Abstract
Purpose
Postpartum depression (PPD) and anxiety (PPA) affect nearly one-quarter (23%) of women in Canada. eHealth is a promising solution for increasing access to postpartum mental healthcare. However, a user-centered approach is not routinely taken in the development of web-enabled resources, leaving postpartum women out of critical decision-making processes. This study aimed to evaluate the effectiveness, usability, and user satisfaction of PostpartumCare.ca, a web-enabled psychoeducational resource for PPD and PPA, created in partnership with postpartum women in British Columbia.
Methods
Participants were randomized to either an intervention group (n = 52) receiving access to PostpartumCare.ca for four weeks, or to a waitlist control group (n = 51). Measures evaluating PPD (Edinburgh Postnatal Depression Scale) and PPA symptoms (Perinatal Anxiety Screening Scale) were completed at baseline, after four weeks, and after a two-week follow-up. User ratings of website usability and satisfaction and website metrics were also collected.
Results
PPD and PPA symptoms were significantly reduced for the intervention group only after four weeks, with improvements maintained after a two-week follow-up, corresponding with small-to-medium effect sizes (PPD: partial η2 = 0.03; PPA: partial η2 = 0.04). Intervention participants were also more likely than waitlist controls to recover from clinical levels of PPD symptoms (χ 2 (1, n = 63) = 4.58, p = .032) and PostpartumCare.ca’s usability and satisfaction were rated favourably overall.
Conclusion
Findings suggest that a web-enabled psychoeducational resource, created in collaboration with patient partners, can effectively reduce PPD and PPA symptoms, supporting its potential use as a low-barrier option for postpartum women.
Trial Registration
Protocol for this trial was preregistered on NIH U.S. National Library of Medicine, ClinicalTrials.gov as of May 2022 (ID No. NCT05382884).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postpartum Depression (PPD) is a leading cause of maternal morbidity and mortality (Oates 2003). In 2019, Statistics Canada reported that PPD symptoms affect 10% of Canadian women, while an additional 8% experience comorbid PPD and postpartum anxiety (PPA) symptoms, and another 5% experience symptoms of PPA only (Government of Canada 2019).
Untreated PPD and PPA can severely impact a parent’s mental and physical health, offspring cognitive and motor development, and the overall wellbeing of a family unit (Agnafors et al. 2013; Brummelte and Galea 2016; Fitelson et al. 2010). Given the impacts of postpartum mental illness, effective strategies for prevention, management, and treatment are critical (Zhou et al. 2022).
Current best practice guidelines for perinatal mental healthcare within British Columbia (BC) recommend treatment based on symptom severity (Williams et al. 2014) with nonpharmacological interventions (e.g., psychotherapy, psychoeducation) being recommended as first-line options before considering pharmacological treatment for mild-to-moderate cases, and combination (psychological and pharmacological) in more severe cases (Cuijpers et al. 2023; Donker et al. 2009; Williams et al. 2014).
Despite these existing effective options, barriers reduce access to these supports (Button et al. 2017; Jones 2019). Key barriers impacting help-seeking include social stigma, financial constraints, insufficient education and awareness, and logistical issues with attending in-person appointments (Button et al. 2017; Jones 2019).
eHealth involves the translation of health interventions from traditional in-person provision to delivery via telephone, mobile application, or web-enabled platforms and is a promising solution for increasing access to mental healthcare (Enam et al. 2018; Eysenbach 2001; Zhao et al. 2021). Previously, eHealth interventions have been developed and assessed to effectively reduce symptoms of PPD and PPA (Lee et al. 2016; Milgrom et al. 2016; Ngai et al. 2015; O’Mahen et al. 2014; Pugh et al. 2016; Wozney et al. 2017; Zhao et al. 2021).
A user-centered design approach involves an iterative process of incorporating end-user input at each stage of eHealth intervention development (Still and Crane 2017; User-Centered Design Basics 2017). This approach establishes the importance of understanding the identity and voice of end-users and involving them early on and regularly to design relevant and valuable resources (Still and Crane 2017; User-Centered Design Basics 2017). According to the standards for evaluating eHealth interventions, the conceptualization and design phases are key points of evaluation (Eng 1999), yet many eHealth interventions do not involve patient partners’ voices throughout, and instead only include them at the end of the study (Enam et al. 2018).
Although existing eHealth interventions for postpartum mental health have been successful in reducing symptoms of mental illness, few have taken a true user-centered approach by involving patient voices in the conceptualization and design of these platforms. For example, O’Mahen et al. (2014) utilized feedback from a qualitative study assessing women’s preferences for a perinatal CBT program when developing content for an internet behavioural-activation-based treatment for PPD, However, this feedback was not specific to the delivery of this program via eHealth and, therefore, user preferences associated with using technology for the delivery of the intervention may have been missed. As well, Pugh et al. (2016) evaluated the efficacy of internet-based CBT program for PPD and assessed qualitative feedback from users of their program and identified areas for improvement, but the intervention itself appears to have been conceptualized and designed by researchers only, without input from the intended user group, PPD patients. To address this gap in the literature, there is a need for research that follows a user-centered approach by involving patient partners in the initial eHealth development processes to create an intervention that best addresses the needs, values, and preferences of those facing postpartum mental illness.
