Abstract
Objectives
The aim of the present study was the evaluation of the effectiveness and efficiency of two plaque-removing techniques, plastic curettes (PC) and glycine powder airflow (GLY) in combination with taurolidine (T), chlorhexidine (CHX), or pure water (PW) as additives and compared to groups without previous treatment (NT).
Materials and methods
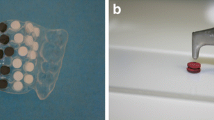
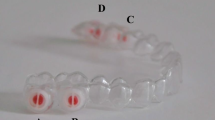
Plaque was collected on titanium samples for 48 h in six subjects. Specimens were worn in a special splint in the upper jaw and randomly assigned to test and control groups. After biofilm removal procedures, clean implant surface (CIS) on the samples and treatment time were taken as parameters.
Results
Mean CIS was determined in the following descending order: T-GLY > CHX-GLY > NT-GLY > T-PC > PW-GLY > PW-PC > CHX-PC > NT-PC. Mean treatment time was determined in the following ascending order: T-GLY < CHX-GLY < PW-GLY < NT-GLY < T-PC < CHX-PC < PW-PC < NT-PC.
Conclusions
Within the limits of this study, it can be concluded that T showed the highest CIS in the GLY and PC groups. T-GLY showed significantly more CIS than all other GLY groups. The T-PC group showed significantly more CIS than all other PC groups. The treatment times of the T groups were significantly lower than their corresponding PC or GLY groups.
Clinical relevance
The results of the current study indicate that taurolidine seems to enhance effectiveness of plaque-removing procedures with plastic curettes and glycine powder airflow. Also, the efficiency of both treatment procedures seems to be increased.






Similar content being viewed by others
References
Klokkevold PR, Newman MG (2000) Current status of dental implants: a periodontal prospective. Int J Oral Maxillofac Implants 15:56–65
Lekholm U, Adell R, Eriksson B, Brånemark PI, Jemt T (1990) Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants 5:347–359
Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, van Steenberghe D (1999) Survival rate of Branemark implants in partially edentulous jaws: a 10 year study. Int J Oral Maxillofac Implants 69:639–645
Renvert S, Polyzois I, Maguire R (2009) Re-osseointegration on previously contaminated surfaces: a systematic review. Clin Oral Implants Res 20(4):216–227
Zitzmann NU, Berglundh T (2008) Definition and prevalence of peri-implant diseases. J Clin Periodontol 35(8):286–291
Berglundh T, Gotfredsen K, Zitzmann NU, Lang NP, Lindhe J (2007) Spontaneous progression of ligature induced peri-implantitis at implants with different surface roughness: an experimental study in dogs. Clin Oral Implants Res 18(5):655–661
Heitz-Mayfield LJ (2008) Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 35(8):292–304
Schwarz F, Ferrari D, Popovski K, Hartig B, Becker J (2009) Influence of different air-abrasive powders on cell viability at biologically contaminated titanium dental implants surfaces. J Biomed Mater Res B Appl Biomater 88(1):83–91
Berglundh T, Lindhe J, Marinello C, Ericsson I, Liljenberg B (1992) Soft tissue reaction to de novo plaque formation on implants and teeth. An experimental study in the dog. Clin Oral Implants Res 3(1):1–8
Zitzmann NU, Berglundh T, Marinello CP, Lindhe J (2001) Experimental peri-implant mucositis in man. J Clin Periodontol 28(6):517–523
Fürst M, Salvi GE, Lang NP, Persson GR (2007) Bacterial colonization immediately after installation on oral titanium implants. Clin Oral Implants Res 18:501–508
Salvi GE, Fürst MM, Lang NP, Persson GR (2008) One-year bacterial colonization patterns of Staphylococcus aureus and other bacteria at implants and adjacent teeth. Clin Oral Implants Res 19:242–248
Esposito M, Hirsch J, Lekholm U, Thomsen P (1999) Differential diagnosis and treatment strategies for biologic complications and failing oral implants: a review of the literature. Int J Oral Maxillofac Implants 14:473–490
