Abstract
The ability to perform activities of daily living (ADL) function is a multifaceted construct that reflects functionality in different daily life situations. The loss of ADL function due to cognitive impairment is the core feature for the diagnosis of Parkinson’s disease dementia (PDD). In contrast to Alzheimer’s disease, ADL impairment in PD can be compromised by various factors, including motor and non-motor aspects. This narrative review summarizes the current state of knowledge on the association of cognition and ADL function in people with PD and introduces the concept of “cognitive ADL” impairment for those problems in everyday life that are associated with cognitive deterioration as their primary cause. Assessment of cognitive ADL impairment is challenging because self-ratings, informant-ratings, and performance-based assessments seldomly differentiate between “cognitive” and “motor” aspects of ADL. ADL function in PD is related to multiple cognitive domains, with attention, executive function, and memory being particularly relevant. Cognitive ADL impairment is characterized by behavioral anomalies such as trial-and-error behavior or task step omissions, and is associated with lower engagement in everyday behaviors, as suggested by physical activity levels and prolonged sedentary behavior. First evidence shows that physical and multi-domain interventions may improve ADL function, in general, but the evidence is confounded by motor aspects. Large multicenter randomized controlled trials with cognitive ADL function as primary outcome are needed to investigate which pharmacological and non-pharmacological interventions can effectively prevent or delay deterioration of cognitive ADL function, and ultimately the progression and conversion to PDD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In this narrative review, we present the current state of knowledge on the association between cognition and activities of daily living (ADL) function in Parkinson’s disease (PD) and introduce the term cognitive ADL impairment for those problems in everyday life associated with cognitive deterioration.
First, we provide a brief overview of cognitive impairment in PD. Cognitive impairment is one of the most common and troublesome non-motor symptoms in people with PD. The occurrence and severity of cognitive impairment in PD is associated with shorter life expectancy, contributes to distress amongst caregivers, and increases the risk of nursing home placement (Bjornestad et al. 2017). Approximately 60% to 83% of people with PD develop Parkinson’s disease dementia (PDD) during the course of their disease (Hely et al. 2008), and about 20 to 33% of patients experience mild cognitive impairment (PD-MCI) already at the time of PD diagnosis (Lawson et al. 2017; Santangelo et al. 2015). Cognitive functions, particularly executive functions such as verbal fluency performance (Darweesh et al. 2017b; Behnke et al. 2007), and set shifting (Thaler et al. 2012) may already be impaired in the prodromal stage of PD. Moreover, working memory performance (Darweesh et al. 2017a) and memory complaints (Foubert-Samier et al. 2020; Schrag et al. 2015) were found to be associated with PD conversion. Additionally, reduced visual memory performance has also been reported in PD-free glucocerebrosidase (GBA) mutation carriers (Zokaei et al. 2014) and impaired verbal memory performance (Yilmaz et al. 2016; Holthoff et al. 1994; Chahine et al. 2015) in PD risk groups. These results emphasize that cognition may decline even before the PD motor symptoms are severe enough to justify the clinical diagnosis of PD (Fengler et al. 2017; Liepelt-Scarfone et al. 2022; Berg et al. 2012). The profile of cognitive impairment in PD is heterogeneous (Aarsland et al. 2021; Kehagia et al. 2010). Executive dysfunction, such as reduced information generation, response inhibition, rule deduction, dual-task performance, or set-shifting occur early in the disease stage and are modulated by frontal-striatal alterations (Dirnberger and Jahanshahi 2013). Episodic memory retrieval and metacognitive processes are also affected by executive control (Dirnberger and Jahanshahi 2013). Furthermore, difficulties in working memory performance and immediate and delayed free recall (Kalbe et al. 2016; Muslimovic et al. 2005; Warden et al. 2016), as well as problems in goal-directed allocation of attention, internal attentional control (Bin Yoo et al. 2018), and visuo-cognitive skills (e.g. visuo-constructive abilities with command tasks; Liebermann-Jordanidis et al. 2022) frequently occur in PD. Language deficits, such as naming difficulties or sentence production with reduced information content have been reported in later stages of PD (Hobson and Meara 2004; Small et al. 1997). However, there is increasing evidence that language deficits occur in all disease stages and that complex sentence comprehension deficits are linked to basal ganglia damage in people with PD (Novakova et al. 2023; Altmann and Troche 2011). These cognitive difficulties may have a detrimental impact on the patents’ ability to function effectively in everyday life. For example, executive functions are regarded as crucial to maintain everyday skills (Godefroy et al. 2010; Koerts et al. 2011) and impaired cortical executive control may account for lost automaticity even in formerly routine tasks (Ferrazzoli et al. 2018; Dirnberger and Jahanshahi 2013).
Preventing or delaying PDD is a matter of great urgency due to its devastating impact on patients and caregivers. Besides older age, the presence of PD-MCI is an established risk factor for PDD (Litvan et al. 2011). PD-MCI can be defined as the intermediate stage of cognitive impairment between normal cognitive function and dementia. Frontal-striatal pathological changes may originate from nigrostriatal and subsequent mesocortical dopamine denervation (Kehagia et al. 2010). Loss of noradrenergic innervation, originating in the locus coeruleus, has also been reported in people with PD-MCI, whereas serotonergic dysfunction is not directly related to cognitive decline (for details see Aarsland et al. 2021). Extensive Lewy body pathology, widespread cortical and subcortical degeneration, and a profound cholinergic deficit may increase the risk for dementia (Kehagia et al. 2013; Williams-Gray et al. 2009). According to the dual-syndrome hypothesis (Kehagia et al. 2010, 2013), cognitive deficits are not limited to executive dysfunction and memory impairments, which are observed in early-stage cognitive impairment in PD, but also include other distinctive cholinergic visuospatial, memory and psychiatric deficits associated with PDD (Aarsland et al. 2021; Kehagia et al. 2010). Of those, worsening of visuo-cognitive skills has been reported to predict cognitive impairment and PDD (Mahieux et al. 1998; Williams-Gray et al. 2009), and language problems occur in the transition to PDD (Hobson and Meara 2004). For an overview of possible neural substrates of specific cognitive functions, we refer to Aarsland et al. (2021) and Citro et al. (2024).
However, PD-MCI is a heterogeneous concept; a recent meta-analysis found that, on average, 31% of PD-MCI patients converted to dementia within seven years; but 24% of PD-MCI patients reverted back to normal cognitive function (Saredakis et al. 2019). This heterogeneity highlights that additional markers are needed to identify those PD-MCI patients that are at high risk for the development of PDD.
Established diagnostic criteria have defined ADL impairment with impact on patients’ personal, occupational, and social daily life due to cognitive deterioration as the core feature differentiating PDD from PD-MCI (Dubois et al. 2007; Emre et al. 2007). It has been reported that the onset of early signs of ADL impairment is a potential risk marker for PDD, which can already be observed in about 30% to 50% of PD-MCI patients (Glonnegger et al. 2016; Martin et al. 2013). People with PD-MCI who display exclusive impairment in ADL tasks that are cognitively demanding and more complex are at an increased risk to develop PDD within three years (Becker et al. 2022a). This finding suggests that the emergence of ADL impairment associated with cognition (cognitive ADL impairment) could serve as an important clinical marker for future PDD, potentially lowering the false-positive rate in people with PD-MCI. In order to pave the path for future research, it is therefore crucial to enhance our understanding of the relationship between cognition and ADL function in PD.
ADL impairment associated with cognition in PD
Definition of cognitive ADL impairment and theoretical conceptualization
The evaluation of a patient’s ability to lead an independent life within their community is a key element of clinical practice for the diagnosis of cognitive impairment. Because ADL function can be viewed as a multifaceted construct that reflects functionality in different daily life situations, it is thought to offer a holistic understanding of the patient’s health within the broader context of their physical, emotional, and social well-being (Bezdicek et al. 2023; Bruderer-Hofstetter et al. 2020). ADL function is commonly divided into basic ADL, which involve self-maintenance skills such as bathing, dressing, or eating, and instrumental ADL (IADL), which involve more complex tasks such as medication management, grocery shopping, or financial administration (Lawton and Brody 1969). More severe ADL impairment in PD has been associated with demographic factors (e.g. higher age, male sex), progressive motor impairment, and non-motor symptoms such as depression (Holroyd et al. 2005; Lang et al. 2013; Sperens et al. 2020). The neurobiology of ADL impairment in PD is still unclear. Lower global ADL function has been linked to reduced functional connectivity in people with PD (Yoo et al. 2015). Beta-Amyloid burden has been shown to be related to ADL impairment in non-PD older adults with MCI, although this association has not yet been confirmed in PD (Jutten et al. 2019).
As mentioned before, losing the ability to perform ADL tasks due to cognitive dysfunction is mandatory for the diagnosis of PDD (Dubois et al. 2007). Therefore, it is necessary to gain insight into how a patient applies their cognitive skills to ADL tasks, that is, real-world situations embedded in a context-rich environment. In order to make a valid diagnosis of PDD, it is important to identify the sources of the patient’s ADL impairment, since PD is primarily a movement disorder. Thereby, distinguishing between different sources of their ADL impairment might be challenging, as motor disturbances also negatively affect ADL function in PD (Lee et al. 2014; Skinner et al. 2015; Rosenthal et al. 2010). For instance, tremors may impede the performance of actions related to meal intake, such as cutting food or bringing a spoon to the mouth without spilling the food (Hanff et al. 2022; Westergren et al. 2016). Additionally, falls frequently occur during everyday behaviors that involve sit-to-stand transfers, walking, bending, reaching, or standing (Allen et al. 2013; Ashburn et al. 2008) and evidence indicates that people with PD who are afraid of falling avoid many daily life situations (Bezdicek et al. 2022; Rider et al. 2023), engaging in less bodily behaviors that involve movement (Atrsaei et al. 2021; Landers et al. 2021). These observable motor aspects may influence the patients’ and the caregivers’ ADL ratings specifically in those ADL tasks that involve substantial physical movement (Becker et al. 2020). On the other hand, an ADL task such as making a doctor’s appointment requires the patient to remember their doctor’s phone number and to effectively communicate in order to match available times with their personal calendar, all while sustaining noisy distractions in the background. This ADL task could therefore be regarded as more cognitively demanding and potentially more sensitive to cognitive dysfunction. The comparison between these two ADL tasks illustrates that situations in everyday life may be qualitatively different in terms of their demands on cognitive abilities and motor skills.
However, distinguishing between the sources of ADL impairment may not always be straightforward. For example, dialing the doctor’s phone number might be more difficult with reduced fine motor function (Lopez et al. 2019; Staunton et al. 2022). The level of required movement may also differ between ADL tasks, and hence their susceptibility to motor confounds may differ accordingly. Motor-related difficulties, such as spilling food can also cause stress or shame in patients (Thordardottir et al. 2014). This may lead them to withdraw from public and social activities to avoid these aversive feelings (Ahn et al. 2022; Thordardottir et al. 2014), a behavior that may be similar to the social isolation frequently observed in dementia (Geng et al. 2024; Lazzari and Rabottini 2022; Shen et al. 2022). Depressive symptoms and apathy, regardless of the presence of motor symptoms, can lead to difficulties in coping with everyday life because persons may lack motivation and interest in activities and experience a loss of energy (Laatu et al. 2013; Numbers et al. 2022). The risk of depression is higher in people with PDD than in those without cognitive impairment, i.e., both phenomena often occur together and have an impact on everyday life (Riedel et al. 2010). Thus, a valid differential diagnosis of depression and dementia is of great importance for further treatment decisions. Another non-motor symptom is autonomic dysfunction, bladder disorders in particular, which patients identify as having a substantially negative impact on their everyday life (Allan et al. 2006). To support the diagnosis of PDD, these diverse factors affecting ADL function should be considered in order to identify if cognitive dysfunction is the primary factor of a patient’s ADL impairment. Therefore, understanding which ADL tasks are more appropriate for detecting cognitive ADL impairment is essential to support the diagnosis of PDD.
