Abstract
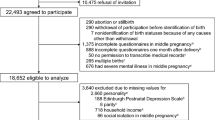
Suicidability has been associated with neuroticism and psychoticism, but its role during perinatal period has not been analyzed. We explore the association between personality dimensions, depressive symptoms, and other psychosocial variables in postpartum suicidal ideation. A cohort of 1795 healthy Spanish women from the general population was assessed for suicidal ideation (EPDS-Item10) in early postpartum, 8 and 32 weeks postpartum. Sociodemographic, obstetric, and reproductive variables, psychiatric history, social support, stressful life-events during pregnancy, depressive symptoms (EPDS), and the Eysenck’s personality dimensions (EPQ-RS) were also assessed at baseline. A major depressive episode (DSM-IV) was confirmed in women with EPDS>10 at follow-up assessments. Descriptive, bivariate, and multivariate analyses were conducted. Adjusted logistic regression analysis was reported as odds ratio (ORs) with 95% confidence intervals (CIs). Seven percent of mothers reported suicidal ideation during the first 8 months postpartum. Sixty-two percent of women with suicidal ideation had a major depressive episode at 8 weeks, and 70% at 32 weeks postpartum. Neuroticism and psychoticism predicted suicidal ideation throughout the first 2 weeks after delivery (OR, 1.03; 95%CI 1.01–1.06; and OR, 1.03; 95%CI 1.01–1.05 respectively). Early postpartum depressive symptoms (OR 1.2; 95%CI 1.11–1.26), personal psychiatric history (OR 2.1; 95%CI 1.33–3.27), and stressful life events during pregnancy (OR 1.88; 95%CI 1.12–3.16) also emerged as predictors of postpartum suicidal ideation. Analysis of women for postpartum suicidal ideation should include not only psychiatric symptoms but also psychosocial assessment (i.e., covering psychiatric history, stressful events, or long-standing personality vulnerabilities) in order to identify those in need of early psychosocial or psychiatric care.

Similar content being viewed by others
References
Alhusen JL, Frohman N, Purcell G (2015) Intimate partner violence and suicidal ideation in pregnant women. Arch Womens Ment Health 18:573–578
Austin M-P, Fisher J, Reilly N (2015) Psychosocial assessment and integrated perinatal care. In: Milgrom J, Gemmill AW (eds) Identifying Perinatal Depression and Anxiety: Evidence-based Practice in Screening, Psychosocial Assessment and Management. Wiley-Blackwell, Chichester, pp 121–138
Baca-Garcia E, Parra CP, Perez-Rodriguez MM et al (2007) Psychosocial stressors may be strongly associated with suicide attempts. Stress Health 23:191–198
Bellón JA, Delgado A, Luna JD, Lardelli P (1996) Validity and reliability of the Duke-UNC-11 questionnaire of functional social support | Validez y fiabilidad del cuestionario de apoyo social functional Duke-UNC-11. Aten Primaria 18:151–207
Bi B, Xiao X, Zang H et al (2012) A comparison of the clinical characteristics of women with recurrent major depression with and without suicidal symptomatology. Psychol Med 42:2591–2598
Bodnar-Deren S, Klipstein K, Fersh M et al (2016) Suicidal ideation during the postpartum period. J Women's Health 25:1219–1224
Brent DA, Melhem N (2008) Familial transmission of suicidal behavior. Psychiatr Clin N Am 31:157–177
Brezo J, Paris J, Turecki G (2006) Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatr Scand 113:180–206
Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH (1988) The Duke-UNC functional social support questionnaire: measurement of social support in family medicine patients. Med Care 26:707–721
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression scale. Br J Psychiatry 150:782–786
Esscher A, Essén B, Innala E et al (2016) Suicides during pregnancy and 1 year postpartum in Sweden, 1980-2007. Br J Psychiatry 208:462–469
Eysenck S (1985) Eysenck Personality Questionnaire-Revised (EPQ-R) and Short-Scale (EPQ-RS). Hooder and Stoughton, London
Eysenck H, Eysenck S (2001) Cuestionario revisado de personalidad de Eysenck: versiones completa (EPQ-R) y abreviada (EPQ-RS). TEA, Madrid
Farmer A, Redman K, Harris T et al (2001) The Cardiff sib-pair study: suicidal ideation in depressed and healthy subjects and their siblings. Crisis 22:71–73
