Abstract
Objectives
This study investigated the clinical effectiveness of intervention with an open-mouth exercise device designed to facilitate maximal interincisal opening (MIO) and improve quality of life in patients with head and neck (H&N) cancer and oral submucous fibrosis (OSF).
Materials and methods
Sixty patients with H&N cancer, OSF, and trismus (MIO < 35 mm) participated in the functional rehabilitation program. An open-mouth exercise device intervention group and conventional group, each consisting of 20 patients, underwent a 12-week training and exercising program and follow-up. For the control group, an additional 20 patients were randomly selected to match the demographic characteristics of the aforementioned two groups.
Results
The patients’ MIO improvements in the aforementioned three groups were 14.0, 10.5, and 1.3 mm, respectively.
Conclusion
Results of this study confirm the significant improvement in average mouth-opening range. In addition, according to patient feedback, significant improvements in health-related quality of life and reductions in trismus symptoms occurred in the open-mouth exercise device group.
Clinical relevance
This newly designed open-mouth exercise device can facilitate trismus patients with H&N cancer and OSF and improve mouth-opening range and quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trismus refers to a reduced ability to open the mouth and is a common symptom in patients with head and neck (H&N) cancer and oral submucous fibrosis (OSF). Trismus limits an individual’s mouth-opening range and alters various aspects of health-related quality of life (HRQL) and an individual’s activities of daily life including persistent problems with eating, chewing, swallowing, and oral hygiene. Impaired HRQL subsequently damages patients’ physical and psychological health [1], which in turn can lead to poor nutritional condition and depression; these symptoms have been observed in many previous studies [2].
Previously documented risk factors for cancer-associated trismus include tumor size, high radiotherapy dose, and tumor location, while OSF-related trismus primarily results from mucositis. The mucositis and muscle fibrosis caused by cancer-associated and OSF-related factors both lead to the development of trismus [3,4,5,6].
The definition of trismus (i.e., maximal interincisal opening [MIO] of 35 mm) described by Dijsktra [7] has been used extensively in studies investigating trismus in patients with H&N cancer and those with OSF and was used in the present study. This definition has facilitated the comparison and study of various outcomes in different individuals.
Various devices have been applied in the treatment of oncological- and OSF-related trismus, including passive mouth-opening devices such as tongue depressors or spatulas that are placed between the teeth. Moreover, a rubber hose could provide better mouth opening ability with high patient satisfaction. However, these conventional treatments exposed difficulties in training protocol design, unpredictable outcomes, and lack of patients’ subjective feedback [7]. Recently, the Therabite and Dynasplint (DTS) devices, which are available with a complete set of training protocols, have become increasingly popular in the Western world. With this type of newly designed mouth-opening exercise device, improved outcomes have been reported with better cost-effectiveness than traditional methods [8,9,10].
Thus, currently, there is no consensus on treating trismus related to H&N cancer and OSF. Some patients are encouraged to receive medication, whereas some authorities encourage physical training. Several studies have revealed that open-mouth exercise devices are effective for the treatment of trismus. However, these studies have not used prospective designs or included patient feedback evaluations (PFEs). Therefore, data regarding the outcome of trismus treatment in relation to patients’ experiences and feedback are limited [11].
The present study aimed to investigate the therapeutic effect of the EZBite device and HRQL outcomes in trismus patients with H&N cancer and OSF.
Methods and materials
EZBite
The EZBite device is an open-mouth training device 6.1 × 5.8 × 10 cm in size and weighing 78 g. The device is manufactured from polyvinyl chloride plastic and stainless steel. The strength afforded by occlusal function is 25 kg/cm2 and the operation temperature range is 20–60 °C. The minimal width of the open mouth is 0.5 cm (5 mm). Therefore, the device is limited to trismus patients with open-mouth ranges > 5 mm (Fig. 1). The mechanical action of the device involves passive mouth-opening exercises, and the EZBite is controlled by the patient. Both upper and lower mouthpieces parts are placed between the teeth in maxilla and mandible. The stretching range is 5 mm when the handle of the EZBite is squeezed.
Subjects
All patients with H&N cancer and OSF were recruited from the Tri-Service General Hospital (TSGH, Taipei City, Taiwan) at the multidisciplinary tumor conference held once every 2 weeks. Patients diagnosed with H&N cancer and OSF in 2016 or 2017 were asked to participate in this study.