This study is the third phase of a research project with the goal of developing an effective and accessible web-enabled psychoeducational resource for individuals in BC, Canada, experiencing postpartum mental health concerns. Phase One identified the unmet needs of those experiencing postpartum mental illness and investigated how a web-enabled intervention could meet these needs, including specific content and features desired (Lackie et al. 2021). Lackie et al. (2021) pointed out that many of the existing eHealth interventions for postpartum mental health relied primarily on delivering psychotherapy via technology (e.g., delivering Cognitive Behavioural Therapy (CBT) or Behavioural Activation adapted to online platforms) which may not address some of the key unmet needs of women identified within the study such as the provision of education using evidence-based information to address the lack of knowledge surrounding perinatal mental illness, a resource hub for accessing relevant support services, and information on self-care and peer support. Therefore, authors concluded that a web-enabled psychoeducational intervention would be best suited to address the unmet needs of women in BC.
Phase Two designed the psychoeducational web-enabled resource for postpartum mental health, PostpartumCare.ca, guided by a multidisciplinary advisory committee of patient partners, mental health clinicians, researchers, and community organization partners with firsthand expertise addressing perinatal mental illness. Phase Two also involved a feasibility study to collect user feedback regarding visual layout, content, and overall website satisfaction (Siddhpuria et al. 2022). This feedback was incorporated in the website design, guided by the web development advisory committee.
The objective of the current Phase Three randomized controlled trial was to evaluate the effectiveness, usability, and user satisfaction of PostpartumCare.ca. Effectiveness was evaluated using primary outcomes of PPD and PPA symptoms. Implementation outcomes included user ratings of website usability and satisfaction and website metrics collected to gain an understanding of participant usage patterns. We hypothesized that: (1) following a four-week usage period of PostpartumCare.ca, intervention participants would see a greater reduction in depression and anxiety symptoms compared to waitlist control participants and that this would be maintained after a two-week follow-up period. (2) We also expected that PostpartumCare.ca would be rated favourably by intervention participants according to implementation outcome measures of usability and satisfaction.
Materials and methods
Inclusion/exclusion criteria
Participants were required to be 19 years of age or older, have given birth within the past 12 months, reside in BC, have occasional or regular access to the internet (via computer, smartphone, tablet, etc.), be able to communicate in English (i.e., be able to read, write, and speak conversational English), and be experiencing symptoms of postpartum depression and/or anxiety as per the EPDS for depression (receive a score ≥ 9), and the Perinatal Anxiety Screening Scale (PASS) for anxiety (receive a score ≥ 26) (Cox et al. 1987; Somerville et al. 2014).
Recruitment
Protocol for this trial was preregistered on NIH U.S. National Library of Medicine, ClinicalTrials.gov as of May 2022 (ID No. NCT05382884). Research Ethics approval for this study was obtained from the University of British Columbia and the BC Children’s and Women’s Hospital Research Ethics Board (REB number: H21-01379)). Participants were recruited primarily online, through advertisements posted on social media pages.
Power and sample size
Sample size was determined for a two-way mixed ANOVA with two groups and three times of assessment using G*Power software (version 3.1) with a goal of detecting a small-to-medium effect using a significance level α = 0.05 and a minimum power of 80%. With these parameters, the recommended total sample size was N = 74. Considering an expected attrition rate of 20%, we aimed to enroll a minimum of 93 participants.
Procedures
Data were collected from June 2022 through April 2023. Enrolled participants were randomly allocated to either the intervention or waitlist control group by simple randomization using a random number generator (0 – waitlist control, 1 – intervention). Participants were not notified of their group allocation, instead they were only notified via email of when their start date would be for website access.
Each arm of the study was six weeks in length and participants in both groups completed online questionnaires evaluating PPD and PPA symptoms at three time points: (T1) at baseline, prior to the intervention/waitlist control period; (T2) after a four-week intervention/waitlist control period; and (T3) after a two-week follow-up period. At T2, intervention participants completed an additional questionnaire assessing website usability and satisfaction and their website metrics were collected. In cases where five consecutive unsuccessful contact attempts were made to remind participants to complete questionnaires, the participant was deemed lost to follow-up.
Description of the intervention/waitlist control conditions
Participants in the intervention group received access to PostpartumCare.ca immediately following the completion of T1 questionnaires for a period of four weeks. Waitlist control participants received website access after T3, following all data collection.