Garcia-Esteve L, Ascaso C, Ojuel J, Navarro P (2003) Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord 75:71–76
Gavin AR, Tabb KM, Melville JL et al (2011) Prevalence and correlates of suicidal ideation during pregnancy. Arch Womens Ment Health 14:239–246
Gelaye B, Kajeepeta S, Williams MA (2016) Suicidal ideation in pregnancy: an epidemiologic review. Arch Womens Ment Health 19:741–751
Giallo R, Pilkington P, Borschmann R et al (2018) The prevalence and correlates of self-harm ideation trajectories in Australian women from pregnancy to 4-years postpartum. J Affect Disord 229:152–158
Girardi P, Pompili M, Innamorati M et al (2011) Temperament, post-partum depression, hopelessness, and suicide risk among women soon after delivering. Women Health 51:511–524
Goodwin RD, Gotlib IH (2004) Gender differences in depression: the role of personality factors. Psychiatry Res 126:135–142
Grigoriadis S, Wilton A, Kurdyack E et al (2017) Perinatal suicide in Ontario, Canada: a 15 year population -based study. CMAJ 28:189 E1085-92. https://doi.org/10.1503/cmaj.170088
Guillard V, Gressier F (2017) Suicidalité en période périnatale. Press Medicale 46:565–571
Horon IL, Chen D (2011) Effectiveness of pregnancy check boxes on the death certificates in indentifying pregnancy-associated mortality. Public Health Ret 126:195–200
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S (1997) A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 16:965–980
Howard LM, Flach C, Mehay A et al (2011) The prevalence of suicidal ideation identified by the Edinburgh Postnatal Depression Scale in postpartum women in primary care: findings from the RESPOND trial. BMC Pregnancy Childbirth 11:1–10
Kim JJ, La Porte LM, Saleh MP et al (2015) Suicide risk among perinatal women who report thoughts of self-harm on depression screens. Obstet Gynecol 125:885–893
Knight M, Nair M, Tuffnell D et al (2017) Saving lives, improving mothers’ care. National Perinatal Epidemiology Unit, University of Oxford, Oxford
Limburg K, Watson HJ, Hagger MS, Egan SJ (2017) The relationship between perfectionism and psychophathology: a meta-analysis. J Clin Psychol 73:1301–1326
Lindahl V, Pearson JL, Colpe L (2005) Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health 8:77–87
Mandelli L, Nearchou FA, Vaiopoulos C et al (2015) Neuroticism, social network, stressful life events: association with mood disorders, depressive symptoms and suicidal ideation in a community sample of women. Psychiatry Res 226:38–44
Mann JJ, Waternaux C, Haas GL, Malone KM (1999) Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 156:181–189
Martín-Santos R, Gelabert E, Subirà S et al (2012) Research letter: is neuroticism a risk factor for postpartum depression? Psychol Med 42:1559–1565
Mauri M, Oppo A, Borri C, Banti S (2012) Suicidality in the perinatal period: comparison of two self-report instruments. Results from PND-ReScU. Arch Womens Ment Health 15:39–47
Moore Simas TA, Brenckle L, Sankaran P et al (2019) The Program in support of Moms (PRISM): study potocol for a cluster randomized controlled trial of two active interventions addressing perinatal depression in obstetric settings. MBC Pregnancy Childbirth 19:256. https://doi.org/10.1186/s12884-019-2387-3
Navarro P, Ascaso C, Garcia-Esteve L et al (2007) Postnatal psychiatric morbidity: a validation study of the GHQ-12 and the EPDS as screening tools. Gen Hosp Psychiatry 29:1–7
Nock MK, Borges G, Bromet EJ et al (2008) Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 192:98–105
Nurnberger JI, Blehar MC et al (1994) Diagnostic interview for genetic studies: rationale, unique features, and training. Arch Gen Psychiatry 51:849–859
Oates M (2003) Suicide: the leading cause of maternal death. Br J Psychiatry 183:279–281
Onah MN, Field S, Bantjes J, Honikman S (2017) Perinatal suicidal ideation and behaviour: psychiatry and adversity. Arch Womens Ment Health 20:321–331
Orsolini L, Valchera A, Vecchiotti R et al (2016) Suicide during perinatal period: epidemiology, risk factors, and clinical correlates. Front Psychiatry 12. https://doi.org/10.3389/fpsyt.2016.00138