The findings presented above show that ADL impairment cannot be regarded as a universal construct. It was reported that people with PD-MCI encountered more difficulties with travelling outside of the house, involving motor actions such as walking, going by car or by bus, than people with Alzheimer’s disease MCI (Becker et al. 2021). Difficulties in these actions could hence lead to an overestimation of ADL impairment or even false positive diagnosis of functional dependence (Almeida et al. 2017). Conversely, these findings may also suggest that ADL impairment of a patient with more impaired cognition, but less severe motor symptoms, could be underestimated in an assessment that primarily focuses on motor-demanding ADL. These issues underscore the importance of carefully deconstructing the demands of ADL tasks for an accurate clinical assessment, in order to avoid overestimating or underestimating ADL impairment.
Fortunately, the awareness for these issues is growing in research. Attempts of deconstructing ADL demands show that it is possible to distinguish between ADL tasks based on their reliance on different skills. For example, factor analytic and regression-based approaches have found the ADL task of financial management to be cognitively more demanding (Becker et al. 2020; Sulzer et al. 2020), as compared to the ADL of shopping, which was more influenced by motor symptoms (Becker et al. 2020; Cheon et al. 2015). Furthermore, certain ADL tasks appear to be more affected by depressive symptoms than others (Choi et al. 2019). Most important, novel assessments have been developed (PASS and PDAQ-15; Foster et al. 2014; Holden et al. 2018) to evaluate performance in ADL with greater cognitive demands, and there have also been suggestions for adapting existing clinical measures (Almeida et al. 2017; Becker et al. 2020; Cheon et al. 2015). Based on these issues, we introduce the term cognitive ADL impairment for those ADL tasks that are most likely to be affected by cognitive impairment in PD.
ADL impairment and cognitive diagnosis in PD
Comparisons among cognitive subgroups in PD show that ADL impairment worsens with cognitive impairment: People with PDD show the most pronounced ADL impairment, specifically in IADL, compared to non-demented people with PD, followed by people with PD-MCI compared to cognitively normal PD (PD-NC) patients (Almeida et al. 2017; Beyle et al. 2018; Cholerton et al. 2020; Giovannetti et al. 2012; Glonnegger et al. 2016; Becker et al. 2020; Cheon et al. 2015; Holden et al. 2018; Fellows and Schmitter-Edgecombe 2019; Kulisevsky et al. 2013).
Therefore, research indicates that cognition is closely intertwined with ADL function, with initial ADL problems being already evident in PD-MCI. Despite these findings, understanding of the progression of ADL function associated with cognitive worsening in PD has been largely neglected (Martin et al. 2013). Additionally, ADL impairment increases within the transition phase of PDD converters (Becker et al. 2022a; Beyle et al. 2018), and presence of cognitive ADL impairment increases the risk for PDD conversion within three years (Becker et al. 2022a). However, not all studies have confirmed the direct link between cognition and ADL function in PD (Reginold et al. 2012; Pirogovsky et al. 2014). Different ways to clinically assess cognitive ADL function will be presented below, followed by their cognitive correlates. Then, an outlook on novel assessments will be provided, and current findings on available interventions will be summarized.
Evaluating ADL in clinical routine
Assessment of ADL function in PD typically involves self-ratings by the patient or informant-ratings made by a spouse, a close relative, or other knowledgeable informants (Shulman et al. 2016). Thereby, patients and informants may derive their ratings by comparing multiple everyday observations with the patients’ premorbid level of functioning (Schmitter-Edgecombe et al. 2011), hence providing important insights on the personal experiences of within-patients changes. As an alternative to these subjective ratings, performance-based ADL assessments evaluate individuals as they carry out simulated everyday scenarios (Giovannetti et al. 2012; Holden et al. 2018; Sulzer et al. 2020).
Self-ratings of ADL function have not consistently demonstrated the ability to distinguish between cognitive subgroups in PD (Holden et al. 2019; Pirogovsky et al. 2012, 2014). Accurate self-ratings require adequate cognitive functioning, as patients must understand the questions and be aware of their own, even subtle ADL impairments. Accordingly, overestimations of ADL function in people with PD have been associated with decreased awareness (Lehrner et al. 2015), a phenomenon that is observed more frequently in people with cognitive impairment (Pennington et al. 2021; Siciliano et al. 2021) and is at least partly modulated by executive function and attention (Kudlicka et al. 2013; Siciliano et al. 2021). Consequently, there is discordance between self-ratings, informant-ratings, and performance-based ADL assessments, which becomes more pronounced as patients’ cognition decreases (Becker et al. 2020; Deck et al. 2019; Shulman et al. 2006). Self-ratings may primarily be sensitive to ADL impairment in the initial stages of cognitive impairment, as self-ratings of ADL function have been reported to correlate with ADL performance in people with PD-NC but not in those with PD-MCI or PDD (Holden et al. 2019). Importantly, in the initial stages of cognitive impairment, self-ratings may be even more sensitive than informant-ratings because people with PD may be highly alert to any detriment in their ability to perform especially more complex ADL, which may, however, be subtle to informants (Cholerton et al. 2020; Kudlicka et al. 2013). Conversely, informant-ratings may be sensitive to ADL impairment in later stages of cognitive decline, as they demonstrate higher consistency with performance-based ADL assessments than patients’ self-ratings (Becker et al. 2022c; Deck et al. 2019; Shulman et al. 2006). Informant-ratings may, however, be negatively biased due to the informants’ caregiving burden, which has been found to increase with patients’ cognitive impairment (Caap-Ahlgren and Dehlin 2002; Ransmayr 2020). A further issue of rating scales in general is that their accuracy can be reduced by measurement errors. For example, raters may interpret items differently and their responses may be influenced by response tendencies (Matthews et al. 2012; Zolfaghari et al. 2022). Taken together, these findings suggest that cognitive impairment may introduce bias into subjective ADL assessments and that the sensitivity of self-ratings and informant-ratings of cognitive ADL impairment may vary with cognitive deterioration.
Performance-based ADL assessments are directly based on ADL situations, rather than the subjective recall of such, which is the case with subjective ADL ratings (Deck et al. 2019; Schmitter-Edgecombe et al. 2022; Shulman et al. 2006). Comparisons between cognitive subgroups in PD consistently indicate that as cognitive impairment increases, performance-based ADL function also deteriorates (Beyle et al. 2018; Glonnegger et al. 2016; Giovannetti et al. 2012; Holden et al. 2018). In performance-based ADL assessments, individuals are prompted to carry out particular tasks from different ADL domains, such as preparing meals or beverages, shopping, making phone calls, managing medications, using public transportation, or managing finances (Glonnegger et al. 2016; Holden et al. 2018; Sulzer et al. 2020). Most often, ADL function is assessed as overall performance across multiple ADL domains, however, there are also assessments that focus on single ADL domains (Carlson et al. 2005; Marson et al. 2000; Patterson et al. 2002). Thereby, ADL function is evaluated based on quantifiable aspects of the individual’s behavior, such as the number of committed errors, the number of cues provided by the investigators, and the completion time. These aspects are typically protocol documented by external investigators with high inter-rater reliability (Beyle et al. 2018; Giovannetti et al. 2012; Sulzer et al. 2020). Criticism of performance-based ADL assessments may be that they are often time-consuming (Martin et al. 2013; Shulman et al. 2016; Pirogovsky et al. 2013; Roll et al. 2019; Brennan et al. 2016c) and/or involve a high level of material expenditure (Fellows and Schmitter-Edgecombe 2019; Foster 2014). Another shortcoming of performance-based ADL assessments is that they are limited to the laboratory test situation (Warmerdam et al. 2020) and that they may not adequately evaluate intra-individual fluctuations of ADL function as well as the frequency of ADL difficulties in daily life (Cain et al. 2009; Weakley et al. 2019). Moreover, performance may be modulated by several psychological factors that are influenced by the laboratory situation (Paradis and Sutkin 2017; Warmerdam et al. 2020). Despite these limitations, performance-based ADL assessments present an objective and standardized method of assessing cognitive ADL function without cognitive bias outside of an individual’s routines in their home-based environment.
Clinical ADL assessments to support cognitive diagnosis in PD
The International Parkinson and Movement Disorder Society (MDS) Task Force on Rating Scales recommended the following scales for the assessment of disabilities in PD (see Shulman et al. 2016 for details). Of all scales recommended by the MDS Task Force on Rating scales, only the IADL scale of Lawton & Brody, the UPDRS-II, and the Schwab and England (S&E-ADL) scale have been evaluated in their diagnostic abilities to differentiate cognitive subgroups.
Table 1 gives an overview of various ADL scales which support the diagnosis of PDD, therefore reflecting cognitive ADL impairment. Except for the IADL scale from the Lawton & Brody scale and the Pill-Questionnaire, the diagnostic discriminatory power for PDD of the scales discussed below has only been confirmed in a single study. The IADL scale of Lawton & Brody (Lawton and Brody 1969) is used as a self- and informant-rated assessment (Christ et al. 2013) and includes eight different ADL domains (e.g. shopping, using transport), which are based on items rated on a three-point Likert scale. Group comparisons show that the informant rated scale can differentiate test performance between people with and without PDD (Dujardin et al. 2010; Giovannetti et al. 2012). Scoring of the IADL scale differs, with ratings on a two-point Likert scale (0 = less able or 1 = more able to do the task), resulting in a maximum score of 8, as well as ratings on a four-point Likert score (0 = unable to do the task to 2 = independent), resulting in a maximum score of 24 (Shulman et al. 2016). For both scores, higher values indicate better ADL performance.
The S&E-ADL Scale (Schwab and England 1968) is rated by physicians, patients, or staff (McRae et al. 2000) using a scale that ranges from 0% to 100% (completely independent; Shulman et al. 2016). The S&E-ADL scale score of people with PDD cannot be differentiated from those with PD-MCI but is able to distinguish PD-NC from people with PD with cognitive impairment (Leroi et al. 2012). The UPDRS is a rating tool designed to allow physicians to monitor worsening or improvement of PD over time in four subparts (Goetz et al. 2008). Its second subpart, the UPDRS-II, covers ADL function, but places greater emphasis on motor limitations than on cognitive limitations. In particular, some of the items of the UPDRS-II enquire about tremor, falling, freezing, or difficulties in swallowing. These items do not represent cognitive ADL impairment and consequently, they can be omitted from the assessment of cognitive ADL function without loss of reliability (Goetz et al. 2008). To date, the discriminatory power of the MDS-UPDRS-II score has not yet been investigated.
