inlays. Clin Oral Investig 21(2):607–612
Bollen CM, Lambrechts P, Quirynen M (1997) Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater 13(4):258–269
Senawongse P, Pongprueksa P (2007) Surface roughness of nanofill and nanohybrid resin composites after polishing and brushing. J Esthet Restor Dent 19(5):265–273 discussion 274-5
Bashetty K, Joshi S (2010) The effect of one-step and multi-step polishing systems on surface texture of two different resin composites. J Conserv Dent 13(1):34–38
Subramani K, Jung RE, Molenberg A, Hammerle CH (2009) Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants 24(4):616–626
Reshad M (2012) Commentary. The effect of ultrasonic instruments on the quality of preparation margins and bonding to dentin. J Esthet Restor Dent 24(4):286
Ahlers MO, Mörig G, Blunck U, Hajtó J, Pröbster L, Frankenberger R (2009) Guidelines for the preparation of CAD/CAM ceramic inlays and partial crowns. Int J Comput Dent 12(4):309–325
Holmes JR, Bayne SC, Holland GA, Sulik WD (1989) Considerations in measurement of marginal fit. J Prosthet Dent 62(4):405–408
Roulet JF, Reich T, Blunck U, Noack M (1989) Quantitative margin analysis in the scanning electron microscope. Scanning Microsc 3(1):147–158 discussion 158-9
Van Meerbeek B, De Munck J, Mattar D, Van Landuyt K, Lambrechts P (2003) Microtensile bond strengths of an etch&rinse and self-etch adhesive to enamel and dentin as a function of surface treatment. Oper Dent 28(5):647–660
Zaruba M, Kasper R, Kazama R, Wegehaupt FJ, Ender A, Attin T, Mehl A (2014) Marginal adaptation of ceramic and composite inlays in minimally invasive mod cavities. Clin Oral Investig 18(2):579–587
Hopp CD, Land MF (2013) Considerations for ceramic inlays in posterior teeth: a review. Clin Cosmet Investig Dent 5:21–32
Acknowledgements
The authors thank Mrs. S. Haußmann for her technical support, Ivoclar Vivadent AG, Schaan, Liechtenstein and Komet Dental, Lemgo, Germany, for providing the materials.
Funding
The materials for this study were provided by Ivoclar Vivadent AG, Schaan, Liechtenstein and Komet Dental, Lemgo, Germany.
Author information
Authors and Affiliations
Contributions
EAN: wrote the paper.
FS: performed the experiments, measurements, and data assessment.
WHA: supervised the measurements and data assessment (morphological analysis), statistically analyzed the data, and corrected the manuscript.
AP: designed, conceived and planned the experiments, supervised the experimental procedures and the entire project, preformed the final manuscript correction.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Ella A. Naumova declares that she has no conflict of interest.
Fabian Schiml declares that he has no conflict of interest.
Wolfgang. H. Arnold declares that he has no conflict of interest.
Andree Piwowarczyk declares that he has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, informed consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Naumova, E.A., Schiml, F., Arnold, W.H. et al. Marginal quality of ceramic inlays after three different instrumental cavity preparation methods of the proximal boxes. Clin Oral Invest 23, 793–803 (2019). https://doi.org/10.1007/s00784-018-2492-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2492-0