PostpartumCare.ca is composed of a main landing page containing tabs for three website sections: Education, Resources, and Supports, as well as a separate Mood/Anxiety Tracker section (Table 1; Fig. 1). The Education, Resources, and Supports sections contain didactic text related to PPD and PPA, links to local BC and remote (online/phone) support services, and information on social supports and self-care practices, respectively. The Mood/Anxiety Tracker section permits users to sign in and input mood and/or anxiety symptoms to track symptom changes over time. Users can select either a “Mood” or “Anxiety” tab and are prompted to rate their mood (i.e., how you feel most of the day, over the past week) on a sliding scale from 0 to 10, with higher scores indicating better mood, and/or their anxiety symptoms (i.e., how anxious you feel most of the day, over the past week) on a sliding scale from 0 to 10, with higher scores indicating less anxiety. For each entry, users are also given options to click on specific symptoms experienced (e.g., losing interest in favourite activities, losing ability to concentrate, feeling guilty or worthless, etc.) and/or write an extra note in an open textbox before submitting their entry. Once submitted, users can click on a “Graphs” tab to see their mood/anxiety ratings plotted over time (e.g., over 3 days, 7 days, 14 days, or 30 days) or on a “Resources” tab for links to resources provided based on specific symptoms entered. All website sections also contained links to outsources (e.g., other websites/resources) relevant to the material within each section.
PostpartumCare.ca was made to be accessible on any computer, tablet, or smartphone device to allow for use on any personal devices (e.g., smartphones or laptops) or public devices (e.g., library computers). Prior to receiving access, intervention participants were notified of all website sections, given a brief description of their contents, and given four weeks to use the website as often/in whatever capacity desired with the knowledge that they would be asked to complete online questionnaires evaluating their experience using the website after this four-week period. No additional instructions or reminders for website use were given. Having participants use the website as desired (i.e., without specific time and/or frequency requirements) was intended to reflect what realistic use of the website might be for BC’s postpartum population in accordance with principles of effectiveness/pragmatic trials (Kim 2013).
Measures
Demographics
Demographic information was obtained through an investigator-derived self-report questionnaire (see Table 2 for demographic variables collected).
PPD symptoms
PPD symptoms were measured using the Edinburgh Postnatal Depression Scale (EPDS), a reliable and valid 10-item self-report measure used internationally to evaluate PPD symptoms (Cox et al. 1987). To avoid false negatives and include participants who might meet PPD diagnostic criteria (i.e., scores indicating possible depression), an EPDS score ≥ 9 was used as an inclusion criterion (Levis et al. 2020; Williams et al. 2014). Cronbach’s alpha for the present sample was high (α = 0.85) (DeVellis 2003; Kline 2005).
PPA symptoms
PPA symptoms were measured using the Perinatal Anxiety Screening Scale (PASS), a reliable and valid 31-item self-report measure for anxiety screening in perinatal populations (Somerville et al. 2014). The recommended cut-off score of ≥ 26 for differentiating high and low risk of presenting with an anxiety disorder was used as an inclusion criterion (Somerville et al. 2014). Cronbach’s alpha for the present sample was high (α = 0.94) (DeVellis 2003; Kline 2005).
Website Usability and Satisfaction: A brief three-question Patient Global Impression of Change (PGIC) questionnaire was adapted for this study based on the measure developed by Hurst and Bolton (2004) to assess (1) perceived improvement of PPD and/or PPA symptoms; (2) perceived improvements in overall quality of life; and (3) overall satisfaction towards the intervention. The System Usability Scale (SUS) was used to evaluate usability parameters such as website ease of use, complexity, and function integration (Brooke 1995). The Patient Education Materials Assessment Tool (PEMAT) was used to evaluate the understandability and actionability of website patient education materials (Shoemaker et al. 2014). The User-Perceived Web Quality Instrument (UPWQI) was used to measure four dimensions of perceived web quality: technical adequacy, content quality, specific content, and appearance (Aladwani and Palvia 2002).
Website metrics
Website metrics were collected using Matomo Analytics to describe how participants used PostpartumCare.ca and included average number of page visits per participant, average time spent visiting each section per session (in minutes), total number of pageviews, and most visited outsources per website section. Data were available for the entire sample (not individual).
Data analysis
Data were analyzed following intention-to-treat (ITT) principles. Independent t-tests were conducted for all continuous variables and chi-square tests were conducted for all categorical variables to compare the randomized groups at baseline. To evaluate primary outcomes, two-way mixed ANOVAs with one between-subject factor (group: intervention, waitlist control) and one within-subject factor (time of assessment: T1, T2, T3) were conducted. Results of participant demographic questionnaires and implementation outcome measures were reported descriptively.
Calculating clinical significance
Clinically significant improvement was assessed for both primary outcomes. For PPD, clinically significant change on the EPDS was calculated according to procedures outlined by Matthey (2004). Participants who saw both a reliable score decrease of four or more points and cut-off change from > 12 to ≤ 12 from T1 to T3 were classified as “recovered” from PPD (Matthey 2004). Clinically significant improvement for PPA was defined as a change in PASS total scores from ≥ 26 to < 26 from T1 to T3 (Somerville et al. 2014). Chi-square tests were conducted to determine if there was an association between group and clinically significant improvement for PPD and PPA.