In addition to the recommendation of the MDS Task Force on Rating Scales for the assessment of disabilities in PD, good diagnostic discriminatory power of the informant-rated Parkinson’s Disease Cognitive Functional Rating Scale (PD-CFRS) has been suggested for the comparison between people with PDD and non-demented people with PD (Kulisevsky et al. 2013). Studies confirm the reliability and validity of the PD-CFRS, and a change in test score has been reported to correlate with cognitive decline after one year (Kulisevsky et al. 2013; Ruzafa-Valiente et al. 2016; Rosenblum et al. 2022). The performance-based University of California San Diego Performance-Based Skills Assessment (UPSA) was originally designed for the use in schizophrenia (Patterson et al. 2002) and for the assessment of performance in five ADL domains (Financial, Communication, Planning/Organization, Travel, and Household), which are scored separately (range 0–20) and are summed to a total UPSA score (range 0–100). Reliability and validity of the UPSA is good (Holden et al. 2020), but test performance needs to be adjusted for age, education, disease duration, intake of dopaminergic medication, and motor impairment. Sensitivity to change has been recently demonstrated in people with PD (Carlisle et al. 2023). However, baseline scores of the UPSA did not predict the rate of change in cognition over time, and therefore did not identify those individuals at greatest risk of cognitive decline. Discriminatory power of the UPSA for PDD among non-demented people with PD is high, a cut-off score of 83 identified PD-MCI vs. PD-NC with a sensitivity of 79% and a specificity of 64% (Holden et al. 2018).
The Pill Questionnaire has been recommended by a group of PD experts to assess ADL function that is indicative of PDD (Dubois et al. 2007). The test requires people with PD to report intake on their regular Parkinson medication (Dubois et al. 2007). Therefore, the Pill Questionnaire can be considered as a memory task and does not require any demonstration of directly observable ADL functions or transfer performance. Scoring of the scales varies from a graded four-point classification (Reginold et al. 2012; Martinez-Martin 2013; Dubois et al. 2007) of persons’ independence for ADL function and a dichotomized performance rating (Christ et al. 2013). Studies have reported good discriminatory power of the Pill Questionnaire for PDD (Christ et al. 2013; Martinez-Martin 2013). The Pill Questionnaire has a high false-positive rate and potential diagnosis of PDD must be further clarified if the test result is positive (Martinez-Martin 2013). In non-demented people with PD, the Pill Questionnaire has demonstrated low sensitivity (41%) and specificity (80%) in detecting PD-MCI (Reginold et al. 2012). The reliability of the Pill Questionnaire and its sensitivity to change have not yet been proven in PD. In addition, test performance may be negatively influenced by various factors (e.g. presence of apathy, depression, level of education).
Another scale specifically developed to assess cognitive ADL function in PD is the informant-rated Penn Parkinson’s daily activities questionnaire-15 (PDAQ-15, Jonasson et al. 2017). The items of the PDAQ-15 were selected based on experts' opinions from the original 50-item version of the PDAQ (Brennan et al. 2016b), rated on a five-point Likert scale (0 to 4 points). The association between global cognition and the PDAQ-15 has been reported to be large, but the test score was also correlated with the UPDRS-III motor score, though to a minor extent. A cutoff of 37 differentiated PD-MCI from PDD with a sensitivity of 83% and a specificity of 71%. Self-ratings and informant ratings showed moderate agreement on the overall PDAQ-15 (Deck et al. 2019), and self-reported cognitive complaints were predicted by the PDAQ-15 at three years (Weintraub et al. 2024). In addition, the PDAQ-15 demonstrated the ability to reflect treatment-induced improvement of ADL function after deep brain stimulation, indicating good sensitivity to change (Bezdicek et al. 2022). The observer-based Performance Assessment of Self-care Skills (PASS) was also designed to assess cognitively-demanding IADL performance in participants with PD without dementia (Foster and Doty 2021). The PASS score is primarily associated with cognitive function and to a lesser extent with motor performance. Between-group analysis has been shown to differentiate between performance of controls and non-demented PD patients (Foster et al. 2014; Foster and Doty 2021), however, diagnostic accuracy for PD-MCI has not yet been reported.
Almeida et al. (2017) modified the Pfeffer Functional Activities Questionnaire (FAQ, Pfeffer et al. 1982), by including two scale items that, in the authors’ opinion, primarily reflect motor impairments (Almeida et al. 2017). For the modified version of the FAQ, a cut-off of 3.5 points has been proposed based on another validated ADL scale. The cut-off discriminates between PD patients with and without ADL limitations with a sensitivity of 47% and a specificity of 88%. A recent study developed novel ADL scores based on a data-driven approach to discriminate between motor and cognitive contributions to ADL in PD using the FAQ (Becker et al. 2020). People with PD-MCI with more cognitive than motor associated ADL problems had a higher risk of PDD conversion (Becker et al. 2022a), but the discriminatory power of the novel subscores for either PD-MCI or PDD has not yet been defined. The total FAQ score showed a moderate to low sensitivity for PD-MCI (< 55%), but a moderate to high specificity (> 54%), with a tendency of higher values for self-ratings compared to informant-ratings of ADL function (Becker et al. 2022b).
In summary, the evaluation of the potential for ADL measures to detect cognitive ADL impairment is still at its infancy. Although the diagnostic values of various assessments need to be confirmed in independent PD cohorts, there is evidence that ADL assessments have the potential to differentiate cognitive subgroups of people with PD. Of those, the PDAQ-15, the PD-CFRS, and the UPSA show sufficient diagnostic properties and accuracy for PDD and are therefore valuable ADL assessment to support cognitive diagnosis.
Cognitive correlates of ADL impairment
In cognitively mixed PD cohorts, including different cognitive PD subgroups (e.g. PD-NC, PD-MCI, and PDD; Litvan et al. 2012), lower global cognition was found to be correlated with worse self-ratings (Cholerton et al. 2020; Pirogovsky et al. 2012), worse informant-ratings (Cholerton et al. 2020; Liepelt-Scarfone et al. 2013), worse mixed self-informant ratings (Choi et al. 2019; de Oliveira et al. 2020), as well as more errors in performance-based ADL assessments of everyday problems (Foster 2014; García-Nevares et al. 2020; Giovannetti et al. 2012; Holden et al. 2018; de Oliveira et al. 2020; Pirogovsky et al. 2012, 2014; Sulzer et al. 2020). An overview of the presented results, along with the type of assessments used, is provided in Supplementary Tables 1 and 2.
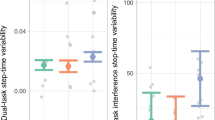
Among the range of cognitive domains, attention/working memory, executive function, and memory appear to have received the greatest attention in research, with relatively less research being published on visuo-cognitive skills and, in particular, language. Lower attention, executive functions, and memory may be related to worse self-ratings, worse informant-ratings, and worse mixed ratings of ADL function (Becker et al. 2023; Cholerton et al. 2020; Fellows and Schmitter-Edgecombe 2019; Pirogovsky et al. 2012; Puente et al. 2016). Analogously, these cognitive domains are also related to performance-based ADL assessments in people with PD, as well as visuo-cognitive skills and, although with mixed support, language function (Beyle et al. 2018; Fernández-Baizán et al. 2022; Foster and Doty 2021; Higginson et al. 2013; Giovannetti et al. 2012; Holden et al. 2020; Glonnegger et al. 2016; Manning et al. 2012; de Oliveira et al. 2020; Pirogovsky et al. 2012; Lopez et al. 2019; Puente et al. 2016; García-Nevares et al. 2020; Schmitter-Edgecombe et al. 2024). Interestingly, those patients who report spending less time per day on complex ADL tasks, indicating that they avoid or practice those challenging tasks less often, also show poorer attention and visuo-cognitive performance (Fernández-Baizán et al. 2022). In PD-MCI, attention, executive function, and memory have been found to be associated with both subjective ADL function and performance-based ADL function (Foster et al. 2022; Schmitter-Edgecombe et al. 2022; Sumida et al. 2021). Furthermore, driving performance may be primarily supported by attention, executive function, and visuo-cognitive skills (Crizzle et al. 2012; Ranchet et al. 2012). Taken together, the evidence indicates that ADL function may be supported by a broad spectrum of cognitive domains, with attention, executive function, and memory taking precedence. However, these results must be interpreted in the context of the imbalance in the literature to the detriment of visuo-cognitive skills and language.
In addition to these examinations of the relationship between ADL and cognition, several approaches have been employed to dichotomize samples based on their ADL performance. For instance, Becker et al. (2020) defined a cut-off that identified people with PD-MCI who exhibited greater cognitive than motor ADL impairment in a mixed self-informant reported ADL measure using a regression-based approach. Those scoring above the cut-off demonstrated poorer performance in both attention/working memory and language. Liepelt-Scarfone et al. (2013) found that in a cognitively mixed sample, people with PD who were reported by their informants to be more ADL impaired, performed worse in tests assessing visuo-construction and attention. Manning et al. (2012) found that non-demented people with PD who scored below 80% in a performance-based medication assessment tended to perform worse in tests assessing memory, attention, and executive function. These findings specifically highlight the role of attention/working memory in ADL function, but further research is required to establish cut-off scores.
Within the domains of attention/working memory, executive function, and memory, some functions appear to be particularly relevant for people with PD to perform their ADL adequately. Attentional performance, in particular vigilance and focused attention, is one of the strongest predictors of ADL function in PDD (Bronnick et al. 2006). In addition, the contributions of processing speed and working memory have been repeatedly emphasized (Beyle et al. 2018; Bronnick et al. 2006; Cholerton et al. 2020; Foster and Doty 2021; Fernández-Baizán et al. 2022; Glonnegger et al. 2016; Higginson et al. 2013; Manning et al. 2012). In terms of executive function, initiation, generation, and set-shifting have been highlighted as crucial skills for ADL performance (Cholerton et al. 2020; de Oliveira et al. 2020; García-Nevares et al. 2020; Glonnegger et al. 2016; Foster and Doty 2021; Lopez et al. 2019; Puente et al. 2016; Foster et al. 2022; Manning et al. 2012). Performance in immediate and delayed recall as well as content memory tasks have also been found to be stronger linked to ADL performance than other memory functions (Fellows and Schmitter-Edgecombe 2019; Sumida et al. 2021).
Given that not only memory, but also attention/working memory and executive function could potentially be the core cognitive domains to contribute to ADL performance, it seems worthwhile to consider the cognitive mechanisms that enable adequate performance of ADL tasks. One potential cognitive mechanism that modulates ADL function may be cognitive control, which relies on both attention and executive function (Diamond 2013; Hofmann et al. 2008; Miller and Wallis 2009). Cognitive control enables individuals to proactively form internal representations of goals and action plans and to maintain them in working memory (Hofmann et al. 2008). More specifically, cognitive control may play a pivotal role in the home-based environment for focusing on relevant tasks and maintaining intentions on actions amidst distractions (Buckley et al. 2014). Additionally, cognitive control allows individuals to resolve internal conflicts through the inhibition of competing interests, of temptations, and of impulses, which is also known as interference control (Aron 2011). Hence, cognitive control may play a major role in the selection, initiation, maintenance, and monitoring of ADL tasks in PD, and therefore ADL function.
