Abstract
Emerging data suggest that certain adverse childhood experiences (ACEs) are associated with perinatal depression (PND). However, few studies have comprehensively assessed the cumulative number and types of ACEs and their association to PND. We conducted a cross-sectional analysis among 16,831 female participants from the Stress-And-Gene-Analysis (SAGA) cohort in Iceland, 2018. ACEs were surveyed with the World Health Organization ACE—International questionnaire, while PND symptoms were assessed using the Edinburgh Postnatal Depression Scale (lifetime version). We, while adjusting for confounding factors, estimated the prevalence ratio (PR) of PND in relation to total number of ACEs using the Poisson quasi-likelihood model and further performed analyses for type-specific ACEs. At a mean age of 44 years (SD ± 11.1), 6,201 (36.8%) participants had experienced probable PND. Total number of ACEs was positively associated with PND (PR 1.11 per ACE, 95% CI: 1.10–1.11), also among women without any psychiatric comorbidities (PR 1.13, 95% CI: 1.11–1.14). PRs increased in a dose–response manner with the number of ACEs (P for trend < 0.001); women that endorsed 5 or more ACEs were twice as likely to have experienced PND (PR 2.24, 95% CI: 2.09–2.41). All ACE types (n = 13) were associated with PND, with most pronounced association for emotional neglect by a guardian (PR 1.53, 95% CI: 1.47–1.59). Our findings suggest a positive association between number of ACEs and PND symptoms. If our results are confirmed with prospective data, healthcare providers need to be alert of the risk of PND among expecting mothers with history of ACEs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perinatal depression (PND) affects about 10–20% of pregnant/postpartum women (Woody et al. 2017) with non-negligible influences on both mothers and their families. For instance, women with PND have a higher incidence of preterm delivery, preeclampsia, and suicide; and their children are more likely to have low birth weight, and decreased social, cognitive, and emotional development (Van Niel and Payne 2020). However, few modifiable risk factors have been identified for prevention, except exposure to abusive partners (Gastaldon et al. 2022; Yang K et al. 2022a).
Adverse childhood experiences (ACEs) are traumatic events that occur in childhood (e.g., emotional and physical abuse or neglect and growing up in dysfunctional home environments) and can harm the child’s development and health through changes in the development of the nervous, endocrine, and immune systems under distress (Hughes et al. 2017). Research data support that ACEs might operate through psychobiological pathways leading to PND (Choi and Sikkema 2016). Indeed, previous studies have revealed an association between selected ACEs, e.g., childhood maltreatment, and perinatal mood disorders, especially PND (Osofsky et al. 2021; Racine et al. 2021; Rich-Edwards et al. 2011). However, few studies have made a comprehensive assessment of the different types of adverse events and situations a child can be exposed to (LeMasters et al. 2021; McDonnell and Valentino 2016; Menke et al. 2019; Osofsky et al. 2021). For instance, some subtypes, such as bullying, have not been investigated in relation to PND. Moreover, most studies have focused on any ACEs (Mersky and Janczewski 2018; Miller et al. 2021; Racine et al. 2020; Wajid et al. 2020), and it remains unclear what subtypes of ACEs are most strongly associated with PND. In addition, ACEs are associated with a range of psychiatric disorders in adulthood (Chapman et al. 2004; McKay et al. 2021; Tebeka et al. 2021), and a history of psychiatric disorders predisposes mothers to PND (Guintivano et al. 2018). However, few studies (Tebeka et al. 2021) have taken into account the role of psychiatric comorbidities in the association between ACEs and PND.
Leveraging a large population-representative cohort of females in Iceland, this study aimed to comprehensively examine whether women with any out of 13 different types of ACEs were more likely to experience depressive symptoms during their pregnancy and/or postpartum. We also aimed to identify high-risk subtypes of ACEs most strongly associated to PND and illustrate any risk modification by comorbidity of psychiatric disorders.
Materials and methods
Sample characteristics and study design
We conducted a cross-sectional analysis with data from the Stress-And-Gene-Analysis (SAGA) cohort in Iceland, which is representative of the Icelandic female population in terms of demographic characteristics, including age, education, income, and geographic location (Daníelsdóttir et al. 2022). In March 2018, all women aged 18–69 years and living in Iceland were invited to participate in the study by filling in an electronic questionnaire regarding trauma history and current health status. Among 30,372 women who consented to participate (corresponding to approximately 30% of eligible women in Iceland), we identified and included 22,651 women who had given a live birth (Fig. 1). Among them, we excluded 2,064 women due to missing information on PND assessment on more than two items and 3,756 women due to missing information on the ACEs questionnaire. In the end, 16,831 women were included in the analysis (Fig. 1).