Results
Participants
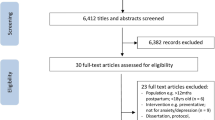
Of 317 initially assessed, N = 103 met inclusion criteria and provided consent (Figs. 2, 3, 4). Following randomization, 101 completed T1 questionnaires, 95 completed T2 questionnaires, and 92 completed T3 questionnaires and were included in analyses for primary outcomes (intervention: n = 45, waitlist control: n = 47). From randomization to T3, 11 participants were lost to follow-up as they did not respond to reminders prompting questionnaire completion, resulting in a 10.7% attrition rate, which was lower than the anticipated 20% attrition rate. There were no additional reasons provided for study discontinuation, so we deemed these as “lost to follow-up”. All participants (N = 103) were included in demographic characteristic analyses. All participants who completed T1 questionnaires (n = 101) were included in analyses of baseline PPD/PPA symptoms and all intervention participants who completed T2 questionnaires (n = 47) were included in analyses for implementation outcomes.
Although participants of any gender were eligible for inclusion, all participants self-identified as cisgender women so we refer to our sample as “women” from here o. Analyses comparing demographic variables at T1 revealed a significant difference in age and education levels such that waitlist control participant were significantly older and more educated than intervention participants (Table 2). Waitlist control participants (M = 34.25, SD = 4.84) were significantly older than intervention participants (M = 31.60, SD = 5.12), t(2) = 2.71, p = .008. Waitlist control participants (M = 17.64, SD = 4.84) attended significantly more years of school compared to intervention participants (M = 16.06, SD = 3.16), t(97) = 2.62, p = .010, and had attained higher education levels, χ 2(6, N = 103) = 12.81, p = .046. To factor in the significant group differences in age and education at baseline, the interaction of time and group was also tested using ANCOVA with age and education as covariates. The results of ANCOVA produced the same pattern of significant interaction and time main effects for both primary outcomes and there were no significant interactions between time and covariates. Therefore, the originally planned ANOVA results are reported without age and education included.
Primary outcome analyses
On the first primary outcome of PPD symptoms (EPDS total score), there was a significant main effect of time with scores decreasing over time, F(2,180) = 11.22, p < .001, partial η2 = 0.11, indicating a medium-to-large effect size, and a significant main effect of group favouring the intervention group F(1, 90) = 5.40, p = .022, partial η2 = .06, indicating a medium effect size (Table 3). Main effects were qualified by a significant interaction between group and time, F(2, 180) = 3.12, p = .046, partial η2 = 0.03, indicating a small-to-medium effect size (Adams and Conway 1966). Post-hoc pairwise-comparisons revealed a significant mean difference from T1 to T2 (MD = 2.85, SE = 0.65, p < .001), with the effect remaining significant at T3 (MD = 2.96, SE = 0.73, p < .001) for the intervention group only. For the waitlist control group, the mean difference from T1 to T2 did not reach significance (MD = 0.62, SE = 0.63, p = .327), and the effect remained non-significant at T3 (MD = 1.20, SE = 0.71, p = .096).
On the co-primary outcome of PPA symptoms (PASS total score), there was a significant main effect of time with scores decreasing over time, F(2,178) = 11.12, p < .001, partial η2 = 0.11, indicating a medium-to-large effect size, and a significant main effect of group favouring the intervention group F(1, 89) = 5.92, p = .017, partial η2 = 0.06, indicating a medium effect size (Table 3). Main effects were qualified by a significant interaction between group and time, F(2, 178) = 3.79, p = .024, partial η2 = 0.04, indicating a small-to-medium effect size (Adams and Conway 1966). Post-hoc pairwise-comparison tests for the interaction effect revealed a significant mean difference from T1 to T2 (MD = 7.42, SE = 1.74, p < .001), with the effect remaining significant at T3 (MD = 8.07, SE = 1.89, p < .001) for the intervention group only. For the waitlist control group, the mean difference from T1 to T2 was non-significant (MD = 1.33, SE = 1.68, p = .430), and the effect remained non-significant at T3 (MD = 2.64, SE = 1.83, p = .148) .
Clinical significance
For PPD, a chi-square test showed a significant relationship between group and PPD recovery, such that a greater proportion of participants recovered in the intervention group χ 2 (1, n = 63) = 4.58, p = .032 (Table 4). For PPA, although there were more that improved in the intervention group (n = 10, 27%) compared to the waitlist control group (n = 5, 11.9%) at T3, there was no statistically significant association between clinically significant PPA improvement and group, χ 2 (1, n = 79) = 2.92, p = .087 (Table 5).
Implementation outcome analyses
Patient global impression of change (PGIC)
Intervention participants (n = 47) provided ratings on three questions adapted from the PGIC. On the first question evaluating perceived improvement in PPD and/or PPA symptoms following the use of PostpartumCare.ca, the mean rating was 3.74, SD = 0.94. On the second question evaluating perceived improvements in overall quality of life, participants’ mean rating was 3.06, SD = 0.73. The final question rated overall satisfaction towards PostpartumCare.ca and the mean score was 5.56, SD = 2.05 (Table 6).