Cognition and performance-based ADL assessments
The ADL domains in performance-based assessments may differ in their demands and levels of difficulty and therefore call for the use of different cognitive functions. For example, medication management and financial administration may place greater demands on executive function, attention, and memory, but place lower demands on visuo-cognitive skills and language than other ADL domains (Lopez et al. 2019; Foster and Doty 2021; Manning et al. 2012; Sulzer et al. 2020; Pirogovsky et al. 2012). Even within the same ADL domain, tasks may vary in their cognitive requirements. For example, household chores like vacuuming and folding laundry may engage different aspects of working memory (García-Nevares et al. 2020). Thus, different cognitive functions are addressed depending on which ADL domains are assessed, which could also explain why support for the role of language in performance-based ADL function is controversial (Glonnegger et al. 2016; Sumida et al. 2021). As most studies have been conducted in cognitively mixed PD cohorts, future studies investigating the relationship between cognition and ADL function in clearly defined cognitive subgroups (e.g. PD-MCI, PDD vs. normal cognition) are needed.
Apart from these findings, qualitative analyses have revealed behavioral peculiarities in the performance of ADL tasks, suggesting that cognitive ADL impairments may involve not just errors themselves, but are also characterized by a specific abnormal behavior. Cognitively impaired people with PD seem to behave inefficiently, exhibiting aimless searching (e.g., searching through the wrong cabinet), repeating actions (e.g., towel a dry dish), stopping mid-action to correct themselves (e.g., reaching for the wrong object at first, then taking the right one; known as perplexity errors), executing tasks in the wrong order, using objects and tools in wrong positions, or perseverating on certain tasks (e.g., excessive wiping of a countertop; Beyle et al. 2018; Giovannetti et al. 2012; Glonnegger et al. 2016; Schmitter-Edgecombe et al. 2022, 2024). This trial-and-error behavior may become more pronounced as cognitive impairment worsens, since people with PDD are more likely to make perplexity errors than non-demented people with PD (Beyle et al. 2018; Glonnegger et al. 2016). In PDD, ADL impairment may further expand to omission errors, where necessary task steps are skipped (Beyle et al. 2018; Glonnegger et al. 2016). Thus, the evidence indicates that cognitive ADL impairment may be indicative of a specific behavioral pattern that can be described in terms of inefficiency, trial-and-error behavior, and, in the case of PDD, task step omissions. Considering the laboratory test situation of performance-based ADL assessments, future studies should investigate how these behavioral patterns manifest in everyday life.
Novel methods to measure everyday behavior in PD
Within the surge of novel methods that enable the quantification of unsupervised behavior in everyday life, clinicians may have increased opportunities in making more informed decisions while minimizing economic resources. This is important because comparisons between supervised and unsupervised assessments have shown that laboratory performance is not identical to everyday behavior in people with PD (Corrà et al. 2021; Morgan et al. 2022; Rehman et al. 2022) raising questions about the transferability of laboratory ADL assessments to everyday behavior. Sensor-based methods may offer a solution to this problem, as they can capture impromptu movements and behavioral fluctuations in an unsupervised environment, thus providing naturalistic data. Because sensor-collected data are derived from behaviors in everyday life situations, which also represent ADL to a large extent (Alberdi Aramendi et al. 2018; Warmerdam et al. 2020), sensor-based methods may objectively and unobtrusively assess ADL function in the home-based environment (referring to any unsupervised setting in the home and in daily life; Warmerdam et al. 2020). Depending on the sensor type or the processing algorithm used, sensor-collected data can be translated into different parameters, such as physical activity, rest-activity rhythms, or in-home behavior. The following section will present results on the associations between sensor-based parameters, cognition, and ADL measures.
A commonly used sensor-based method to assesses everyday behavior is provided by accelerometers, usually worn around the hip, ankle, or wrist. Accelerometers can capture a broad range of spatial-temporal parameters of bodily behaviors, and depending on the algorithm used, can be processed to different constructs such as physical activity. Physical activity subsumes information about bodily behaviors such as sitting and lying (sedentary behaviors) or walking and standing (active behaviors; Mathie et al. 2004). Thereby, the frequency, the duration, and the metabolic demands of the bodily behaviors can be assessed, which makes it also possible to assess the pattern of physical activity (Mc Ardle et al. 2023).
Lower levels of physical activity have been linked to cognitive impairment, with the lowest levels observed in people with PDD, followed by those with PD-MCI compared to PD-NC (Cerff et al. 2017; van Uem et al. 2018). Additionally, lower levels of physical activity have been associated with self-rated ADL impairment in a cognitively mixed PD cohort (Terashi et al. 2017), and, although insignificantly, with informant-rated ADL impairment in a PDD cohort (Mc Ardle et al. 2020). Furthermore, lower global cognition, attention, and executive function have been linked to lower physical activity levels in cognitively mixed PD cohorts (Cerff et al. 2017; Donahue et al. 2022; Lamont et al. 2015; Dontje et al. 2013; Loprinzi et al. 2018; Terashi et al. 2017). A study reported that people with PD-MCI who received cognitive training increased their physical activity in comparison to an active control group, as measured by accelerometry (Bode et al. 2023). These increases were associated with improvements in executive function, indicating that those people with PD-MCI who were more physically active after the cognitive training also showed better performance in tests assessing executive functions (Bode et al. 2023). Emphasis has also been placed on the pattern of sedentary behavior. It was observed that interruptions of sedentary behaviors were less frequent in a small sample of people with PDD, who had subjectively rated ADL impairment, compared to people with PD-MCI (Cerff et al. 2017). Similarly, this sedentary pattern, indicating that sedentary bouts are more prolonged, has been linked to self-rated ADL impairment in non-PD cohorts (Chen et al. 2016; Sardinha et al. 2015; Tieges et al. 2015; Son et al. 2024). However, in people with PD-MCI, informant-rated ADL impairment was associated with a higher number of sedentary bouts (Bode et al. 2023). Interestingly, in the same cohort, prolonged sedentary bouts were associated with lower working memory (Bode et al. 2023), and prolonged sedentary bouts occurred more frequently in people with PDD than in non-demented PD (Cerff et al. 2017; van Uem et al. 2018). As explained further above, reduced physical activity could be partially due to motor-cognitive mechanisms (Ferrazzoli et al. 2018; Raffegeau et al. 2019). Accordingly, the ability to execute sit-to-stand transfers is related to self-reported ADL function in PD (Bryant et al. 2020), and falls frequently occur during sit-to-stand-transfers (Allen et al. 2013; Ashburn et al. 2008). Thus, lower physical activity levels and prolonged sedentary bouts could indicate a subjective protective strategy, where patients only get up when it is necessary (e.g. Cerff et al. 2017).
Besides physical activity, spatial-temporal parameters of bodily behaviors can also be processed to rest-activity rhythms (also referred to as „Actigraphy “). Rest-activity rhythms complement physical activity because they characterize the distribution and fragmentation of behaviors within a day (“intraday variability”) as well as the stability of behaviors between days (“Inter-day stability”; Gao et al. 2023). In cognitively normal people with PD, lower inter-day stability of physical activity was linked to lower attention, executive function, and visuo-cognitive skills (Leonard 2016; Wu et al. 2018). Additionally, greater intraday variability and lower inter-day stability were linked to cognitive impairment in non-PD cohorts (Rabinowitz et al. 2022). Lower inter-day stability was also reported to correlate with subjective ADL impairment in non-PD older adults with dementia, which needs to be confirmed in PD (Ishimaru et al. 2021; Carvalho-Bos et al. 2007). Overall, the evidence indicates that lower cognition and ADL impairment in PD are characterized by lower physical activity levels and prolonged sitting, and potentially a greater variability of rest-activity between and within days. However, studies are needed to examine which activities the patients engage in during these behaviors.
An alternative to accelerometers is provided by smart-home sensors, which can be attached to different objects within an individual’s home, such as kitchen gadgets, a washing machine, or doors. As these objects may be part of ADL scenarios, the field of smart-home research considers smart-home sensor data as direct estimate of an individual’s ADL function within their home (Yamasaki and Kumagai 2021). Different aspects of in-home behavior have been shown to reflect subjective ratings of ADL function (Alberdi et al. 2018) and performance-based ADL assessments (Suchy et al. 2020). Data obtained by pill box sensors have revealed that cognitively impaired non-PD older adults forget their medication more frequently in everyday life than cognitively normal non-PD older adults (Rawtaer et al. 2020), and medication errors have been linked to lower executive functions (Insel et al. 2006; Suchy et al. 2020). Additionally, cognitively impaired non-PD older adults tend to move less in their homes than cognitively normal non-PD older adults (Rawtaer et al. 2020; Kaye et al. 2014), to leave their homes less frequently (Wettstein et al. 2015), and to execute their ADL tasks irregularly within a day and between days (Urwyler et al. 2017). Having been interpreted to reflect disrupted and erratic routines (Lee et al. 2020), behavioral variability associated with cognitive impairment has been also reported for in-home movement, room transitions (Schütz et al. 2019), computer use (Kaye et al. 2014), walking speed (Hayes et al. 2008), and sensor patterns (Botros et al. 2022). To date, no study using smart-home sensors in people with PD could be identified. However, smart-home sensors seem to be a promising approach to get a deeper insight into patients’ home-based everyday live.
Treatment of ADL impairment associated with cognition
As the literature suggests that cognitive ADL function offers valuable insight into the integrity of cognition in real-life situations, this underscores the need for appropriate interventions focused on improving or maintaining cognitive ADL function. To date, literature with ADL function as primary outcome in clinical intervention trial is sparse. We therefore present data on various ADL assessments and their potential to reflect treatment effects.
Pharmacological treatment
No pharmacological treatments are yet available to improve both cognition and ADL function, or either alone, in PD-MCI. Current evidence is insufficient to recommend the use of memantine (Kawashima et al. 2022) and Acetylcholinesterase inhibitors (AChEIs, Baik et al. 2021; Mamikonyan et al. 2015; Sawada et al. 2018, 2021) in PD-MCI. In contrast, positive treatment effects of rivastigmine and donepezil for global cognitive state, memory, and speech have been reported in PDD (Brennan et al. 2016a; McShane et al. 2019; Matsunaga et al. 2015; Pagano et al. 2015; Rolinski et al. 2012). The effects of AChEIs treatments on ADL in PDD are controversially discussed. On the one hand, a meta-analysis supports a positive effect of donepezil compared to placebo for the improvement of ADL function (Matsunaga et al. 2015). On the other hand, no beneficial effect of AChEIs on ADL function in PDD could be identified (Pagano et al. 2015). In addition, discontinuation of AChEIs may have little or no effect on ADL status in the short term (Matsunaga et al. 2015; Parsons et al. 2021), and there are currently insufficient data to assess the long-term effect of AChEI on ADL function in people with dementia.
Non-invasive non-pharmacological intervention
The value of non-pharmacological interventions for the treatment of cognitive impairment in PD is increasingly recognized, but their effect on cognitive ADL function has been addressed less often. Cognitive training, physiotherapy, and occupational therapy have been proven to improve cognition and motor skills in people with PD (Clarke et al. 2016; Leung et al. 2015). A meta-analysis, including eight studies (n = 485 people with PD) confirmed that moderate exercise interventions containing functional-task training had a positive effect on the UPDRS-II (Perry et al. 2019). It has also been suggested that virtual reality (Lina et al. 2020) and occupational therapy (Foster et al. 2021) have the potential to improve ADL function in PD, although the number of studies investigating these issues is limited.