Assessment of PND
Perinatal depressive symptoms were measured using the Edinburgh Perinatal Depression Scale (EPDS) (Cox et al. 1987)—lifetime version (Meltzer-Brody et al. 2013). The EPDS is a ten-item self-reported screening tool for depressive symptoms during pregnancy and/or postpartum and has been proven to have good specificity and sensitivity in other Nordic populations (Eberhard-Gran et al. 2001; SBU 2012). Each item is scored on a scale rangeing from 0 to 3, giving a total score of 30, with higher score reflecting more severe symptoms. The lifetime version of EPDS starts with two screening questions asking if the participant (1) ever felt depressed during pregnancy and (2) ever felt depressed within 6 months after giving birth. Women who answer “yes” to either screening question receive the 10 following questions from the original EPDS to assess the lifetime prevalence of PND, asking for the worst period during pregnancy or after childbirth experienced. For women with missing data on either one or two items, the individual mean value was used for imputation. In accordance with previous studies (Rubertsson et al. 2011), a clinical cut-off of ≥ 13 was used to indicate probable PND. We further divided the women with PND into antenatal, postnatal, and persistent (both antenatal and postnatal) depression according to the first two screening questions, and two additional questions asking for when the symptoms started during pregnancy and when they started postpartum. If depressed both during pregnancy and after childbirth, women were classified as persistent.
Assessment of ACEs
A modified Icelandic version of the World Health Organization (WHO) ACEs – International questionnaire (IQ) was used to assess ACEs. This widely adopted questionnaire consisted of 39 items on 13 types of ACEs and has been qualitatively tested in six culturally diverse settings (Rutter 2021; WHO 2018). The 13 types included can be grouped into four catergories including abuse (physical, emotional, and sexual abuse), neglect (physical and emotional neglect), household dysfunction (domestic violence, lost of a parent or parental separation, household substance abuse, incarcerated household member, mental illness in the household), and violence (community violence, bullying, and collective violence). Exposure to war or collective violence is extremely rare in Iceland. Consequently, the Icelandic ACE-IQ was modified by adding one screening question on collective violence. As described elsewhere (Daníelsdóttir et al. 2022; Yang Q et al. 2022b), the exposure of each type of ACE was defined according to the Guidance of Analyzing ACE-IQ (frequency version) provided by WHO (WHO 2018). We then calculated the total numbers of ACEs (0–13) for analysis.
Covariates
Potential confounders included age at time of survey and experience of childhood economic deprivation. To assess the latter, participants were asked “Was your family’s economic situation ever so bad that you suffered any deprivation as a consequence? For example, this could apply to deprivation of nutritious food and/or deprivation of warm clothes and appropriate footwear during the winter months.” We also obtained information on highest educational level, employment status, marital status, and monthly income, surveyed at recruitment, as a proxy for socioeconomic status over the lifetime.
Potential mediators, including parity, age at menarche, and current body mass index (BMI) (derived via self-reported height and weight), were assessed through questions at the recruitment. ACEs has been associated with obesity, whereas pre-pregnancy BMI has been associated with PND (Dachew et al. 2021; Hughes et al. 2017).
Lastly, psychiatric comorbidities including attention deficit hyperactivity disorder (ADHD), autism, schizophrenia, severe depression, bipolar disorder, panic disorder, agoraphobia, social phobia, body dysmorphic disorder, obsessive–compulsive disorder (OCD), specific phobia, general anxiety disorder, adjustment disorder, post-traumatic stress disorder (PTSD), eating disorder (e.g., anorexia nervosa or bulimia nervosa), sleeping disorder, personality disorder, and substance abuse disorder were all collected via self-reports. Current perceived social support was assessed using the Multidimensional Scale of Perceived Social Support (MSPSS), a 12-item questionnaire with scores ranging from 0 to 84, with higher scores suggesting a higher levels of social support. By calculating the mean value of the MSPSS total score, we grouped the participants into low, moderate, and high perceived social support. Categories for all covariates are listed in Table 1.
Statistical analyses
Prevalence ratios (PR) of PND were estimated in relation to the total number of ACEs by fitting a log-binomial regression through the robust Poisson regression model (Chen et al. 2018). We then analyzed ACEs categorically by comparing individuals who had experienced 1, 2, 3, 4, or ≥ 5 ACE to those without ACEs. To better test the linear assumption, we also visulized the results by the total number of ACEs from 1 to 13.
We constructed four different models for adjustment. In the first model, crude estimates were reported. In the second model, we adjusted for potential confounders, including age and childhood deprivation. In the third model, we additionally adjusted for socioeconomic status at recruitment, including educational level, marital status, employment status, and income. In the final model, the estimates were further adjusted for potential mediators, including age at menarche, BMI, and parity. To reduce tests, we applied the final model in all subsequent association analyses described below.
Similarly, we examined associations for each type of ACEs with PND separately. To understand the independent role of ACE types, the estimates were further adjusted for the other ACEs in the same category.
To investigate potential risk modification by psychiatric comorbidities, we stratified the analyses by the presence of depression, other psychiatric comorbidities, and absence of the psychiatric comorbidities. Moreover, we stratified analyses by age to examine potential recall bias, and by social support to understand the role of current physical and emotional comfort provided by families and friends. To test for effect modification, an interaction term between PND and stratification factor was added and tested for statistical significance as P for interaction.