The inclusion criteria for this study were trismus with OSF and trismus with H&N cancer status post-surgery with or without radiation therapy. Patients with recurrent H&N tumors, poor general health, difficulties with completing questionnaires, and who are edentulous were excluded from this study.
Patients living in Taipei City underwent regular follow-up and detailed clinical evaluations conducted by one oral surgeon from an oral and maxillofacial surgery (OMFS) clinic in TSGH. Those who developed trismus after developing H&N cancer and undergoing OSF treatment were invited to attend an intervention program for the treatment of trismus. In the case of coexisting acute mucositis or painful mouth symptoms, intervention was initiated as early as patients’ oral status allowed. For geographical reasons, only patients living in Taipei City were included in this study. The conventional exercise group and control group were comprised of patients living in Taipei City and matched according to sex, tumor location, tumor stage, comorbidity, radiation dosage, and age.
The patients in this study were divided into three groups. The conventional exercise group and control group followed the standard medical center schedule in Taiwan for follow-up visits according to the local guidelines, which included regular MIO measurements by staff members recruited from an OMFS of TSGH. A structured intervention program was introduced to the participants during the time of trismus occurrence in each of the three groups. The EZBite device was used specifically for improving mouth-opening performance in the EZBite exercise group.
Trismus intervention
The exercise program was a 12-week structured exercise program involving exercise nine times per day. The program consisted of the following three steps: (1) warm up movements, namely jaw opening ten times and small sideway movements of the jaws ten times without using the jaw device; (2) passive stretching with the jaw-mobilizing device and conventional mouth devices such as a tongue depressor for 30 s (if possible), to be repeated five times; and (3) five repetitions of active exercise (bite toward resistance). Patients were instructed to relax between each session and to gradually increase the amount and intensity of the exercises to avoid pain or injury. During the program, the patients were evaluated by an oral surgeon who conducted MIO measurements after 12 weeks after intervention commencement.
The patients in control group of this study were selected from patients originally in the other two groups, who did not comply with instructions. The patients received written and oral instructions and the EZBite device was demonstrated to the patients by an oral surgeon (Fig. 2).
Endpoints and assessment
The primary endpoint in this study was MIO. The secondary endpoint was a questionnaire surveying trismus-related symptoms and HRQL before and after treatment. A multidimensional study protocol was used to evaluate functional outcomes before and after the trismus exercise program. The protocol included MIO, weight, height, sociodemographic data, treatment regimens, and tumor classification. TNM classification and tumor staging results were retrieved according to the system of classification determined by the National Comprehensive Cancer Network of the USA.
MIO
The criterion for trismus (MIO < 35 mm), suggested by Dijsktra et al. [7], was used. MIO scores were measured using a ruler with the patient in an upright position. MIO was measured as the maximal distance between the edges of the incisors of the mandible and the maxilla and expressed in mm.
PFE
The Gothenburg Trismus Questionnaire (GTQ) is a newly developed and validated symptom-specific trismus questionnaire. The GTQ has been well accepted by patients, has satisfactory compliance with low rates of missing items, and has exhibited good psychometric properties (validity and reliability). The questionnaire design modified the acceptable items of the GTQ, which contains 12 items divided into three domains, namely jaw-related problems (four items), eating limitations (four items), and muscular tension (two items), and two additional items that were retained as single items. The domains and single items were scored within a range of 0–100, in which 100 indicates the maximal number of symptoms and 0 indicates the absence of symptoms.
Statistical methods
Because of the small sample size in the present study, the Kruskal-Wallis test was applied to examine the correlation between and statistical significance of differences among the groups. All tests were conducted at 5% significance level.
Results
Patient characteristics
In total, 60 patients were identified, of whom 48 had trismus related to H&N cancer and 12 had trismus not related to cancer. Twenty-four patients with trismus related to H&N cancer were referred to the Department of Radiation Oncology for further radiation therapy. No data regarding MIO before treatment was available for these patients. Patient characteristics, diagnosis, and tumor localization are summarized in Table 1.
Twenty patients with trismus were enrolled in this study and allocated to the EZBite group, with another 20 enrolled in the conventional group. An additional 20 patients were enrolled during the same period as a control group. Except for the latter 20 patients, all patients completed the intervention program. In the EZBite group, the patients received treatment for trismus with the EZBite device. The patients in the conventional group used a conventional jaw-opening device with a tongue depressor or rubber hose. Due to difficulties in complying with instructions, the 20 patients in the control group used their own methods of manual stretching during the training course. No patients in the control group used the EZBite device or conventional jaw-opening device (Table 1).