Table 2 summarizes effects of non-pharmacological randomized controlled trials (RCTs) with an active control group and ADL as an outcome. Additionally, Table 2 lists study characteristics that allow for the evaluation of these RCTs conducted with greater scientific quality for a specific treatment effect on ADL function. An analogous summary of RCTs with an active control group is provided in Supplementary Table 3. In summary, only the minority of studies with an active and passive control group defined treatment induced change in ADL as primary outcome (da Silva et al. 2023; Daley et al. 2014; Foster et al. 2013; Frazzitta et al. 2012; Pompeu et al. 2012). Effective physical RCTs with an active control group applied aerobic training (Burini et al. 2006; Schenkman et al. 2012), physical therapy (Dereli and Yaliman 2010), resistance training and fall education, movement strategy training (Morris et al. 2015; King et al. 2015), postural breathing exercises (Paolucci et al. 2017), balance trainings (Volpe et al. 2014), and walking coordination trainings (Zhu et al. 2018). Combined interventions, consisting of multiple elements such as cognitive, motor training, occupational therapy, or psychomotor exercises, have been shown to provide benefits for ADL function (Sousa et al. 2021; Pedreira et al. 2013; Palamara et al. 2017), greater than either alone or than less demanding interventions (Choi and Cho 2022; Monticone et al. 2015; Pompeu et al. 2012; Tamir et al. 2007). So far, only one study revealed a positive effect of cognitive training vs. an active control group on ADL (Peña et al. 2014). Treatment duration varies between 30 (Ribas et al. 2017; Pompeu et al. 2012) and 120 (Morris et al. 2015) minutes in RCTs with active control group, and the weekly treatment frequencies are highly variable between studies. A variety of studies used the UPDRS-II as study outcome (Burini et al. 2006; Dereli and Yaliman 2010; King et al. 2015; Morris et al. 2015; Paolucci et al. 2017; Schenkman et al. 2012; Tamir et al. 2007; Volpe et al. 2014; Zhu et al. 2018; Pompeu et al. 2012) and did not correct their statistical analyses for the influence of motor impairment, albeit the UPDRS-II is confounded by such. Only few of the identified RCTs with active control group included more than 30 persons per active control group (Monticone et al. 2015; Morris et al. 2015; Schenkman et al. 2012; Choi and Cho 2022). Most important, people with PDD were excluded in nearly all non-pharmacological intervention trials (Folkerts et al. 2018), thus the evaluation of treatment effects is limited to people without dementia. To date, only some studies investigate treatment effects in homogenous groups of people with PD-MCI (Kalbe et al. 2020), so more studies are needed to evaluate treatment effects on ADL in distinct cognitive subgroups.
Interventional studies in non-PD older adults with MCI may offer insights into the positive impact of ADL trainings as a future directive to prevent further ADL decline in the prodromal phase of PDD, namely PD-MCI. These studies demonstrate that interventions, such as cognitive trainings, cognitive rehabilitation, multi-domain trainings, and everyday problem-solving strategy trainings improve ADL performance compared to control groups (Schmitter-Edgecombe and Dyck 2014; Park 2022; Chandler et al. 2016; Tulliani et al. 2022). Moreover, the training impact is not limited to the improvements in ADL performance but also positively affects cognitive functioning, especially executive and memory function (Park 2022; Schmitter-Edgecombe et al. 2022). Therefore, findings in non-PD cohorts suggest that an ADL training may effectively improve IADL function of people with PD-MCI. Home-based digital CTs are increasingly tested as innovative strategies to improve cognition in patients with limited access to healthcare facilities due to disabilities such as traveling difficulties (Biundo et al. 2017). Digital CTs have been shown to improve cognition as assessed by cognitive tests (Gavelin et al. 2022), but their positive effect on ADL either short- or long-term and, accordingly, its potential to prevent PDD has not been investigated yet.
Discussion and conclusion
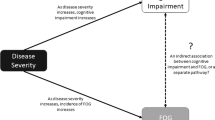
ADL function can be viewed as a multifaceted construct that reflects functionality in different daily life situations, and therefore provides clinicians comprehensive insight into their patient’s overall health and well-being. The assessment of ADL function is crucial for cognitive diagnosis: The core feature that differentiates PDD from PD-MCI is the loss of the ability to perform ADL tasks that are necessary for independent living due to cognitive deterioration (Dubois et al. 2007). Because motor and non-motor symptoms of people with PD can impact their ADL function, clinicians should carefully assess the primary factor that contributes to a patient’s ADL impairment, as far as possible. Assessing ADL tasks that are primarily reliant on cognition could enhance the precision of diagnostic procedures because these tasks indicate how cognitive skills are used in real-world scenarios embedded within a context-rich environment. To that end, however, more systematic examinations are required, for which a proper nomenclature for the multifaceted construct of ADL is necessary. Therefore, we here introduce the concept of cognitive ADL impairment (see Fig. 1), which reflects problems in everyday life due to cognitive deterioration.
This figure depicts the conceptualization of cognitive ADL. Cognitive ADL function refers to the functionality in everyday behaviors that are associated with cognition. These behaviors can be observed in a laboratory environment, measured with performance-based ADL assessments, or measured in the home-based environment (referring to any unsupervised setting in the home and in daily life) with sensor-collected data. Rating scales may represent an overlap of these two observational situations, as raters may draw from their observations in everyday life to respond to a laboratory assessment. Different factors, which partially overlap, may be associated with these ADL assessments, including cognitive factors (with attention, executive function, and memory being particularly important) and other factors
Impairment in IADL tasks is reported in about 30% to 50% of people with PD-MCI (Glonnegger et al. 2016; Martin et al. 2013). Importantly, those people with PD-MCI who display exclusive impairment in IADL that place greater demands on cognition are at an increased risk to develop PDD within three years (Becker et al. 2022a). Therefore, people with PD-MCI and cognitive ADL impairment should be considered an important target group for pharmacological and non-pharmacological interventions that maintain or improve their everyday life.
Currently, we face several challenges in research on effective interventions targeting cognitive ADL impairment. Firstly, the diagnostic properties of clinical instruments to assess cognitive ADL impairment are still insufficiently explored and existing data need to be verified in larger samples. It must be acknowledged that the views of patients and their informants may be confounded by several biases, with particular caution regarding those biases conflicting with the assessment of cognitive dysfunction. Sensor-based assessments could offer a novel approach to objectively assess ADL function in terms of manifest behavior. Nevertheless, ADL rating scales offer the advantage that they synthesize multiple observations from everyday life over an extended time period in comparison to the patient’s premorbid ability. Therefore, the results of subjective ADL assessments may be of value for the screening of everyday problems, which practitioners should then explore in detail in a patient- and/or caregiver-centered interview. Secondly, knowledge of the time course of cognitive ADL impairment in people with PD is sparse. Prospective longitudinal studies that examine the onset and the severity of ADL impairment in the prodromal phase of PDD are urgently needed to understand the causal relationship between ADL impairment and cognitive worsening.
Our construct of cognitive ADL function may provide a framework for research that aims to enhance the accuracy of diagnostic methods. While new ADL assessments could be developed, existing ADL scales could be extended or adapted as well. For example, total scores for cognitive ADL function might only include cognitive ADL items, or adjusted cognitive ADL scores may weight each ADL item depending on their cognitive demands. Another approach could be to modify items of existing scales to ask for the primary cause for a patient’s difficulties. First evidence supports that informants attribute different sources to the patient's difficulties in an ADL task (Benge and Balsis 2016). Nevertheless, it remains a challenge to disentangle patients’ and caregivers’ ADL ratings from the different biases affecting their responses (e.g., Caap-Ahlgren and Dehlin 2002; Ransmayr 2020). More studies are needed to get further insight how to minimize the biases of ratings of everyday skills.
Although a broad range of cognitive functions may be implicated in the ADL function of people with PD, attention, executive functions, and memory are most consistently highlighted in the current body of research (Holden et al. 2020; Sulzer et al. 2020; Cholerton et al. 2020). However, future research must strive to equilibrate the imbalance in literature for the examination of the role of language and visuo-cognition. Several mechanisms, such as cognitive control or mechanisms associated with memory, may be at play in the establishment of these relationships. Longitudinal studies and experimental paradigms are necessary to understand the specific cognitive mechanisms that link cognition and ADL function. With such an understanding, it will be possible to provide effective interventions that are precisely tailored to the specific causes of a patient’s cognitive ADL impairment, thereby improving patient-centered medical care.
Based on studies that have used performance-based ADL assessments, it can be inferred that ADL impairment associated with cognition may be characterized by a specific error profile (Beyle et al. 2018; Glonnegger et al. 2016; Schmitter-Edgecombe et al. 2022). Future studies using smart-home sensors might lead to a deeper understanding of patients’ everyday behavior, but such studies are not yet available. As performance-based ADL assessments are time consuming and involve a high level of material expenditure, digital assessments targeting the characteristic behavior of people with PD might be helpful to detect cognitive ADL impairment at its early stage.
Therefore, monitoring the home-based behavior of people with PD might be a future directive to get an ecologically valid insight into patients’ everyday life. On the one hand, cognitive ADL impairment may be characterized by lower engagement in everyday behaviors, as suggested by physical activity levels, prolonged sedentary behavior, and in-home behavior (Terashi et al. 2017; Cerff et al. 2017; Rawtaer et al. 2020). On the other hand, cognitive ADL impairment may be characterized by a high variability within and between days, which is impossible to detect with one-time clinical assessments (Urwyler et al. 2017; Ishimaru et al. 2021). More effort is warranted to understand the relationship between these behavioral aspects and their subjective experience by patients and informants with ADL function and cognition, as there appears to be a gap between subjective and objective measures (Foster and Hershey 2011; Puente et al. 2016; Vlagsma et al. 2017).
Physical, cognitive, and multi-domain interventions can improve ADL function in PD. Unfortunately, the ADL measures used as outcomes in currently available RCTs are often confounded by motor performance (Lee et al. 2014; Skinner et al. 2015; Rosenthal et al. 2010). Further non-pharmacological blinded RCTs in large multicenter studies with cognitive ADL function as the primary outcome are needed to fully recognize the benefit of preventing or delaying the worsening of cognitive ADL impairment in the prodromal phase of PDD. These interventions should be specifically targeted on cognitive ADL function, as this may be an even more important outcome than laboratory-assessed cognition. Cognitive ADL tasks often involve open-ended activities in distracting environments, unlike the structured cognitive tests conducted in quiet laboratory conditions. Additionally, cognitive ADL tasks might require multiple cognitive functions simultaneously, contrasting with traditional cognitive tests which assess one cognitive function at a time. Most importantly, people with PD have a strong desire to maintain their autonomy and their self-reliance (Haahr et al. 2011), while dreading becoming dependent on others and burdening their loved ones (Vann-Ward et al. 2017). Therefore, enhancing cognitive ADL function aligns directly with meeting the patients' needs. In this regard, home-based digital trainings offer an innovative and self-reliance-promoting strategy to improve cognition and cognitive ADL function in patients with difficulties in travelling, which limits patients’ access to healthcare facilities (Zaman et al. 2021).
In conclusion, there is a great need for ADL assessments and ADL treatments specifically designed to target cognitive ADL impairment in PD. Early detection and treatment of cognitive ADL impairment shows great potential to delay or prevent dementia conversion in people with PD and enhancing the quality of life for patients and caregivers.
Data availability
Data sharing is not available for this article as no original datasets were generated or analyzed for this narrative review.