To shed light on PND subtypes, analyses were conducted for antenatal, postnatal, and persistent depression (both antenatal and postnatal depressive symptoms) separately, using all women not included in respective category as reference group. Additionally, we conducted a sensitivity analysis for postnatal depressive symptoms excluding women with postnatal depressive symptoms who experienced premature delivery (< 37 weeks) or serious illness, birth defect, or infant death in the first months (n = 356), as these are potentially traumatic events that could account for postnatal depression.
Lastly, to comply with the prevalence of PND in other population settings, a sensitivity analysis was conducted to assess the association of ACEs with PND by using a higher EPDS cut-off score (≥ 22) resulting in a prevalence of 11.1%.
The data were prepared and analyzed through RStudio (Version 1.2.5033) with the statistical significance set at the nominal two-side level of 0.05. This study was approved by the National Bioethics Committee of Iceland (reference number 13–017). Informed consents were obtained from all participants.
Results
At a mean age of 44 years (standard deviation (SD) 11.1), 6,201 (36.8%) women reported having experienced probable PND. The mean age when they reported suffering PND was 27.8 years (SD 5.7). Compared to women without PND, women with PND were younger at the survey and more likely to have suffered from childhood deprivation and having psychiatric comorbidities including depression. Women with PND were younger at menarche compared to women without PND. Furthermore, at the time of the survey, women who reported PND were more likely to be unemployed, single, obese, as well as to have lower educational levels and monthly income (Table 1).
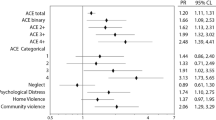
The prevalence of PND increased from 814 (21.6%) among women without any ACEs to 1,785 (60.2%) among those reporting ≥ 5 ACEs (Table 2). The total number of ACEs was positively associated with PND (Table 2, Model 1: PR 1.14 per ACE, 95% CI 1.13–1.15). After full adjustment, the association was somewhat attenuated yet significant (Table 2, Model 4: PR 1.11 per ACE, 95% CI 1.10–1.11). The PR gradually increased over categories of ACEs. Specifically, women who reported 5 or more ACEs were two times more likely to have experienced PND (Table 2, Model 4: PR 2.24, 95% CI 2.09–2.41). A dose–response relationship was observed between the number of ACEs and PND (P for trend < 0.001). The linear relationship was further confirmed when analyzing the number of ACEs from 1 to 13 (Online Resource Fig. S1).
All individual types of ACEs were positively associated with PND (Table 3). The strongest association was noted for emotional neglect (Table 3, PR 1.53, 95% CI: 1.47–1.59), followed by having someone mentally ill in the household (Table 3, PR 1.48, 95% CI: 1.42–1.54) and emotional abuse by a parent/guardian (Table 3, PR 1.46, 95% CI: 1.40–1.53). When additionally adjusting for ACEs in the same category, associations of loss of a parent or experience of parental separation and incarcerated household member attenuated to null.
In the stratified analysis, a stronger positive association was found among individuals without any psychiatric comorbidities (P for interaction < 0.001; Table 4). Moreover, we found a positive association between ACEs and PND across all age groups, although the PR was somewhat greater with increased age (P for interaction < 0.001; Table 4). Further, current perceived social support did not clearly modify the association although a weaker PR was noted among women having moderate social support (P for interaction < 0.001; Table 4).
In the analysis of PND subtypes, the strongest association was found for persistent depression (both antenatal and postnatal depressive symptoms) (PR: 1.12, 95% CI 1.11–1.13; Table 5). Women that endorsed 5 or more ACEs were almost three times more likely to have experienced persistent PND (PR: 2.83, 95% CI 2.50–3.20; Table 5). The association for postnatal depressive symptoms was comparable in the sensitivity analysis where we excluded women with postnatal depressive symptoms who experienced premature delivery, serious illness, birth defect, or infant death (Online Resource Table S1).
Last, in a sensitivity analysis of using a higher threshold for PND classification (EPDS cut-off score ≥ 22; prevalence 11.1%), an even stronger association was noted between the total number of ACEs and PND (PR: 1.18, 95% CI 1.16–1.20; Online Resource Table S2).
Discussion and conclusions
In this nationwide study of 16,831 Icelandic women with population representative sociodemographic characteristics, the findings indicated a positive association between the accumulative number of ACEs and PND symptoms in a dose–response manner. Specifically, women who were exposed to ≥ 5 ACEs had a twofold higher risk of PND than women with no ACEs. Moreover, we found that all 13 studied types of ACEs were positively associated with PND, albeit to a varying extent. The strongest association was noted for emotional neglect, followed by having someone mentally ill in the household and emotional abuse during childhood. While studies suggest impaired emotional clarity and regualtion as a possible mechanism linking emotional neglect to major depression (Jessar et al. 2017), further research is needed to understand why these ACEs are particularly associated with PND. Notably, in contradiction to most of the other ACEs where anyone can be considered the offender, emotional neglect and emotional abuse are specifically asked as the parent being the one that neglected or abused. Losing a parent or parental separation and having a household member incarcerated did not increase the risk of PND when other household dysfunctions were accounted for. In addition, we observed a stronger association between ACEs and PND among individuals without a comorbidity of psychiatric disorders. The association was most pronounced in women reporting persistent (both antenatal and postnatal) perinatal depression.