System usability scale (SUS)
Intervention participants (n = 47) rated the system usability of PostpartumCare.ca as about average overall (M = 67.29, SD = 21.15) (Table 6), given that an SUS score ≥ 68 indicates above average website usability (Bangor 2009).
Patient education materials assessment tool (PEMAT)
On average, intervention participants (n = 45) rated website understandability at 85.23%, SD = 20.63. Similarly, intervention women (n = 45) rated the website as 84.07% actionable on average, SD = 23.56 (Table 6).
User-perceived web quality index (UPWQI)
Intervention participants (n = 47) rated agreement with the website’s technical adequacy as M = 5.17, SD = 1.04. Agreement with PostpartumCare’s content quality was rated as M = 5.27, SD = 1.32, and specific content was rated as M = 4.97, SD = 1.15. Finally, agreement with website appearance was rated as M = 5.31, SD = 1.40 (Table 6).
Website metrics
Website metrics for the intervention group (n = 47) were collected according to website section (Education, Supports, Resources, Mood/Anxiety Tracker) at T2 (see Table 7). Of the 47 participants who completed T2 questionnaires, 4 did not access the website during the study period but were still included in analyses for website metrics.
In total, the website was accessed 113 times, an average of 2.40 (SD = 1.90) times per participant. The Education section was visited an average of 1.06 times per participant, for an average time of 48 min per session and received 56 total page views. The Supports section was visited an average of 0.93 times per participant for an average time of 37 min per session and received 49 total page views. The Resources section was visited an average of 0.23 times per participant for an average time of 106 min per session and received 12 total page views. The Mood/Anxiety Tracker was visited an average of 1.02 times per participant for an average time of 33 min and received 82 total page views. The number of Mood/Anxiety Tracker entries per participant ranged from 0 to 6 total entries within the four-week study period. The most viewed outsources per section are reported in Table 7.
Discussion
Principal findings
Results showed that engagement with PostpartumCare.ca significantly reduced symptoms of PPD and PPA after four weeks in the intervention group only, with improvements maintained after a two-week follow-up. These improvements were associated with small-to-medium effect sizes, and clinical significance outcomes showed intervention participants to be more likely to recover from PPD. Website usability and satisfaction were rated favourably overall by intervention participants. Global patient impression of change scores indicated a small-to-moderate perceived improvement in depression and anxiety symptoms, a small improvement in perceived overall quality of life, and slightly above average overall satisfaction with the intervention with scores falling in the middle range. System usability was rated as average overall, understandability and actionability were highly rated, and women generally agreed with the website’s technical adequacy, content quality, specific content, and appearance.
Website metrics also provided some insights as to how PostpartumCare.ca may be used. Intervention participants viewed most sections about once on average and spent anywhere from 33 to 106 min on each section per session, suggesting that website visits may be somewhat infrequent, but of considerable duration.
Web-enabled psychoeducational resource can improve symptoms of PPD and PPA
These findings build upon previous research indicating that psychoeducational interventions can be effective for reducing symptoms of depression and anxiety in various patient populations and may be a valuable first-line intervention for those experiencing psychological distress (Al-Alawi et al. 2022; Chan et al. 2019; Donker et al. 2009; Williams et al. 2014). Further, our study found evidence of the effectiveness of a psychoeducational resource for mental health delivered via eHealth and applied to a sample of postpartum women.
Although psychoeducational interventions are known to serve purposes such as education and prevention, research also suggests that psychoeducation can be effective for reducing symptoms of psychological disorders including depression and anxiety and are generally less expensive, less time-consuming, more easily administered, and potentially more accessible than other psychotherapeutic interventions (Donker et al. 2009). This may be particularly relevant for those facing postpartum mental health challenges considering the added time and financial constraints associated with postpartum and early parenthood (Button et al. 2017; Jones 2019).
Previous literature investigating eHealth interventions for the prevention and treatment of PPD and PPA have largely focused on interventions that incorporated a direct psychotherapeutic component, often centered on CBT or Behavioural Activation principles (Saddichha et al. 2014). However, the body of literature investigating the effects of eHealth-delivered psychoeducational resources without direct psychotherapeutic components for reducing postpartum mental illness is limited, and existing studies have shown mixed results. One study found a reduction in PPD symptoms following the use of a smartphone-based psychoeducational intervention in first time mothers, but reductions in anxiety symptoms were not significant (Chan et al. 2019). Another study found no significant difference in PPD symptoms between intervention and control groups following the use of a psychoeducational mobile-health application, and PPA was not evaluated (Shorey et al. 2017). Our findings suggest that psychoeducational content delivered online can be effective for reducing symptoms of PPD and PPA. Because they are informational in nature, the specific content delivered may be key in influencing the effectiveness of an intervention (Donker et al. 2009). Of note, both interventions from Chan et al. (2019) and Shorey et al. (2017) provided information related to general parenting rather than tailored to perinatal mental health disorders. The effectiveness of the current intervention may be attributed to women responding favourably to psychoeducational material specific to their underlying mental health disorder(s). Future research should therefore continue to investigate the effectiveness of web-enabled psychoeducational tools for postpartum mental health to further understand what types of information provide the most benefit to those in need of support.