References
Aarsland D, Batzu L, Halliday GM, Geurtsen GJ, Ballard C, Ray Chaudhuri K, Weintraub D (2021) Parkinson disease-associated cognitive impairment. Nat Rev Dis Primers 7(1):47. https://doi.org/10.1038/s41572-021-00280-3
Ahn S, Springer K, Gibson JS (2022) Social withdrawal in Parkinson’s disease: a scoping review. Geriatr Nurs 48:258–268. https://doi.org/10.1016/j.gerinurse.2022.10.010
Alberdi A, Weakley A, Schmitter-Edgecombe M, Cook DJ, Aztiria A, Basarab A, Barrenechea M (2018) Smart Home-Based Prediction of Multidomain Symptoms Related to Alzheimer’s Disease. IEEE J Biomed Health Inform 22(6):1720–1731. https://doi.org/10.1109/JBHI.2018.2798062
Alberdi Aramendi A, Weakley A, Aztiria Goenaga A, Schmitter-Edgecombe M, Cook DJ (2018) Automatic assessment of functional health decline in older adults based on smart home data. J Biomed Inform 81:119–130. https://doi.org/10.1016/j.jbi.2018.03.009
Allan L, McKeith I, Ballard C, Kenny RA (2006) The prevalence of autonomic symptoms in dementia and their association with physical activity, activities of daily living and quality of life. Dement Geriatr Cogn Disord 22(3):230–237. https://doi.org/10.1159/00009497110.1159/000094971
Allen NE, Schwarzel AK, Canning CG (2013) Recurrent falls in Parkinson’s disease: a systematic review. Parkinsons Dis 2013:906274. https://doi.org/10.1155/2013/906274
Almeida KJ, de Macedo LP, de Melo L, Lobo Jofili Lopes J, Bor-Seng-Shu E, Campos-Sousa RN, Barbosa ER (2017) Modified Pfeffer Questionnaire for Functional Assessment in Parkinson Disease. J Geriatr Psychiatry Neurol 30(5):261–266. https://doi.org/10.1177/0891988717720298
Altmann LJ, Troche MS (2011) High-level language production in Parkinson’s disease: a review. Parkinson’s Disease 2011:238956. https://doi.org/10.4061/2011/238956
Aron AR (2011) From reactive to proactive and selective control: developing a richer model for stopping inappropriate responses. Biol Psychiat 69(12):e55–e68. https://doi.org/10.1016/j.biopsych.2010.07.024
Ashburn A, Stack E, Ballinger C, Fazakarley L, Fitton C (2008) The circumstances of falls among people with Parkinson’s disease and the use of Falls Diaries to facilitate reporting. Disabil Rehabil 30(16):1205–1212. https://doi.org/10.1080/09638280701828930
Atrsaei A, Hansen C, Elshehabi M, Solbrig S, Berg D, Liepelt-Scarfone I, Maetzler W, Aminian K (2021) Effect of Fear of Falling on Mobility Measured During Lab and Daily Activity Assessments in Parkinson’s Disease. Front Aging Neurosci 13:722830. https://doi.org/10.3389/fnagi.2021.722830
Baik K, Kim SM, Jung JH, Lee YH, Chung SJ, Yoo HS, Ye BS, Lee PH, Sohn YH, Kang SW, Kang SY (2021) Donepezil for mild cognitive impairment in Parkinson’s disease. Sci Rep 11(1):4734. https://doi.org/10.1038/s41598-021-84243-4
Becker S, Baumer A, Maetzler W, Nussbaum S, Timmers M, Van Nueten L, Salvadore G, Zaunbrecher D, Roeben B, Brockmann K, Streffer J, Berg D, Liepelt-Scarfone I (2020) Assessment of cognitive-driven activity of daily living impairment in non-demented Parkinson’s patients. J Neuropsychol 14(1):69–84. https://doi.org/10.1111/jnp.12173
Becker S, Boettinger O, Sulzer P, Hobert MA, Brockmann K, Maetzler W, Berg D, Liepelt-Scarfone I, Alzheimer’s Disease Neuroimaging I (2021) Everyday function in Alzheimer’s and Parkinson’s patients with mild cognitive impairment. J Alzheimers Dis 79(1):197–209. https://doi.org/10.3233/JAD-200256
Becker S, Bode M, Brockmann K, Gasser T, Michaelis K, Solbrig S, Nuerk HC, Schulte C, Maetzler W, Zimmermann M, Berg D, Liepelt-Scarfone I (2022a) Cognitive-Driven Activities of Daily Living Impairment as a Predictor for Dementia in Parkinson Disease: A Longitudinal Cohort Study. Neurology 99(23):e2548-2560. https://doi.org/10.1212/WNL.0000000000201201
Becker S, Pauly C, Lawton M, Hipp G, Bowring F, Sulzer P, Hu M, Kruger R, Gasser T, Liepelt-Scarfone I (2022b) Quantifying activities of daily living impairment in Parkinson’s disease using the functional activities questionnaire. Neurol Sci 43(2):1047–1054. https://doi.org/10.1007/s10072-021-05365-1
Becker S, Solbrig S, Michaelis K, Faust B, Brockmann K, Liepelt-Scarfone I (2022c) Divergence between informant and self-ratings of activities of daily living impairments in Parkinson’s disease. Front Aging Neurosci 14:838674. https://doi.org/10.3389/fnagi.2022.838674
Becker S, Maarouf N, Kibreab M, Hammer T, Kathol I, Monchi O, Callahan BL (2023) 66 Association of executive functions and instrumental activities of daily living in Parkinson’s disease. J Int Neuropsychol Soc 29(s1):576–577. https://doi.org/10.1017/s1355617723007373
Behnke S, Double KL, Duma S, Broe GA, Guenther V, Becker G, Halliday GM (2007) Substantia nigra echomorphology in the healthy very old: correlation with motor slowing. Neuroimage 34(3):1054–1059. https://doi.org/10.1016/j.neuroimage.2006.10.010
Benge JF, Balsis S (2016) Informant Perceptions of the Cause of Activities of Daily Living Difficulties in Parkinson’s Disease. Clin Neuropsychol 30(1):82–94. https://doi.org/10.1080/13854046.2015.1136690
Berg D, Marek K, Ross GW, Poewe W (2012) Defining at-risk populations for Parkinson’s disease: lessons from ongoing studies. Movement Disorders Clinical Practice 27(5):656–665. https://doi.org/10.1002/mds.24985
Beyle A, Glonnegger H, Cerff B, Graber S, Berg D, Liepelt-Scarfone I (2018) The Multiple Object Test as a performance-based tool to assess the decline of ADL function in Parkinson’s disease. PLoS ONE 13(8):e0200990. https://doi.org/10.1371/journal.pone.0200990
Bezdicek O, Mana J, Ruzicka F, Havlik F, Fecikova A, Uhrova T, Ruzicka E, Urgosik D, Jech R (2022) The Instrumental activities of daily living in Parkinson’s disease patients treated by subthalamic deep brain stimulation. Front Aging Neurosci 14:886491. https://doi.org/10.3389/fnagi.2022.886491
Bezdicek O, Ferreira J, Fellows R, Liepelt-Scarfone I (2023) Editorial: Activities of daily living and everyday functioning: from normal aging to neurodegenerative diseases. Front Aging Neurosci 15:1161736. https://doi.org/10.3389/fnagi.2023.1161736
Bin Yoo H, Concha EO, De Ridder D, Pickut BA, Vanneste S (2018) The Functional Alterations in Top-Down Attention Streams of Parkinson’s disease Measured by EEG. Sci Rep 8(1):10609. https://doi.org/10.1038/s41598-018-29036-y
Biundo R, Weis L, Fiorenzato E, Antonini A (2017) Cognitive rehabilitation in Parkinson’s disease: is it feasible? Arch Clin Neuropsychol 32(7):840–860. https://doi.org/10.1093/arclin/acx092
Bjornestad A, Pedersen KF, Tysnes OB, Alves G (2017) Clinical milestones in Parkinson’s disease: A 7-year population-based incident cohort study. Parkinsonism Relat Disord 42:28–33. https://doi.org/10.1016/j.parkreldis.2017.05.025
Bode M, Sulzer P, Schulte C, Becker S, Brockmann K, Elben S, Folkerts AK, Ophey A, Schlenstedt C, Witt K, Wojtecki L, Evers J, Maetzler W, Kalbe E, Liepelt-Scarfone I (2023) Parkinsonism Relat Disord 113:105330. https://doi.org/10.1016/j.parkreldis.2023.105330
Botros AA, Schuetz N, Rocke C, Weibel R, Martin M, Muri RM, Nef T (2022) Eigenbehaviour as an Indicator of Cognitive Abilities. Sensors (basel) 22(7):2769. https://doi.org/10.3390/s22072769
Brennan L, Pantelyat A, Duda JE, Morley JF, Weintraub D, Wilkinson JR, Moberg PJ (2016a) Memantine and cognition in Parkinson’s disease dementia/dementia with Lewy bodies: a meta-analysis. Mov Disord Clin Pract 3(2):161–167. https://doi.org/10.1002/mdc3.12264
Brennan L, Siderowf A, Rubright JD, Rick J, Dahodwala N, Duda JE, Hurtig H, Stern M, Xie SX, Rennert L, Karlawish J, Shea JA, Trojanowski JQ, Weintraub D (2016b) Development and initial testing of the Penn Parkinson’s Daily Activities Questionnaire. Mov Disord 31(1):126–134. https://doi.org/10.1002/mds.26339
Brennan L, Siderowf A, Rubright JD, Rick J, Dahodwala N, Duda JE, Hurtig H, Stern M, Xie SX, Rennert L, Karlawish J, Shea JA, Trojanowski JQ, Weintraub D (2016c) The Penn Parkinson’s Daily Activities Questionnaire-15: Psychometric properties of a brief assessment of cognitive instrumental activities of daily living in Parkinson’s disease. Parkinsonism Relat Disord 25:21–26. https://doi.org/10.1016/j.parkreldis.2016.02.020
Bronnick K, Ehrt U, Emre M, De Deyn PP, Wesnes K, Tekin S, Aarsland D (2006) Attentional deficits affect activities of daily living in dementia-associated with Parkinson’s disease. J Neurol Neurosurg Psychiatry 77(10):1136–1142. https://doi.org/10.1136/jnnp.2006.093146
Bruderer-Hofstetter M, Sikkes SAM, Munzer T, Niedermann K (2020) Development of a model on factors affecting instrumental activities of daily living in people with mild cognitive impairment - a Delphi study. BMC Neurol 20(1):264. https://doi.org/10.1186/s12883-020-01843-9
Bryant MS, Kang GE, Protas EJ (2020) Relation of chair rising ability to activities of daily living and physical activity in Parkinson’s disease. Arch Physiother 10(1):22. https://doi.org/10.1186/s40945-020-00094-8
Buckley J, Cohen JD, Kramer AF, McAuley E, Mullen SP (2014) Cognitive control in the self-regulation of physical activity and sedentary behavior. Front Hum Neurosci 8:747. https://doi.org/10.3389/fnhum.2014.00747
Burini D, Farabollini B, Iacucci S, Rimatori C, Riccardi G, Capecci M, Ceravolo MG (2006) A randomised controlled cross-over trial of aerobic training versus Qigong in advanced Parkinson’s disease. Eura Medicophys 42(3):231–238
Caap-Ahlgren M, Dehlin O (2002) Factors of importance to the caregiver burden experienced by family caregivers of Parkinson’s disease patients. Aging Clin Exp Res 14(5):371–377. https://doi.org/10.1007/BF03324464
Cain AE, Depp CA, Jeste DV (2009) Ecological momentary assessment in aging research: a critical review. J Psychiatr Res 43(11):987–996. https://doi.org/10.1016/j.jpsychires.2009.01.014