Although the SAGA cohort is representative of the Icelandic female population (Daníelsdóttir et al. 2022), the prevalence of PND in this study was 36.7%, which is considerably higher than in other studies (PR: 11.9–17%) (Shorey et al. 2018; Woody et al. 2017). The use of the lifetime version of the EPDS in our study may contribute to this higher prevalence as it will present a cumulative prevalence of PND from multiple pregnancies. Previous studies, although with dissimilar settings, have reported both higher (Kiewa et al. 2022; Meltzer-Brody et al. 2013) and lower prevalence (Viktorin et al. 2016) of PND using the EPDS lifetime version. In a sensitivity analysis where we increased the EPDS cut-off threshold to 22, the prevalence of PND was more comparable to other population settings (Woody et al. 2017), and we found an even stronger association between ACEs and PND symptoms.
Our results of accumulative number of ACEs and risk of PND are in line with previous studies on a single or fewer types of ACEs (Chung et al. 2008; Kumar et al. 2018; Leeners et al. 2014; Li et al. 2017; Osofsky et al. 2021; Racine et al. 2020; Rich-Edwards et al. 2011; Robertson-Blackmore et al. 2013; Samia et al. 2020; Tebeka et al. 2021; Zhang et al. 2019). A few studies measuring multiple types of ACEs have also indicated a does-response relationship (Tebeka et al. 2021; Wajid et al. 2020). However, none of these studies covered 13 ACE subtypes in one sample and analysed associations of each of them with PND. Particularly those not included in the pioneer study by Felitti et al. (1998) (e.g., loss of parent or parental separation, community and collective violence and bullying) have been less studied although some are common adverse experiences in childhood (Modecki et al. 2014). In line with previous studies, we also found positive associations of reported physical and emotional neglect (Lang et al. 2006; Li et al. 2017; Tebeka et al. 2021), emotional, sexual, and physical abuse (Benedict et al. 1999; Leeners et al. 2014; Robertson-Blackmore et al. 2013; Tebeka et al. 2021), and household dysfunction (Osofsky et al. 2021) during childhood and PND symptoms. Domestic violence was positively associated with PND in our study and has previously been associated with depressive symptoms at 36 months postpartum (LeMasters et al. 2021), while other studies (Chung et al. 2008) found domestic violence not significantly associated with antenatal depression, possibly due to different assesment of PND. Most importantly, being bullied during childhood has been associated with mental ill-health outside the perinatal period (McKay et al. 2021). However, bullying has not been analyzed separately in relation to PND although included in a couple of studies (LeMasters et al. 2021; Samia et al. 2020). Our findings indeed indicate that bullying is associated with an increased risk of PND symptoms.
Both ACEs (Copeland et al. 2018) and PND (Yang K et al. 2022a) have been associated with lower educational attainment, risky behaviours, and social functioning. In our study, the estimates were only slightly reduced when adjusting for educational level, income, and employment status at survey, indicating that these characteristics do not contribute significantly to the noted association between ACEs and PND.
ACEs are associated with an increased risk of a range of psychiatric disorders, including depression (Chapman et al. 2004; McKay et al. 2021; Tebeka et al. 2021). Moreover, it has been well recognized that pre-existing psychiatric disorders, especially depressive disorders, constitute an important risk factor of PND (Gastaldon et al. 2022; Guintivano et al. 2018; Howard et al. 2014; Yang K et al. 2022a). It is therefore plausible that pre-existing psychiatric disorders mediate the observed association between ACEs and PND. However, we found a positive association between ACEs and PND among individuals with and without psychiatric comorbidities, respectively. This suggests that pre-existing psychiatric disorders cannot completely explain our findings on the association between ACEs and PND symptoms.
Maltreatment during childhood is associated with morphological alterations in the brain (Teicher and Samson 2016), and ACEs might operate through psychobiological pathways leading to PND (Choi and Sikkema 2016). After exposure to a threatening event in childhood, the hypothalamic-pituitary-adrenal (HPA) axis is activated causing an increase in corticosteroids, which interact with cognitive and physical functions (de Kloet et al. 1999). Young children are more vulnerable to overexposure to corticosteroids induced by regular stress events and are therefore predisposed for stress-related disorders in adulthood (Chapman et al. 2004; Suzuki et al. 2014). Notably, during pregnancy, the placenta produces corticotrophins releasing hormone, activating the pituitary gland which in turn activates the adrenal gland to produce corticosteroids. Indeed, ACEs have been associated with heightened HPA axis activity and higher cortisol levels during pregnancy (Schreier et al. 2015). Moreover, the association between having someone mentally ill in the household during childhood and PND suggests potential confounding by familial factors, such as shared genetics between the participant with PND and the family member who was mentally ill. Further, psychosocial factors such as low social and emotional support by family members (Cho et al. 2022; Racine et al. 2020) and low resilience to distress in adulthood in women experiencing ACEs (Daníelsdóttir et al. 2022) could contribute to the association between ACEs and PND. Future studies may also assess other factors, such as adverse events in adulthood and comorbidities such as premenstrual syndrome, which perhaps could mediate the observed association.