Quirynen M, De Soete M, van Steenberghe D (2002) Infectious risks for oral implants: a review of the literature. Clin Oral Implants Res 13:1–19
Leonhardt A, Dahlén G, Renvert S (2003) Five year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol 74:1415–1422
Renvert S, Lessem J, Dahlén G, Renvert H, Lindahl C (2008) Mechanical and repeated antimicrobial therapy using a local drug delivery system in the treatment of peri-implantitis: a randomized clinical trial. J Periodontol 5:836–844
Fox SC, Moriarty JD, Kusy RP (1990) The effects of scaling a titanium implant surface with metal and plastic instruments: an in vitro study. J Periodontol 61(8):485–490
Augthun M, Tinschert J, Huber A (1998) In vitro studies on the effect of cleaning methods on different implant surfaces. J Periodontol 69(8):857–864
Kreisler M, Kohnen W, Christoffers AB, Gotz H, Jansen B, Duschner H, d’Hoedt B (2005) In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er:YAG laser and an air powder system. Clin Oral Implants Res 16(1):36–43
Sahrmann P, Ronay V, Hofer D, Attin T, Jung RE, Schmidlin PR (2013) In vitro cleaning potential of three different implant debridement methods. Clin Oral Implants Res. doi: 10.1111/clr.12322
Cochis A, Fini M, Carrassi A, Migliario M, Visai L, Rimondini L (2013) Effect of air polishing with glycine powder on titanium abutment surfaces. Clin Oral Implants Res 24(8):904–909
Jones CG (1997) Chlorhexidine: is it still the gold standard? Periodontol 2000(15):55–62
Arweiler NB, Boehnke N, Sculean A, Hellwig E, Auschill TM (2006) Differences in efficacy of two commercial 0.2 % chlorhexidine mouthrinse solutions: a 4-day plaque re-growth study. J Clin Periodontol 33:334–339
Flötra L, Gjermo P, Rölla G, Waerhaug J (1972) A 4-month study on the effect of chlorhexidine mouthwashes on 50 soldiers. Scand J Dent Res 80:10–17
Schaupp H, Wohnaut H (1978) Disturbances of taste from oral disinfectants. HNO 26:335–341
Wilken R, Botha SJ, Grobler A, Germishuys PJ (2001) In vitro cytotoxicity of chlorhexidine gluconate, benzydamine-HCl and povidone iodine mouthrinses on human gingival fibroblasts. SADJ 56:455–460
Bhandari M, Adili A, Schemitsch EH (2001) The efficacy of low-pressure lavage with different irrigating solutions to remove adherent bacteria from bone. J Bone Joint Surg Am 83:412–419
Schuller-Levis GB, Park E (2003) Taurine: new implications for an old amino acid. FEMS Microbiol Lett 226:195–202
Erb F, Febvay N, Imbenotte M (1982) Structural investigation of a new organic antiseptic: taurolidine : a spectroscopic study of its stability and equilibria in various solvents. Talanta 29:953–958
Browne MK, Leslie GB, Pfirrmann RW (1976) Taurolin, a new chemotherapeutic agent. J Appl Bacteriol 41:363–368
Baker DM, Jones JA, Nguyen-Van-Tam JS, Lloyd JH, Morris DL, Bourke JB, Steele RJ, Hardcastle JD (1994) Taurolidine peritoneal lavage as prophylaxis against infection after elective colorectal surgery. Br J Surg 81:1054–1056
Simon A, Ammann RA, Wiszniewsky G, Bode U, Fleischhack G, Besuden MM (2008) Taurolidine-citrate lock solution (TauroLock) significantly reduces CVAD-associated grampositive infections in pediatric cancer patients. BMC Infect Dis 8:102
Koldehoff M, Zakrzewski JL (2004) Taurolidine is effective in the treatment of central venous catheter-related bloodstream infections in cancer patients. Int J Antimicrob Agents 24:491–495
Eick S, Radakovic S, Pfister W, Nietzsche S, Sculean A (2012) Efficacy of taurolidine against periodontopathic species—an in vitro study. Clin Oral Investig 16(3):735–744
Arweiler NB, Auschill TM, Sculean A (2012) Antibacterial effect of taurolidine (2%) on established dental plaque biofilm. Clin Oral Investig 16(2):499–504
John G, Becker J, Schwarz F (2014) Effects of taurolidine and chlorhexidine on SaOS-2 cells and human gingival fibroblasts grown on implant surfaces. Int J Oral Maxillofac Implants 29(3):728–34