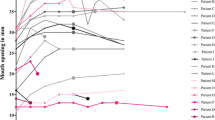
MIO
The EZBite group had higher mean MIO outcomes than the conventional and control groups and with differences that were statistically significant. At the end of the intervention, the mean MIO improvements were 14.0 mm in the EZBite group, 10.5 mm in the conventional group, and 1.3 mm in the control group. Changes in MIO before and after treatment with the EZBite are presented in Table 2.
However, patients who could not comply with the treatment recommendations, grouping in the control group, did not demonstrate significant improvement (pretreatment to post-treatment MIO, 14.2–15.5 mm; p = 0.88). No complications were reported during treatment with the EZBite.
PFE
A questionnaire to evaluate the improvement in participant HRQL was designed. The questionnaire included 12 items, with 10 items divided into three domains: jaw-related problems (4 items), eating limitations (4 items), and muscular tension (2 items). The remaining two items were retained as single items. The domains and single items range from 0 to 100, in which 100 refers to maximal amount of symptoms and 0 indicates the complete absence of symptoms.
The results revealed improvement in the participants’ HRQL, including those related to jaw-related problems, eating limitations, muscle tension, jaw limitations, and social activity, which were reflected in the patients’ PFEs based on the score improvements in the questionnaire.
Before the intervention, there were no significant differences in the questionnaire scores between the three groups. At the end of the treatment period, the scores contained significant differences between the groups in all three domains (jaw-related problems, eating limitations, and muscular tension) and two single items, indicating a significant decrease in trismus-related symptoms in the EZBite group (Table 3). It is especially important to note that improvement in social activity resulted in the restoration of the patients’ inter-social relationships. Moreover, this result supported our post-treatment expectations, rather than simply an increase in MIO.
Discussion
Previous studies have demonstrated improvements in mouth-opening range after jaw exercise in patients with H&N cancer and trismus. Three retrospective studies found evidence that jaw-mobilizing devices, such as the Therabite® device and Dynasplint System®, are effective for the treatment of trismus [6,7,8]. However, to our knowledge, few prospective studies have investigated the impact and influences of exercise-based treatment on patients with H&N cancer and trismus. In addition, various measurement methods and experimental designs have rendered results diverse and difficult for analyzing further outcomes. We are devoted to developing accurate experimental designs and conducting comprehensive result analyses, and we look forward to conducting further studies. Despite the limited sample size in this study, we attempted to surpass the results of previous retrospective studies.
We found the greatest improvement in the EZBite group, including that of MIO from 15.7 to 29.7 mm and various increases in aspects of HRQL based on quantitative evaluations of the GTQ scores. Compared with the improvement of 6.4 mm achieved using the Therabite system in the previous studies, the EZBite training device demonstrated a greater capability for inducing MIO improvement.
Reduction in the increased MIO was a major problem after completion of the mouth-opening training program. Aspects of the treatment modality of MIO improvement remain controversial. For example, physical therapy is generally considered to be the mainstay of trismus treatment and is often used independently or in combination with other modalities. However, according to several studies, treatment choices and outcomes remain limited after the occurrence of relapse [9,10,11]. Because of the case selection time, we did not record the relapse conditions of our participants. We still believe that these are major problems in maintaining positive treatment outcomes. We intend to perform further investigations to examine how to maintain positive outcomes.
We should mention that healthy anterior dentition was noted in all of our participants, without the appearance of periodontitis or partial edentulous anterior dentition. In addition, these patients are not suitable for this device given the difficulties in manipulation and higher risks to teeth and for soft tissue trauma. Further consideration should be given when recommending the device [12].
The present investigation was designed as a pilot study to further explore the efficacy of the EZBite device as part of a multimodal treatment strategy for reducing trismus. However, we used measurements of participants’ passive mouth opening rather than active mouth opening to acquire objective data. In our opinion, data from active mouth opening and further long-term follow-up will better reflect the real-life situations of patients’ long-term HRQL. Therefore, further evaluation of the possibility of relapse should be a focus in further studies. Other difficulties include short-arm force, which causes hand manipulation difficulties according to our participants. Further ergonomic correction should be considered in future studies [13].