Strengths and limitations
The major strength of this study is the large sample size, which allows us to explore the association of multiple ACEs and both PND subtypes and ACE subtypes. Moreover, our sample is representative of the Icelandic female population (Daníelsdóttir et al. 2022), whereas many previous studies on this association are based on smaller samples from clinical settings (Li et al. 2017; Samia et al. 2020; Tebeka et al. 2021).
One limitation of this study is the nature of the cross-sectional setting, which precludes any inferences on causality. In our study, the timeline between the exposure and outcome seems established, although both data were collected retrospectively. Moreover, there might be some misclassification of ACEs. The participants had to recall experiences that occurred during childhood at an average age of 44 years. However, we found a robust association between ACEs and PND among individuals aged 18–29 years, reducing concerns of recall bias. In addition, a validity study has found a good agreement between ACEs and the recall in adulthood (Dube et al. 2004). Mental state, such as ongoing symptoms of depression, can affect how childhood memories are viewed and recalled (Köhler et al. 2015). Although we found a strong association in women without psychiatric disorders, subclinical conditions could still result in recall bias on ACEs.
Furthermore, we might have misclassified some PND cases. The EPDS is designed as a screening tool for PND. To our knowledge, the EPDS has not been validated in the Icelandic population, although it has a high specificity and sensitivity in other Nordic countries, e.g. Sweden (specificity 88% and sensitivity 72%) (SBU 2012). Women who have experienced ACEs are more likely to report psychological problems, including PND. Hence, it is possible that the misclassification of PND is differential. However, the observed association between PND and ACEs is even stronger in the absence of psychiatric comorbidities, which decreases this possibility. Moreover, we used a modified EPDS (which captures lifetime prevalence), where women are asked to recall their experiences during and after pregnancy. Recall bias is therefore also a possibility, although it has been shown that the lifetime version is reliable enough for epidemiological studies (Meltzer-Brody et al. 2013). As mentioned above, the robust association noted in the group aged 18–29 somewhat alleviates the concern of potential recall bias in PND. Further, due to the structure of how data was collected, we were unable to assess when in relation to the delivery the EPDS was completed. In addition, we cannot rule out the possibility of residual confounding.
Clinical application
The results of this study suggest that screening pregnant women for ACEs could help identify women vulnerable to PND. Early identification of high-risk individuals may aid early detection and potential intervention, which would not only reduce the burden for the mother and her baby (O’Connor et al. 2019), but also the cost to the society (Bauer et al. 2016).
Conclusions
Our findings suggest that ACEs are positively associated with perinatal depressive symptoms in a dose–response manner, with emotional neglect, having someone mentally ill in the household, and emotional abuse by a parent/guardian presenting the strongest association. Our findings highlight the potential utility of screening for ACEs at maternal healthcare and may call for targeted prevention strategies for women with ACEs to lower the risk of PND. Finally, it is of utmost importance to prevent ACEs among children worldwide to minimize the impact on their adult life and intergenerational transmission of adverse health effects.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bauer A, Knapp M, Parsonage M (2016) Lifetime costs of perinatal anxiety and depression. J Affect Disord 192:83–90. https://doi.org/10.1016/j.jad.2015.12.005
Benedict MI, Paine LL, Paine LA, Brandt D, Stallings R (1999) The association of childhood sexual abuse with depressive symptoms during pregnancy, and selected pregnancy outcomes. Child Abuse Neglect 23(7):659–670. https://doi.org/10.1016/s0145-2134(99)00040-x
Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF (2004) Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord 82(2):217–225. https://doi.org/10.1016/j.jad.2003.12.013
Chen W, Qian L, Shi J, Franklin M (2018) Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol 18(1):63. https://doi.org/10.1186/s12874-018-0519-5
Cho H, Lee K, Choi E, Cho HN, Park B, Suh M, Rhee Y, Choi KS (2022) Association between social support and postpartum depression. Sci Rep 12:3128. https://doi.org/10.1038/s41598-022-07248-7
Choi KW, Sikkema KJ (2016) Childhood maltreatment and perinatal mood and anxiety disorders: a systematic review. Trauma Violence Abuse 17(5):427–453. https://doi.org/10.1177/1524838015584369