Carlisle TC, Fought AJ, Olson KE, Lopez-Esquibel N, Simpson A, Medina LD, Holden SK (2023) Original research: longitudinal evaluation of cognitively demanding daily function using performance-based functional assessment highlights heterogeneous trajectories in cognitive and functional abilities in people with Parkinson’s disease. Front Neurosci 17:1200347. https://doi.org/10.3389/fnins.2023.1200347
Carlson MC, Fried LP, Xue QL, Tekwe C, Brandt J (2005) Validation of the Hopkins Medication Schedule to identify difficulties in taking medications. J Gerontol A Biol Sci Med Sci 60(2):217–223. https://doi.org/10.1093/gerona/60.2.217
Carvalho-Bos SS, Riemersma-van Der Lek RF, Waterhouse J, Reilly T, Van Someren EJW (2007) Strong association of the rest-activity rhythm with well-being in demented elderly women. Am J Geriatr Psychiatry 15(2):92–100. https://doi.org/10.1097/01.JGP.0000236584.03432.dc
Cerff B, Maetzler W, Sulzer P, Kampmeyer M, Prinzen J, Hobert MA, Blum D, van Lummel R, Del Din S, Graber S, Berg D, Liepelt-Scarfone I (2017) Home-based physical behavior in late stage Parkinson disease dementia: differences between cognitive subtypes. Neurodegener Dis 17(4–5):135–144. https://doi.org/10.1159/000460251
Chahine LM, Weintraub D, Hawkins KA, Siderowf A, Eberly S, Oakes D, Seibyl J, Stern MB, Marek K, Jennings D (2015) Cognition in individuals at risk for Parkinson’s: Parkinson associated risk syndrome (PARS) study findings. Mov Disord 31(1):86–94. https://doi.org/10.1002/mds.26373
Chandler MJ, Park AC, Marsiske M, Rotblatt LJ, Smith GE (2016) Everyday Impact of Cognitive Interventions in Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Neuropsychol Rev 26(3):225–251. https://doi.org/10.1007/s11065-016-9330-4
Chen T, Narazaki K, Haeuchi Y, Chen S, Honda T, Kumagai S (2016) Associations of Sedentary Time and Breaks in Sedentary Time With Disability in Instrumental Activities of Daily Living in Community-Dwelling Older Adults. J Phys Act Health 13(3):303–309. https://doi.org/10.1123/jpah.2015-0090
Cheon S-M, Park KW, Kim JW (2015) Identification of daily activity impairments in the diagnosis of Parkinson disease dementia. Cogn Behav Neurol 28(4):220–228. https://doi.org/10.1097/WNN.0000000000000081
Choi HS, Cho SH (2022) Effects of Multimodal Rehabilitation on the Activities of Daily Living, Quality of Life, and Burden of Care for Patients with Parkinson’s Disease: A Randomized Control Study. Healthcare (basel) 10(10):1888. https://doi.org/10.3390/healthcare10101888
Choi SM, Yoon GJ, Jung HJ, Kim BC (2019) Analysis of characteristics affecting instrumental activities of daily living in Parkinson’s disease patients without dementia. Neurol Sci 40(7):1403–1408. https://doi.org/10.1007/s10072-019-03860-0
Cholerton B, Poston KL, Tian L, Quinn JF, Chung KA, Hiller AL, Hu SC, Specketer K, Montine TJ, Edwards KL, Zabetian CP (2020) Participant and study partner reported impact of cognition on functional activities in Parkinson’s disease. Mov Disord Clin Pract 7(1):61–69. https://doi.org/10.1002/mdc3.12870
Christ JB, Fruhmann Berger M, Riedl E, Prakash D, Csoti I, Molt W, Graber S, Brockmann K, Berg D, Liepelt-Scarfone I (2013) How precise are activities of daily living scales for the diagnosis of Parkinson’s disease dementia? A Pilot Study Parkinsonism Relat Disord 19(3):371–374. https://doi.org/10.1016/j.parkreldis.2012.11.004
Citro S, Lazzaro GD, Cimmino AT, Giuffre GM, Marra C, Calabresi P (2024) A multiple hits hypothesis for memory dysfunction in Parkinson disease. Nat Rev Neurol 20(1):50–61. https://doi.org/10.1038/s41582-023-00905-z
Clarke CE, Patel S, Ives N, Rick CE, Dowling F, Woolley R, Wheatley K, Walker MF, Sackley CM, Group PRC (2016) Physiotherapy and Occupational Therapy vs No Therapy in Mild to Moderate Parkinson Disease: A Randomized Clinical Trial. JAMA Neurol 73(3):291–299. https://doi.org/10.1001/jamaneurol.2015.4452
Corrà MF, Atrsaei A, Sardoreira A, Hansen C, Aminian K, Correia M, Vila-Cha N, Maetzler W, Maia L (2021) Comparison of Laboratory and Daily-Life Gait Speed Assessment during ON and OFF States in Parkinson’s Disease. Sensors (basel) 21(12):3974. https://doi.org/10.3390/s21123974
Crizzle AM, Classen S, Uc EY (2012) Parkinson disease and driving: an evidence-based review. Neurology 79(20):2067–2074. https://doi.org/10.1212/WNL.0b013e3182749e95
da Silva AZ, Iucksch DD, Israel VL (2023) Aquatic dual-task training and its relation to motor functions, activities of daily living, and quality of life of individuals with Parkinson’s disease: a randomized clinical trial. Health Serv Insights 16:11786329231180768. https://doi.org/10.1177/11786329231180768
Daley DJ, Deane KH, Gray RJ, Clark AB, Pfeil M, Sabanathan K, Worth PF, Myint PK (2014) Adherence therapy improves medication adherence and quality of life in people with Parkinson’s disease: a randomised controlled trial. Int J Clin Pract 68(8):963–971. https://doi.org/10.1111/ijcp.12439
Darweesh SK, Verlinden VJ, Stricker BH, Hofman A, Koudstaal PJ, Ikram MA (2017a) Trajectories of prediagnostic functioning in Parkinson’s disease. Brain 140(2):429–441. https://doi.org/10.1093/brain/aww291
Darweesh SKL, Wolters FJ, Postuma RB, Stricker BH, Hofman A, Koudstaal PJ, Ikram MK, Ikram MA (2017b) Association Between Poor Cognitive Functioning and Risk of Incident Parkinsonism. JAMA Neurol 74(12):1431–1438. https://doi.org/10.1001/jamaneurol.2017.2248
de Oliveira GSR, Bressan L, Balarini F, Jesuino ESRS, Brito M, Foss MP, Santos-Lobato BL, Tumas V (2020) Direct and indirect assessment of functional abilities in patients with Parkinson’s disease transitioning to dementia. Dement Neuropsychol 14(2):171–177. https://doi.org/10.1590/1980-57642020dn14-020011
Deck BL, Xie SX, Choi G, Rick J, Siderowf A, Rudovsky S, Chen-Plotkin A, Duda JE, Morley JF, Dahodwala N, Trojanowski JQ, Weintraub D (2019) Cognitive Functional Abilities in Parkinson’s Disease: Agreement Between Patients and Informants. Mov Disord Clin Pract 6(6):440–445. https://doi.org/10.1002/mdc3.12781
Dereli EE, Yaliman A (2010) Comparison of the effects of a physiotherapist-supervised exercise programme and a self-supervised exercise programme on quality of life in patients with Parkinson’s disease. Clin Rehabil 24(4):352–362. https://doi.org/10.1177/0269215509358933
Diamond A (2013) Executive functions. Annu Rev Psychol 64:135–168. https://doi.org/10.1146/annurev-psych-113011-143750
Dirnberger G, Jahanshahi M (2013) Executive dysfunction in Parkinson’s disease: a review. J Neuropsychol 7(2):193–224. https://doi.org/10.1111/jnp.12028
Donahue EK, Venkadesh S, Bui V, Tuazon AC, Wang RK, Haase D, Foreman RP, Duran JJ, Petkus A, Wing D, Higgins M, Holschneider DP, Bayram E, Litvan I, Jakowec MW, Van Horn JD, Schiehser DM, Petzinger GM (2022) Physical activity intensity is associated with cognition and functional connectivity in Parkinson’s disease. Parkinsonism Relat Disord 104:7–14. https://doi.org/10.1016/j.parkreldis.2022.09.005
Dontje ML, de Greef MH, Speelman AD, van Nimwegen M, Krijnen WP, Stolk RP, Kamsma YP, Bloem BR, Munneke M, van der Schans CP (2013) Quantifying daily physical activity and determinants in sedentary patients with Parkinson’s disease. Parkinsonism Relat Disord 19(10):878–882. https://doi.org/10.1016/j.parkreldis.2013.05.014
Dubois B, Burn D, Goetz C, Aarsland D, Brown RG, Broe GA, Dickson D, Duyckaerts C, Cummings J, Gauthier S, Korczyn A, Lees A, Levy R, Litvan I, Mizuno Y, McKeith IG, Olanow CW, Poewe W, Sampaio C, Tolosa E, Emre M (2007) Diagnostic procedures for Parkinson’s disease dementia: recommendations from the movement disorder society task force. Mov Disord 22(16):2314–2324. https://doi.org/10.1002/mds.21844
Dujardin K, Dubois B, Tison F, Durif F, Bourdeix I, Pere JJ, Duhamel A, Group Es (2010) Parkinson’s disease dementia can be easily detected in routine clinical practice. Mov Disord 25(16):2769–2776. https://doi.org/10.1002/mds.23391
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, Broe GA, Cummings J, Dickson DW, Gauthier S, Goldman J, Goetz C, Korczyn A, Lees A, Levy R, Litvan I, McKeith I, Olanow W, Poewe W, Quinn N, Sampaio C, Tolosa E, Dubois B (2007) Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 22(12):1689–1707. https://doi.org/10.1002/mds.21507
Fellows RP, Schmitter-Edgecombe M (2019) Multimethod assessment of everyday functioning and memory abilities in Parkinson’s disease. Neuropsychology 33(2):169–177. https://doi.org/10.1037/neu0000505
Fengler S, Liepelt-Scarfone I, Brockmann K, Schaffer E, Berg D, Kalbe E (2017) Cognitive changes in prodromal Parkinson’s disease: a review. Mov Disord 32(12):1655–1666. https://doi.org/10.1002/mds.27135
Fernández-Baizán C, García-Nevares A, Díaz-Cáceres E, Menéndez-González M, Arias JL, Méndez M (2022) Activities of daily living in Parkinson disease: are they related to short term and working memory and visuospatial abilities? Topics in Geriatric Rehabilitation 38(4):285–295. https://doi.org/10.1097/TGR.0000000000000376
Ferrazzoli D, Ortelli P, Madeo G, Giladi N, Petzinger GM, Frazzitta G (2018) Basal ganglia and beyond: the interplay between motor and cognitive aspects in Parkinson’s disease rehabilitation. Neurosci Biobehav Rev 90:294–308. https://doi.org/10.1016/j.neubiorev.2018.05.007
Folkerts AK, Dorn ME, Roheger M, Maassen M, Koerts J, Tucha O, Altgassen M, Sack AT, Smit D, Haarmann L, Kalbe E (2018) Cognitive stimulation for individuals with Parkinson’s disease dementia living in long-term care: preliminary data from a randomized crossover pilot study. Parkinsons Dis 2018:8104673. https://doi.org/10.1155/2018/8104673
Foster ER (2014) Instrumental activities of daily living performance among people with Parkinson’s disease without dementia. Am J Occup Ther 68(3):353–362. https://doi.org/10.5014/ajot.2014.010330