User perceptions of postpartumCare.ca
Following use of PostpartumCare.ca, participants on average perceived small-to-moderate improvements in depression and anxiety symptoms and a small improvement in overall quality of life. User feedback was positive regarding the website’s actionability and understandability, and towards specific website aspects such as technical adequacy, content quality, and appearance. These findings are in agreement with previous results from a pilot study of a prototype of the current intervention where the website’s layout, language, and content were found to be generally easy to understand, clear, trustworthy, and helpful by nearly all participants (Siddhpuria et al. 2022). However, on measures that assessed overall satisfaction and system usability, our results fell in the middle range, around average. This finding differs slightly from Siddhpuria et al. (2022), where most participants were either somewhat or very satisfied with the website protypes. A possible explanation for the more modest satisfaction ratings in the current study may be reflected in the website metrics of participants, as some key aspects of the site may not have been accessed to their fullest potential. Most pages were viewed an average of one time per participant. Because of this infrequent usage pattern, participants may not have been able to fully utilize website features intended for repeated usage such as the Mood/Anxiety Tracker, which was intended to allow participants to create entries on a more regular basis to track mood and anxiety symptoms over time. However, this study did not collect direct participant feedback related to usability and satisfaction of individual website sections (i.e., Education, Resources, Supports, Mood/Anxiety Tracker) and therefore, it is difficult to confirm how satisfaction ratings might have been related to participant experiences with individual website sections/features. As such, specific reasons as to why features such as the Mood/Anxiety Tracker were not utilized as frequently as initially intended are unclear. Despite this, when considering all measures of website usability and satisfaction together, the website was reviewed favorably overall by participants in this study, evidencing its potential usefulness for women.
Clinical implications
Women with clinical levels of PPD who used PostpartumCare.ca were more likely than controls to recover from PPD. This finding, along with the statistically significant improvements in symptoms, suggest our web-enabled resource may be helpful for the alleviation of clinical PPD symptoms. These findings, though, are difficult to confirm without the use of gold-standard methods for evaluating clinical PPD/PPA diagnosis (i.e., diagnostic interviews based on DSM-5 criteria). Therefore, future research employing gold-standard diagnostic methods is suggested to better understand the effect of a web-enabled psychoeducational tool on clinical PPD and PPA symptom recovery.
Limitations and strengths
This study does have some limitations. First, the demographic homogeneity of our sample (e.g., all cisgender women, mostly White, educated, heterosexual, with relatively high income) may limit the generalizability of our findings to the greater BC population. Second, this study lacks longer-term follow-ups beyond two weeks after engaging with PostpartumCare.ca, thus limiting our understanding of the potential long-term impact of the intervention on symptoms of PPD/PPA. Finally, this study did not collect qualitative participant feedback on website utilization (i.e., investigating why participants spent more/less time on certain pages). Therefore, specific reasons as to why certain sections were utilized more/less by each participant are unclear.
Despite these limitations, our study had notable strengths. To our knowledge this is the first study to evaluate a web-enabled psychoeducational intervention specific to the needs of women in BC affected by postpartum mental illness and that was developed according to principles of user-centered design (Canadian Institutes of Health Research 2011; Still and Crane 2017; User-Centered Design Basics 2017). Few published studies evaluating digital postpartum mental health resources have incorporated the same degree of iterative patient engagement, utilizing user feedback at each stage of intervention development and assessment (Chan et al. 2019; Fealy et al. 2019; Haga et al. 2013; O’Mahen et al. 2014; Pugh et al. 2016; Shorey et al. 2017). Considering the increasing reliance on web-enabled resources in many health domains, patient engagement should be prioritized given its feasibility and benefits for intended populations. Second, this study had relatively low attrition compared to similar studies in the field (Chan et al. 2019; Dennis et al. 2020). Finally, our intervention addressed both PPD and PPA, setting it apart from many existing resources that target depression only (Loughnan et al. 2019).
Conclusions and future directions
Our findings suggest that four-week usage of a web-enabled psychoeducational intervention for postpartum mental health is effective for reducing symptoms of PPD and PPA among women in BC. As a follow-up to the current trial, a future knowledge translation phase will seek to develop mobilization strategies for implementing PostpartumCare.ca as a practical tool for women in BC.