Paris R, Bolton RE, Weinberg MK (2009) Postpartum depression, suicidality, and mother-infant interactions. Arch Womens Ment Health 12:309–321
Paykel ES (1983) Methodological aspects of life events research. J Psychosom Res 27:341–352
Pickles A, Aglan A, Collishaw S et al (2010) Predictors of suicidality across the life span: The Isle of Wight study. Psychol Med 40:1453–1466
Pope CJ, Xie B, Sharma V, Campbell MK (2013) A prospective study of thoughts of self-harm and suicidal ideation during the postpartum period in women with mood disorders. Arch Womens Ment Health 16:483–488
Rappaport LM, Flint J, Kendler KS (2017) Clarifying the role of neuroticism in suicidal ideation and suicide attempt among women with major depressive disorder. Psychol Med 47:2334–2344
Reilly N, Kingston D, Loxton D et al (2019) A narrative review of studies addressing the clinical effectiveness of perinatal depression screening programs. Women Birth 3. https://doi.org/10.1016/jwombi.2019.03.004
Roca M, Martin-Santos R, Saiz J et al (2007) Diagnostic Interview for Genetic Studies (DIGS): inter-rater and test-retest reliability and validity in a Spanish population. Eur Psychiatry 22:44–48
Sanjuán J, Martin-Santos R, Garcia-Esteve L et al (2008) Mood changes after delivery: role of the serotonin transporter gene. Br J Psychiatry 193:383–388
Schuitemaker N, Van Roosmalen J, Dekker J et al (1997) Underreporting of materanl mortality in the Netherlands. Obstet Gynecol 90:68–82
Serafini G, Muzio C, Piccinini G et al (2015) Life adversities and suicidal behavior in young individuals: a systematic review. Eur Child Adolesc Psychiatry 24(12):1423–1446
Sit D, Seltman H, Wisner KL (2011) Seasonal effects on depression risk and suicidal symptoms in postpartum women. Depress Anxiety 28:400–405
Sit D, Luther J, Buysse D et al (2015) Suicidal ideation in depressed postpartum women: associations withchildhood trauma, sleep disturbance and anxiety. J Psychiatr Res 66–67:95–104
The Lancet. Editorial (2016) Screening for perinatal depression: a missed opportunity. Lancet 387:505
Voracek M, Loibl LM (2007) Genetics of suicide: a systematic review of twin studies. Wien Klin Wochenschr 119:463–475
Vrshek-Schallhorn S, Czarlinski J, Mineka S et al (2011) Prospective predictors of suicidal ideation during depressive episodes among older adolescents and young adults. Personal Individ Differ 50:1202–1207
WHO; World Health Organization (2019) Mental health. Suicide data. https://www.who.int/gho/publications/world_health_statistics/2019/EN_WHS_2019_Annex2.pdf?ua=1. Accessed August 2019
Woody CA, Ferrari AJ, Siskind DJ et al (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord 219:86–92
Zhong QY, Gelaye B, Rondon MB et al (2014) Using the Patient Health Questionnaire (PHQ-9) and the Edinburgh Postnatal Depression Scale (EPDS) to assess suicidal ideation among pregnant women in Lima, Peru. Arch Womens Ment Health 18:783–792
Acknowledgements
This work was carried out with the Instituto Carlos III (Spanish Ministry of Health) grants, FIS (PI041635, PI041783, PI041779, PI041761, PI041791, PI041766 and PI041782), as well as the Spanish Psychiatric Genetics and Genotyping network GO3/184. We also acknowledge the support of the Centro de Investigación Biomédica en Red en Salud Mental (CIBERSAM), Instituto Carlos III (Spanish Ministry of Health) and the Secretaria d'Universitats i Recerca del Departament d'Economia i Coneixement, Generalitat de Catalunya (SGR2014/1114; SGR2017/1798). We would like to thank all women who agreed to participate in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
E. Gelabert and A. Gutierrez-Zotes both are first authors.
Rights and permissions
About this article
Cite this article
Gelabert, E., Gutierrez-Zotes, A., Navines, R. et al. The role of personality dimensions, depressive symptoms and other psychosocial variables in predicting postpartum suicidal ideation: a cohort study. Arch Womens Ment Health 23, 585–593 (2020). https://doi.org/10.1007/s00737-019-01007-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-019-01007-w