Our study had two main advantages: first, the participants’ MIO and HRQL significantly improved after using the EZBite device and second is the cost-effective characteristics of our device, which is available to patients at a price five times lower than that of the Therabite device. Thus, we intend to encourage more patients to use the EZBite device to achieve more positive treatment experiences and outcomes.
Our study had several limitations, including selection bias and a small sample size. In the future, we hope to adopt a longer tracing time to further examine the relationship between relapse and our treatment design.
Conclusion
Regular rehabilitation and adequate device assistance facilitate the maintenance of an increased MIO and increased HRQL among patients with H&N cancer and trismus. We intend to conduct further investigations and develop new treatment regimens in subsequent studies.
References
Weber C, Dommerich S, Pau HW, Kramp B (2010) Limited mouth opening after primary therapy of head and neck cancer. Oral Maxillofac Surg 14:169–173. https://doi.org/10.1007/s10006-010-0220-2
Lee R, Slevin N, Musgrove B, Swindell R, Molassiotis A (2012) Prediction of post-treatment trismus in head and neck cancer patients. Br J Oral Maxillofac Surg 50:328–332. https://doi.org/10.1016/j.bjoms.2011.06.009
Sharma M, Radhakrishnan R (2017) Limited mouth opening in oral submucous fibrosis: reasons, ramifications, and remedies. J Oral Pathol Med 46:424–430. https://doi.org/10.1111/jop.12513
Louise Kent M, Brennan MT, Noll JL, Fox PC, Burri SH, Hunter JC, Lockhart PB (2008) Radiation-induced trismus in head and neck cancer patients. Support Care Cancer 16:305–309
Pauli N, Fagerberg-Mohlin B, Andréll P, Finizia C (2014) Exercise intervention for the treatment of trismus in head and neck cancer. Acta Oncol 53:502–509. https://doi.org/10.3109/0284186X.2013.837583
Pauli N, Johnson J, Finizia C, Andrell P (2013) The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncol 52:1137–1145. https://doi.org/10.3109/0284186X.2012.744466
Dijkstra PU, Huisman PM, Roodenburg JL (2006) Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg 35:337–342
Stubblefield MD, Manfield L, Riedel ER (2010) A preliminary report on the efficacy of a dynamic jaw opening device (dynasplint trismus system) as part of the multimodal treatment of trismus in patients with head and neck cancer. Arch Phys Med Rehabil 91:1278–1282. https://doi.org/10.1016/j.apmr.2010.05.010
Baranano CF, Rosenthal EL, Morgan BA, McColloch NL, Magnuson JS (2011) Dynasplint for the management of trismus after treatment of upper aerodigestive tract cancer: a retrospective study. Ear Nose Throat J 90:584–590
Kamstra JI, Roodenburg JL, Beurskens CH, Reintsema H, Dijkstra PU (2013) TheraBite exercises to treat trismus secondary to head and neck cancer. Support Care Cancer 21:951–957. https://doi.org/10.1007/s00520-012-1610-9
Dijkstra PU, Sterken MW, Pater R, Spijkervet FK, Roodenburg JL (2007) Exercise therapy for trismus in head and neck cancer. Oral Oncol 43:389–394
Grandi G, Silva ML, Streit C, Wagner JC (2007) A mobilization regimen to prevent mandibular hypomobility in irradiated patients: an analysis and comparison of two techniques. Med Oral Patol Oral Cir Bucal 12:E105–E109
Buchbinder D, Currivan RB, Kaplan AJ, Urken ML (1993) Mobilization regimens for the prevention of jaw hypomobility in the radiated patient: a comparison of three techniques. J Oral Maxillofac Surg 51:863–867
Acknowledgments
This study was supported by The Megaforce Company, Taipei, Taiwan, R.O.C.
Funding
Tri-Service General Hospital (TSGH-C106-004-006-008-S05)
Tri-Service General Hospital (TSGH-C107-008-S06)
Ministry of National Defense, Taiwan (MAB-106-090)
National Science Council, Taiwan, Republic of China (MOST 105-2314-B-016-021-MY3)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Li, YH., Chang, WC., Chiang, TE. et al. Mouth-opening device as a treatment modality in trismus patients with head and neck cancer and oral submucous fibrosis: a prospective study. Clin Oral Invest 23, 469–476 (2019). https://doi.org/10.1007/s00784-018-2456-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2456-4