References
Agnafors S, Sydsjö G, Dekeyser L, Svedin CG (2013) Symptoms of depression postpartum and 12 years later-associations to child mental health at 12 years of age. Matern Child Health J 17(3):405–414. https://doi.org/10.1007/s10995-012-0985-z
Al-Alawi KS, Al-Azri M, Al-Fahdi A, Chan MF (2022) Effect of Psycho-Educational intervention to reduce anxiety and depression at Postintervention and Follow-Up in women with breast Cancer: a systematic review and Meta-analysis. Semin Oncol Nurs 38(6):151315. https://doi.org/10.1016/j.soncn.2022.151315
Aladwani AM, Palvia PC (2002) Developing and validating an instrument for measuring user-perceived web quality. Inf Manag 39(6):467–476. https://doi.org/10.1016/S0378-7206(01)00113-6
Brooke J (1995) SUS: a quick and dirty usability scale. Usability Eval Ind. 189
Brummelte S, Galea LAM (2016) Postpartum depression: etiology, treatment and consequences for maternal care. Horm Behav 77:153–166. https://doi.org/10.1016/j.yhbeh.2015.08.008
Button S, Thornton A, Lee S, Shakespeare J, Ayers S (2017) Seeking help for perinatal psychological distress: a meta-synthesis of women’s experiences. Br J Gen Pract 67(663):692–699. https://doi.org/10.3399/bjgp17X692549
Canadian Institutes of Health Research (2011) Canada’s Strategy for Patient-Oriented Research. Government of Canada. https://cihr-irsc.gc.ca/e/44000.html
Chan KL, Leung WC, Tiwari A, Or KL, Ip P (2019) Using smartphone-based psychoeducation to reduce postnatal Depression among First-Time mothers: Randomized Controlled Trial. JMIR MHealth UHealth 7(5):12794. https://doi.org/10.2196/12794
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry: J Mental Sci 150:782–786. https://doi.org/10.1192/bjp.150.6.782
Cuijpers P, Franco P, Ciharova M, Miguel C, Segre L, Quero S, Karyotaki E (2023) Psychological treatment of perinatal depression: a meta-analysis. Psychol Med 53(6):2596–2608. https://doi.org/10.1017/S0033291721004529
Dennis CL, Grigoriadis S, Zupancic J, Kiss A, Ravitz P (2020) Telephone-based nurse-delivered interpersonal psychotherapy for postpartum depression: Nationwide randomised controlled trial. Br J Psychiatry 216(4):189–196. https://doi.org/10.1192/bjp.2019.275
DeVellis RF (2003) Scale Development: theory and applications. SAGE
Donker T, Griffiths KM, Cuijpers P, Christensen H (2009) Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Med 7(1):79. https://doi.org/10.1186/1741-7015-7-79
Enam A, Torres-Bonilla J, Eriksson H (2018) Evidence-based evaluation of eHealth interventions: systematic literature review. J Med Internet Res 20(11):10971. https://doi.org/10.2196/10971
Eng T (1999) Introduction to evaluation of interactive health communication applications. Am J Prev Med 16(1):10–15. https://doi.org/10.1016/S0749-3797(98)00107-X
Eysenbach G (2001) What is e-health? J Med Internet Res 3(2):833. https://doi.org/10.2196/jmir.3.2.e20
Fealy S, Chan S, Wynne O, Dowse E, Ebert L, Ho R, Zhang MWB, Jones D (2019) The support for New Mums Project: a protocol for a pilot randomized controlled trial designed to test a postnatal psychoeducation smartphone application. J Adv Nurs 75(6):1347–1359. https://doi.org/10.1111/jan.13971
Fitelson E, Kim S, Baker AS, Leight K (2010) Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Women’s Health 3:1–14. https://doi.org/10.2147/IJWH.S6938
Government of Canada (2019) Maternal Mental Health in Canada. https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2019041-eng.htm
Haga SM, Drozd F, Brendryen H, Slinning K (2013) Mamma Mia: a feasibility study of a web-based intervention to reduce the risk of Postpartum Depression and enhance subjective well-being. JMIR Res Protocols 2(2):29. https://doi.org/10.2196/resprot.2659
Hurst H, Bolton J (2004) Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manip Physiol Ther 27(1):26–35. https://doi.org/10.1016/j.jmpt.2003.11.003
Jones A (2019) Help seeking in the Perinatal period: a review of barriers and facilitators. Social Work Public Health 34(7):596–605. https://doi.org/10.1080/19371918.2019.1635947
Kim SY (2013) Efficacy versus effectiveness. Korean J Family Med 34(4):227. https://doi.org/10.4082/kjfm.2013.34.4.227
Kline RB (2005) Principles and Practice of Structural Equation Modeling, Second Edition. Guilford Publications
Lackie ME, Parrilla JS, Lavery BM, Kennedy AL, Ryan D, Shulman B, Brotto LA (2021) Digital Health needs of women with Postpartum Depression: Focus Group Study. J Med Internet Res 23(1):18934. https://doi.org/10.2196/18934
Lee EW, Denison FC, Hor K, Reynolds RM (2016) Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth 16:38. https://doi.org/10.1186/s12884-016-0831-1
Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD (2020) Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. https://doi.org/10.1136/bmj.m4022. BMJ m4022
Loughnan SA, Joubert AE, Grierson A, Andrews G, Newby JM (2019) Internet-delivered psychological interventions for clinical anxiety and depression in perinatal women: a systematic review and meta-analysis. Archives Women’s Mental Health 22(6):737–750. https://doi.org/10.1007/s00737-019-00961-9