Chung EK, Mathew L, Elo IT, Coyne JC, Culhane JF (2008) Depressive symptoms in disadvantaged women receiving prenatal care: the influence of adverse and positive childhood experiences. Ambul Pediatr: Off J Ambul Pediatr Assoc 8(2):109–116. https://doi.org/10.1016/j.ambp.2007.12.003
Copeland WE, Shanahan L, Hinesley J, Chan RF, Aberg KA, Fairbank JA, van den Oord EJCG, Costello EJ (2018) Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open 1(7):e184493. https://doi.org/10.1001/jamanetworkopen.2018.4493
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal depression scale. Br J Psychiatry 150:782–786. https://doi.org/10.1192/bjp.150.6.782
Dachew BA, Ayano G, Betts K, Alati R (2021) The impact of pre-pregnancy BMI on maternal depressive and anxiety symptoms during pregnancy and the postpartum period: a systematic review and meta-analysis. J Affect Disord 281:321–330. https://doi.org/10.1016/j.jad.2020.12.010
Daníelsdóttir HB, Aspelund T, Thordardottir EB, Fall K, Fang F, Tómasson G, Rúnarsdóttir H, Yang Q, Choi KW, Kennedy B, Halldorsdottir T, Lu D, Song H, Jakobsdóttir J, Hauksdóttir A, Valdimarsdóttir UA (2022) Adverse childhood experiences and resilience among adult women: a population-based study. ELife 11:e71770. https://doi.org/10.7554/eLife.71770
de Kloet ER, Oitzl MS, Joëls M (1999) Stress and cognition: are corticosteroids good or bad guys? Trends Neurosci 22(10):422–426. https://doi.org/10.1016/s0166-2236(99)01438-1
Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF (2004) Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl 28(7):729–737. https://doi.org/10.1016/j.chiabu.2003.08.009
Eberhard-Gran M, Eskild A, Tambs K, Schei B, Opjordsmoen S (2001) The Edinburgh Postnatal depression scale: validation in a Norwegian community sample. Nord J Psychiatry 55(2):113–117. https://doi.org/10.1080/08039480151108525
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 14(4):245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
Gastaldon C, Solmi M, Correll CU, Barbui C, Schoretsanitis G (2022) Risk factors of postpartum depression and depressive symptoms: umbrella review of current evidence from systematic reviews and meta-analyses of observational studies. Br J Psychiatry: J Mental Sci: 1–12. https://doi.org/10.1192/bjp.2021.222
Guintivano J, Manuck T, Meltzer-Brody S (2018) Predictors of postpartum depression: a comprehensive review of the last decade of evidence. Clin Obstet Gynecol 61(3):591–603. https://doi.org/10.1097/GRF.0000000000000368
Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J (2014) Non-psychotic mental disorders in the perinatal period. Lancet 384(9956):1775–1788. https://doi.org/10.1016/S0140-6736(14)61276-9
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP (2017) The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2(8):e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4
Jessar AJ, Hamilton JL, Flynn M, Abramson LY, Alloy LB (2017) Emotional clarity as a mechanism linking emotional neglect and depressive symptoms during early adolescence. J Early Adolesc 37(3):414–432. https://doi.org/10.1177/0272431615609157
Kiewa J, Meltzer-Brody S, Milgrom J, Bennett E, Mackle T, Guintivano J, Hickie IB, Colodro-Conde L, Medland SE, Martin N, Wray N, Byrne E (2022) Lifetime prevalence and correlates of perinatal depression in a case-cohort study of depression. BMJ Open 12(8):e059300. https://doi.org/10.1136/bmjopen-2021-059300
Köhler CA, Carvalho AF, Alves GS, McIntyre RS, Hyphantis TN, Cammarota M (2015) Autobiographical memory disturbances in depression: a novel therapeutic target? Neural Plast 2015:759139. https://doi.org/10.1155/2015/759139
Kumar M, Amugune B, Madeghe B, Wambua GN, Osok J, Polkonikova-Wamoto A, Bukusi D, Were F, Huang K-Y (2018) Mechanisms associated with maternal adverse childhood experiences on offspring’s mental health in Nairobi informal settlements: a mediational model testing approach. BMC Psychiatry 18(1):381. https://doi.org/10.1186/s12888-018-1953-y
Lang AJ, Rodgers CS, Lebeck MM (2006) Associations between maternal childhood maltreatment and psychopathology and aggression during pregnancy and postpartum. Child Abuse Negl 30(1):17–25. https://doi.org/10.1016/j.chiabu.2005.07.006
Leeners B, Rath W, Block E, Görres G, Tschudin S (2014) Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med 42(2):171–178. https://doi.org/10.1515/jpm-2013-0003
LeMasters K, Bates LM, Chung EO, Gallis JA, Hagaman A, Scherer E, Sikander S, Staley BS, Zalla LC, Zivich PN, Maselko J (2021) Adverse childhood experiences and depression among women in rural Pakistan. BMC Public Health 21(1):400. https://doi.org/10.1186/s12889-021-10409-4