Rodan SB, Imai Y, Thiede MA, Wesolowski G, Thompson D, Bar-Shavit Z, Shull S, Mann K, Rodan GA (1987) Characterization of a human osteosarcoma cell line (Saos-2) with osteoblastic properties. Cancer Res 47(18):4961–4966
Auschill TM, Arweiler NB, Netuschil L, Brecx M, Reich E, Sculean A, Artweiler NB (2001) Spatial distribution of vital and dead microorganisms in dental biofilms. Arch Oral Biol 46:471–476
Hahn R, Netuschil L, Löst C (1992) Initiale Plaquebesiedlung auf keramischen Restaurationsmaterialien. Dtsch Zahnärztl Z 47:330–334
Schwarz F, Sculean A, Romanos G, Herten M, Horn N, Scherbaum W, Becker J (2005) Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clin Oral Investig 9:111–117
John G, Becker J, Schwarz F (2013) Rotating titanium brush for plaque removal from rough titanium surfaces - an in vitro study. Clin Oral Implants Res 25(7):838–42. doi: 10.1111/clr.12147
Rimondini L, Fare S, Brambilla E, Felloni A, Consonni C, Brossa F, Carrassi A (1997) The effect of surface roughness on early in vivo plaque colonization on titanium. J Periodontol 68:556–562
Schwarz F, Papanicolau P, Rothamel D, Beck B, Herten M, Becker J (2006) Influence of plaque biofilm removal on reestablishment of the biocompatibility of contaminated titanium surfaces. J Biomed Mater Res A 77:437–444
Schwarz F, Nuesry E, Bieling K, Herten M, Becker J (2006) Influence of an erbium, chromium-doped yttrium, scandium, gallium, and garnet (Er, Cr:YSGG) laser on the reestablishment of the biocompatibility of contaminated titanium implant surfaces. J Periodontol 77:1820–1827
Siegrist BE, Brecx MC, Gusberti FA, Joss A, Lang NP (1991) In vivo early human dental plaque formation on different supporting substances. A scanning electron microscopic and bacteriological study. Clin Oral Implants Res 2:38–46
Schroeder HE (1965) Crystal morphology and gross structures of mineralizing plaque and of calculus. Helv Odontol Acta 35:73–86
Quirynen M, van der Mei HC, Bollen CM, Schotte A, Marechal M, Doornbusch GI, Naert I, Busscher HJ, van Steenberghe D (1993) An in vivo study of the influence of the surface roughness of implants on the microbiology of supra- and subgingival plaque. J Dent Res 72:1304–1309
Rams TE, Roberts TW, Tatum H Jr, Keyes PH (1984) The subgingival microbial flora associated with human dental implants. J Prosthet Dent 51:529–534
Maehara Y, Anai H, Tamada R, Sugimachi K (1987) The ATP assay is more sensitive than the succinate dehydrogenase inhibition test for predicting cell viability. Eur J Cancer Clin Oncol 23:273–276
Ahmad M, McCarthy MB, Gronowicz G (1999) An in vitro model for mineralization of human osteoblast-like cells on implant materials. Biomaterials 20:211–220
Crouch SP, Kozlowski R, Slater KJ, Fletcher J (1993) The use of ATP bioluminescence as a measure of cell proliferation and cytotoxicity. J Immunol Methods 160:81–88
Petty RD, Sutherland LA, Hunter EM, Cree IA (1995) Comparison of MTT and ATP-based assays for the measurement of viable cell number. J Biolumin Chemilumin 10:29–34
Sennerby L, Lekholm U (1993) The soft tissue response to titanium abutments retrieved from humans and reimplanted in rats. A light microscopic study. Clin Oral Implants Res 4:23–27
Mengel R, Buns CE, Mengel C, Flores-de-Jacoby L (1998) An in vitro study of the treatment of implant surfaces with different instruments. Int J Oral Maxillofac Implants 13:91–96
Funding
The study was, in part, funded by Geistlich Pharma AG, Wolhusen, Switzerland.
Conflict of interest
The authors declare that they have no conflict of interests related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
John, G., Schwarz, F. & Becker, J. Taurolidine as an effective and biocompatible additive for plaque-removing techniques on implant surfaces. Clin Oral Invest 19, 1069–1077 (2015). https://doi.org/10.1007/s00784-014-1337-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1337-8