Matthey S (2004) Calculating clinically significant change in postnatal depression studies using the Edinburgh postnatal depression scale. J Affect Disord 78(3):269–272. https://doi.org/10.1016/S0165-0327(02)00313-0
Milgrom J, Danaher BG, Gemmill AW, Holt C, Holt CJ, Seeley JR, Tyler MS, Ross J, Ericksen J (2016) Internet cognitive behavioral therapy for women with postnatal depression: a Randomized Controlled Trial of MumMoodBooster. J Med Internet Res 18(3):e54. https://doi.org/10.2196/jmir.4993
Ngai FW, Wong PWC, Leung KY, Chau PH, Chung KF (2015) The Effect of Telephone-based cognitive-behavioral therapy on postnatal depression: a Randomized Controlled Trial. Psychother Psychosom 84(5):294–303. https://doi.org/10.1159/000430449
O’Mahen HA, Richards DA, Woodford J, Wilkinson E, McGinley J, Taylor RS, Warren FC (2014) Netmums: a phase II randomized controlled trial of a guided internet behavioural activation treatment for postpartum depression. Psychol Med 44(8):1675–1689. https://doi.org/10.1017/S0033291713002092
Oates M (2003) Perinatal psychiatric disorders: a leading cause of maternal morbidity and mortality. Br Med Bull 67:219–229. https://doi.org/10.1093/bmb/ldg011
Pugh NE, Hadjistavropoulos HD, Dirkse D (2016) A randomised controlled trial of Therapist-Assisted, internet-delivered cognitive behavior therapy for women with maternal depression. PLoS ONE 11(3):e0149186. https://doi.org/10.1371/journal.pone.0149186
Saddichha S, Al-Desouki M, Lamia A, Linden IA, Krausz M (2014) Online interventions for depression and anxiety—A systematic review. Health Psychol Behav Med 2(1):841–881. https://doi.org/10.1080/21642850.2014.945934
Shoemaker SJ, Wolf MS, Brach C (2014) Development of the Patient Education materials Assessment Tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns 96(3):395–403. https://doi.org/10.1016/j.pec.2014.05.027
Shorey S, Lau YY, Dennis CL, Chan YS, Tam WWS, Chan YH (2017) A randomized-controlled trial to examine the effectiveness of the ‘Home-but not alone’ mobile-health application educational programme on parental outcomes. J Adv Nurs 73(9):2103–2117. https://doi.org/10.1111/jan.13293
Siddhpuria S, Breau G, Lackie ME, Lavery BM, Ryan D, Shulman B, Kennedy AL, Brotto LA (2022) Women’s preferences and design recommendations for a Postpartum Depression psychoeducation intervention: user involvement study. JMIR Formative Res 6(6):e33411. https://doi.org/10.2196/33411
Somerville S, Dedman K, Hagan R, Oxnam E, Wettinger M, Byrne S, Coo S, Doherty D, Page AC (2014) The perinatal anxiety screening scale: development and preliminary validation. Archives Women’s Mental Health 17(5):443–454. https://doi.org/10.1007/s00737-014-0425-8
Still B, Crane K (2017) Fundamentals of user-centered design: a practical Approach. CRC
User-Centered Design Basics (2017) US Department of Health and Human Services. https://www.usability.gov/what-and-why/user-centered-design.html
Williams J, Ryan D, Thomas-Peter K, Cadario B, Li D (2014) Best Practice Guidelines for Mental Health Disorders in the Perinatal Period. BC Reproductive Mental Health Program
Wozney L, Olthuis J, Lingley-Pottie P, McGrath PJ, Chaplin W, Elgar F, Cheney B, Huguet A, Turner K, Kennedy J (2017) Strongest Families™ managing our Mood (MOM): a randomized controlled trial of a distance intervention for women with postpartum depression. Archives Women’s Mental Health 20(4):525–537. https://doi.org/10.1007/s00737-017-0732-y
Zhao L, Chen J, Lan L, Deng N, Liao Y, Yue L, Chen I, Wen SW, Xie R (2021) Effectiveness of Telehealth interventions for Women with Postpartum Depression: systematic review and Meta-analysis. JMIR MHealth UHealth 9(10):e32544. https://doi.org/10.2196/32544
Zhou C, Hu H, Wang C, Zhu Z, Feng G, Xue J, Yang Z (2022) The effectiveness of mHealth interventions on postpartum depression: a systematic review and meta-analysis. J Telemed Telecare 28(2):83–95. https://doi.org/10.1177/1357633X20917816
Acknowledgements
We would like to acknowledge funding received in support of this research by The Diamond Foundation, the Gillespie Family Foundation, and the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All study procedures were approved and carried out in accordance with the guidelines set by the University of British Columbia and BC Children’s and Women’s Hospital Research Ethics Board (REB number: H21-01379).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors report no competing financial or non-financial interests that are directly or indirectly related to the work submitted for this publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lawrence, C.G., Breau, G., Yang, L. et al. Effectiveness of a web-enabled psychoeducational resource for postpartum depression and anxiety among women in British Columbia. Arch Womens Ment Health (2024). https://doi.org/10.1007/s00737-024-01468-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00737-024-01468-8