Li Y, Long Z, Cao D, Cao F (2017) Maternal history of child maltreatment and maternal depression risk in the perinatal period: a longitudinal study. Child Abuse Negl 63:192–201. https://doi.org/10.1016/j.chiabu.2016.12.001
McDonnell CG, Valentino K (2016) Intergenerational effects of childhood trauma: evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreat 21(4):317–326. https://doi.org/10.1177/1077559516659556
McKay MT, Cannon M, Chambers D, Conroy RM, Coughlan H, Dodd P, Healy C, O’Donnell L, Clarke MC (2021) Childhood trauma and adult mental disorder: a systematic review and meta-analysis of longitudinal cohort studies. Acta Psychiatr Scand 143(3):189–205. https://doi.org/10.1111/acps.13268
Meltzer-Brody S, Boschloo L, Jones I, Sullivan PF, Penninx BW (2013) The EPDS-Lifetime: assessment of lifetime prevalence and risk factors for perinatal depression in a large cohort of depressed women. Arch Womens Ment Health 16(6):465–473. https://doi.org/10.1007/s00737-013-0372-9
Menke RA, Swanson L, Erickson NL, Reglan G, Thompson S, Bullard KH, Rosenblum K, Lopez JP, Muzik M, WIMH Group at University of Michigan (2019) Childhood adversity and sleep are associated with symptom severity in perinatal women presenting for psychiatric care. Arch Womens Ment Health 22(4):457–465. https://doi.org/10.1007/s00737-018-0914-2
Mersky JP, Janczewski CE (2018) Adverse childhood experiences and postpartum depression in home visiting programs: prevalence, association, and mediating mechanisms. Matern Child Health J 22(7):1051–1058. https://doi.org/10.1007/s10995-018-2488-z
Miller ES, Fleming O, Ekpe EE, Grobman WA, Heard-Garris N (2021) Association between adverse childhood experiences and adverse pregnancy outcomes. Obstet Gynecol 138(5):770–776. https://doi.org/10.1097/AOG.0000000000004570
Modecki KL, Minchin J, Harbaugh AG, Guerra NG, Runions KC (2014) Bullying prevalence across contexts: a meta-analysis measuring cyber and traditional bullying. J Adolesc Health: Off Publ Soc Adolesc Med 55(5):602–611. https://doi.org/10.1016/j.jadohealth.2014.06.007
O’Connor E, Senger CA, Henninger ML, Coppola E, Gaynes BN (2019) Interventions to prevent perinatal depression: evidence report and systematic review for the US preventive services task force. JAMA 321(6):588–601. https://doi.org/10.1001/jama.2018.20865
Osofsky JD, Osofsky HJ, Frazer AL, Fields-Olivieri MA, Many M, Selby M, Holman S, Conrad E (2021) The importance of adverse childhood experiences during the perinatal period. Am Psychol 76(2):350–363. https://doi.org/10.1037/amp0000770
Racine N, Zumwalt K, McDonald S, Tough S, Madigan S (2020) Perinatal depression: the role of maternal adverse childhood experiences and social support. J Affect Disord 263:576–581. https://doi.org/10.1016/j.jad.2019.11.030
Racine N, Devereaux C, Cooke JE, Eirich R, Zhu J, Madigan S (2021) Adverse childhood experiences and maternal anxiety and depression: a meta-analysis. BMC Psychiatry 21(1):28. https://doi.org/10.1186/s12888-020-03017-w
Rich-Edwards JW, James-Todd T, Mohllajee A, Kleinman K, Burke A, Gillman MW, Wright RJ (2011) Lifetime maternal experiences of abuse and risk of pre-natal depression in two demographically distinct populations in Boston. Int J Epidemiol 40(2):375–384. https://doi.org/10.1093/ije/dyq247
Robertson-Blackmore E, Putnam FW, Rubinow DR, Matthieu M, Hunn JE, Putnam KT, Moynihan JA, O’Connor TG (2013) Antecedent trauma exposure and risk of depression in the perinatal period. J Clin Psychiatry 74(10):e942-948. https://doi.org/10.4088/JCP.13m08364
Rubertsson C, Borjesson K, Berglund A, Josefsson A, Sydsjo G (2011) The Swedish validation of Edinburgh Postnatal Depression Scale (EPDS) during pregnancy. Nord J Psychiatry 65(6):414–418. https://doi.org/10.3109/08039488.2011.590606
Rutter A (2021) The relevance of the adverse childhood experience international questionnaire to working children: knowledge gaps and implications for policy makers. Children (Basel, Switzerland) 8(10):897. https://doi.org/10.3390/children8100897
Samia P, Premji S, Tavangar F, Yim IS, Wanyonyi S, Merali M, Musana W, Omuse G, Forcheh N, Dosani A, Letourneau N, & The Maternal Infant Global Health Team MiGHT Collaborators In Research, null (2020) Adverse childhood experiences and changing levels of psychosocial distress scores across pregnancy in Kenyan women. Int J Environ Res Public Health 17(10):E3401. https://doi.org/10.3390/ijerph17103401
SBU, S. beredning för medicinsk och social utvärdering, Swedish Agency for Health Technology Assessment and Assessment of Social (2012) Diagnostik och uppföljning av förstämningssyndrom [HTA-rapport, systematisk litteraturöversikt, Systematic review, HTA]. https://www.sbu.se/sv/publikationer/SBU-utvarderar/diagnostik-och-uppfoljning-av-forstamningssyndrom/. Accessed 25 Nov 2022
Schreier HMC, Enlow MB, Ritz T, Gennings C, Wright RJ (2015) Childhood abuse is associated with increased hair cortisol levels among urban pregnant women. J Epidemiol Community Health 69(12):1169–1174. https://doi.org/10.1136/jech-2015-205541
Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS (2018) Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res 104:235–248. https://doi.org/10.1016/j.jpsychires.2018.08.001
Suzuki A, Poon L, Papadopoulos AS, Kumari V, Cleare AJ (2014) Long term effects of childhood trauma on cortisol stress reactivity in adulthood and relationship to the occurrence of depression. Psychoneuroendocrinology 50:289–299. https://doi.org/10.1016/j.psyneuen.2014.09.007
Tebeka S, Le Strat Y, Etain B, Ray M, Mullaert J, Dubertret C, & IGEDEPP Study Group (2021) Childhood trauma and perinatal depression: data from the IGEDEPP cohort. J Clin Psychiatry 82(5):20m13664. https://doi.org/10.4088/JCP.20m13664
Teicher MH, Samson JA (2016) Annual research review: enduring neurobiological effects of childhood abuse and neglect. J Child Psychol Psychiatry 57(3):241–266. https://doi.org/10.1111/jcpp.12507
Van Niel MS, Payne JL (2020) Perinatal depression: a review. Cleve Clin J Med 87(5):273–277. https://doi.org/10.3949/ccjm.87a.19054
Viktorin A, Meltzer-Brody S, Kuja-Halkola R, Sullivan PF, Landén M, Lichtenstein P, Magnusson PK (2016) Heritability of perinatal depression and genetic overlap with nonperinatal depression. Am J Psychiatry 173(2):158–165. https://doi.org/10.1176/appi.ajp.2015.15010085
Wajid A, van Zanten SV, Mughal MK, Biringer A, Austin M-P, Vermeyden L, Kingston D (2020) Adversity in childhood and depression in pregnancy. Arch Womens Ment Health 23(2):169–180. https://doi.org/10.1007/s00737-019-00966-4
World Health Organization (WHO) (2018) Adverse Childhood Experiences International Questionnaire (ACE-IQ) guidance for analysing ACE-IQ. Geneva: WHO 2018. Retrieved January 25, 2023, from https://cdn.who.int/media/docs/default-source/documents/child-maltreatment/ace-iq-guidance-for-analysing.pdf?sfvrsn=adfe12bb_2
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord 219:86–92. https://doi.org/10.1016/j.jad.2017.05.003
Yang K, Wu J, Chen X (2022a) Risk factors of perinatal depression in women: a systematic review and meta-analysis. BMC Psychiatry 22(1):63. https://doi.org/10.1186/s12888-021-03684-3
Yang Q, Þórðardóttir EB, Hauksdóttir A, Aspelund T, Jakobsdóttir J, Halldorsdottir T, Tomasson G, Rúnarsdóttir H, Danielsdottir HB, Bertone-Johnson ER, Sjölander A, Fang F, Lu D, Valdimarsdóttir UA (2022b) Association between adverse childhood experiences and premenstrual disorders: a cross-sectional analysis of 11,973 women. BMC Med 20(1):60. https://doi.org/10.1186/s12916-022-02275-7
Zhang S, Wang L, Yang T, Chen L, Qiu X, Wang T, Chen L, Zhao L, Ye Z, Zheng Z, Qin J (2019) Maternal violence experiences and risk of postpartum depression: a meta-analysis of cohort studies. Eur Psychiatr: J Assoc Eur Psychiatr 55:90–101. https://doi.org/10.1016/j.eurpsy.2018.10.005
Acknowledgements
Our greatest gratitude goes to the women participating in the SAGA cohort.
Funding
Open access funding provided by Karolinska Institute. This project was funded by the Grant of Excellence from the Icelandic Research Fund (No. 163362‑051 and 218274‑051) to Dr. Valdimarsdóttir, European Research Council (No. 726413) to Dr. Valdimarsdóttir, the Swedish Research Council for Health, Working Life and Welfare (FORTE) (No. 2020‑00971) to Dr. Lu, and the Swedish Research Council (Vetenskapsrådet) (No. 2020‑01003) to Dr. Lu.
Author information
Authors and Affiliations
Contributions
Emma Bränn and Alexandra Vaina conducted the literature review and the analyses and wrote the original manuscript draft. Hilda Björk Daníelsdóttir and Qian Yang supported the analyses. Edda Bjork Thordardottir was responsible for data curation. Jóhanna Jakobsdóttir and Thor Aspelund were responsible for data curation and participated in methodological design. Arna Hauksdóttir and Unnur A. Valdimarsdóttir conceptualized the study and were involved in data curation, and Unnur A. Valdimarsdóttir also provided funding. Donghao Lu conceptualized the study, provided funding, was involved in methodology design, was responsible for administration of this project, and was the main supervisor for author Alexandra Vaina. All authors of this paper have read, reviewed, and approved the final version submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Emma Bränn and Alexandra Vaina shared first authorship.
Supplementary Information
ESM 1
(DOCX 28.6 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bränn, E., Vaina, A., Daníelsdóttir, H.B. et al. Association between adverse childhood experiences and perinatal depressive symptoms: a cross-sectional analysis of 16,831 women in Iceland. Arch Womens Ment Health 26, 839–849 (2023). https://doi.org/10.1007/s00737-023-01369-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-023-01369-2