Foster ER, Doty T (2021) Cognitive correlates of instrumental activities of daily living performance in Parkinson disease without dementia. Arch Rehabil Res Clin Transl 3(3):100138. https://doi.org/10.1016/j.arrct.2021.100138
Foster ER, Hershey T (2011) Everyday Executive Function is Associated with Activity Participation in Parkinson Disease without Dementia. OTJR (thorofare N J). 31(1):16–22. https://doi.org/10.3928/15394492-20101108-04
Foster ER, Golden L, Duncan RP, Earhart GM (2013) Community-based argentine tango dance program is associated with increased activity participation among individuals with Parkinson’s disease. Arch Phys Med Rehabil 94(2):240–249. https://doi.org/10.1016/j.apmr.2012.07.028
Foster ER, Carson LG, Archer J, Hunter EG (2021) Occupational therapy interventions for instrumental activities of daily living for adults with Parkinson’s disease: a systematic review. Am J Occup Ther 75(3):7503190031. https://doi.org/10.5014/ajot.2021.046581
Foster ER, Carson L, Jonas J, Kang E, Doty T, Toglia J (2022) The weekly calendar planning activity to assess functional cognition in Parkinson disease. OTJR (thorofare N j) 42(4):315–323. https://doi.org/10.1177/15394492221104075
Foubert-Samier A, Helmer C, Le Goff M, Guillet F, Proust-Lima C, Jacqmin-Gadda H, Dartigues JF, Amieva H, Tison F (2020) Cognitive and functional changes in prediagnostic phase of Parkinson disease: a population-based study. Parkinsonism Relat Disord 79:40–46. https://doi.org/10.1016/j.parkreldis.2020.08.022
Frazzitta G, Bertotti G, Riboldazzi G, Turla M, Uccellini D, Boveri N, Guaglio G, Perini M, Comi C, Balbi P, Maestri R (2012) Effectiveness of intensive inpatient rehabilitation treatment on disease progression in parkinsonian patients: a randomized controlled trial with 1-year follow-up. Neurorehabil Neural Repair 26(2):144–150. https://doi.org/10.1177/1545968311416990
Gao C, Haghayegh S, Wagner M, Cai R, Hu K, Gao L, Li P (2023) Approaches for assessing circadian rest-activity patterns using actigraphy in cohort and population-based studies. Current Sleep Medicine Reports 9(4):247–256. https://doi.org/10.1007/s40675-023-00267-4
García-Nevares A, Fernández-Baizá C, García PF, Méndez M (2020) Performance on daily life activities and executive functioning in Parkinson’s disease. Topics in Geriatric Rehabilitation 36(4):252–259. https://doi.org/10.1097/TGR.0000000000000290
Gavelin HM, Domellof ME, Leung I, Neely AS, Launder NH, Nategh L, Finke C, Lampit A (2022) Computerized cognitive training in Parkinson’s disease: a systematic review and meta-analysis. Ageing Res Rev 80:101671. https://doi.org/10.1016/j.arr.2022.101671
Geng T, Li Y, Peng Y, Chen X, Xu X, Wang J, Sun L, Gao X (2024) Social isolation and the risk of Parkinson disease in the UK biobank study. NPJ Parkinsons Dis 10(1):79. https://doi.org/10.1038/s41531-024-00700-7
Giovannetti T, Britnell P, Brennan L, Siderowf A, Grossman M, Libon DJ, Bettcher BM, Rouzard F, Eppig J, Seidel GA (2012) Everyday action impairment in Parkinson’s disease dementia. J Int Neuropsychol Soc 18(5):787–798. https://doi.org/10.1017/S135561771200046X
Glonnegger H, Beyle A, Cerff B, Graber S, Csoti I, Berg D, Liepelt-Scarfone I (2016) The multiple object test as a performance based tool to assess cognitive driven activity of daily living function in Parkinson’s disease. J Alzheimers Dis 53(4):1475–1484. https://doi.org/10.3233/JAD-160173
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N, Movement Disorder Society URTF (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170. https://doi.org/10.1002/mds.22340
Haahr A, Kirkevold M, Hall EO, Ostergaard K (2011) Living with advanced Parkinson’s disease: a constant struggle with unpredictability. J Adv Nurs 67(2):408–417. https://doi.org/10.1111/j.1365-2648.2010.05459.x
Hayes TL, Abendroth F, Adami A, Pavel M, Zitzelberger TA, Kaye JA (2008) Unobtrusive assessment of activity patterns associated with mild cognitive impairment. Alzheimers Dement 4(6):395–405. https://doi.org/10.1016/j.jalz.2008.07.004
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG (2008) The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord 23(6):837–844. https://doi.org/10.1002/mds.21956
Higginson CI, Lanni K, Sigvardt KA, Disbrow EA (2013) The contribution of trail making to the prediction of performance-based instrumental activities of daily living in Parkinson’s disease without dementia. J Clin Exp Neuropsychol 35(5):530–539. https://doi.org/10.1080/13803395.2013.798397
Hobson P, Meara J (2004) Risk and incidence of dementia in a cohort of older subjects with Parkinson’s disease in the United Kingdom. Movement Disorders Clinical Practice 19(9):1043–1049. https://doi.org/10.1002/mds.20216
Hofmann W, Gschwendner T, Friese M, Wiers RW, Schmitt M (2008) Working memory capacity and self-regulatory behavior: toward an individual differences perspective on behavior determination by automatic versus controlled processes. J Pers Soc Psychol 95(4):962–977. https://doi.org/10.1037/a0012705
Holden SK, Medina LD, Hoyt B, Sillau SH, Berman BD, Goldman JG, Weintraub D, Kluger BM (2018) Validation of a performance-based assessment of cognitive functional ability in Parkinson’s disease. Mov Disord 33(11):1760–1768. https://doi.org/10.1002/mds.27487
Holden SK, Medina LD, Simpson A, Kluger BM (2019) Self-report of cognitive functional abilities is inaccurate in PD-MCI and PDD [abstract]. Behrens, Paper presented at the Movement Disorders Congress
Holden S, Simpson A, Medina L (2020) The UCSD Performance-based Skills assessment primarily measures attention, executive function, and memory in Parkinson’s disease (1081). Neurology 94(15):1081. https://doi.org/10.1212/WNL.94.15_supplement.1081
Holroyd S, Currie LJ, Wooten GF (2005) Depression is associated with impairment of ADL, not motor function in Parkinson disease. Neurology 64(12):2134–2135. https://doi.org/10.1212/01.WNL.0000165958.12724.0D
Holthoff VA, Vieregge P, Kessler J, Pietrzyk U, Herholz K, Bönner J, Wienhard K, Pawlik G, Heiss W-D (1994) Discordant twins with Parkinson’s disease: positron emission tomography and early signs of impaired cognitive circuits. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society 36(2):176–182. https://doi.org/10.1002/ana.410360209
Insel K, Morrow D, Brewer B, Figueredo A (2006) Executive Function. Working Memory, and Medication Adherence among Older Adults. 61(2):102–107. https://doi.org/10.1093/geronb/61.2.P102
Ishimaru D, Tanaka H, Nagata Y, Ogawa Y, Fukuhara K, Takabtake S, Nishikawa T (2021) Impact of disturbed rest-activity rhythms on activities of daily living in moderate and severe dementia patients. Alzheimer Dis Assoc Disord 35(2):135. https://doi.org/10.1097/WAD.0000000000000423
Jonasson SB, Hagell P, Hariz GM, Iwarsson S, Nilsson MH (2017) Psychometric evaluation of the Parkinson’s disease activities of daily living scale. Parkinsons Dis 2017:4151738. https://doi.org/10.1155/2017/4151738
Jutten RJ, Dicks E, Vermaat L, Barkhof F, Scheltens P, Tijms BM, Sikkes SAM (2019) Impairment in complex activities of daily living is related to neurodegeneration in Alzheimer’s disease-specific regions. Neurobiol Aging 75:109–116. https://doi.org/10.1016/j.neurobiolaging.2018.11.018
Kalbe E, Rehberg SP, Heber I, Kronenbuerger M, Schulz JB, Storch A, Linse K, Schneider C, Graber S, Liepelt-Scarfone I, Berg D, Dams J, Balzer-Geldsetzer M, Hilker R, Oberschmidt C, Witt K, Schmidt N, Mollenhauer B, Trenkwalder C, Spottke A, Roeske S, Wittchen HU, Riedel O, Dodel R (2016) Subtypes of mild cognitive impairment in patients with Parkinson’s disease: evidence from the LANDSCAPE study. J Neurol Neurosurg Psychiatry 87(10):1099–1105. https://doi.org/10.1136/jnnp-2016-313838
Kalbe E, Folkerts AK, Ophey A, Eggers C, Elben S, Dimenshteyn K, Sulzer P, Schulte C, Schmidt N, Schlenstedt C, Berg D, Witt K, Wojtecki L, Liepelt-Scarfone I (2020) Enhancement of Executive Functions but Not Memory by Multidomain Group Cognitive Training in Patients with Parkinson’s Disease and Mild Cognitive Impairment: A Multicenter Randomized Controlled Trial. Parkinsons Dis 2020:4068706. https://doi.org/10.1155/2020/4068706
Kawashima S, Matsukawa N, Group RC-NS (2022) Memantine for the patients with mild cognitive impairment in Parkinson’s disease: a pharmacological fMRI study. BMC Neurol 22(1):175. https://doi.org/10.1186/s12883-022-02699-x
Kaye J, Mattek N, Dodge HH, Campbell I, Hayes T, Austin D, Hatt W, Wild K, Jimison H, Pavel M (2014) Unobtrusive measurement of daily computer use to detect mild cognitive impairment. Alzheimers Dement 10(1):10–17. https://doi.org/10.1016/j.jalz.2013.01.011
Kehagia AA, Barker RA, Robbins TW (2010) Neuropsychological and clinical heterogeneity of cognitive impairment and dementia in patients with Parkinson’s disease. Lancet Neurol 9(12):1200–1213. https://doi.org/10.1016/S1474-4422(10)70212-X
Kehagia AA, Barker RA, Robbins TW (2013) Cognitive impairment in Parkinson’s disease: the dual syndrome hypothesis. Neurodegener Dis 11(2):79–92. https://doi.org/10.1159/000341998
King LA, Wilhelm J, Chen Y, Blehm R, Nutt J, Chen Z, Serdar A, Horak FB (2015) Effects of group, individual, and home exercise in persons with parkinson disease: a randomized clinical trial. J Neurol Phys Ther 39(4):204–212. https://doi.org/10.1097/NPT.0000000000000101
Kudlicka A, Clare L, Hindle JV (2013) Awareness of executive deficits in people with Parkinson’s disease. J Int Neuropsychol Soc 19(5):559–570. https://doi.org/10.1017/S1355617713000064
Kulisevsky J, Fernandez de Bobadilla R, Pagonabarraga J, Martinez-Horta S, Campolongo A, Garcia-Sanchez C, Pascual-Sedano B, Ribosa-Nogue R, Villa-Bonomo C (2013) Measuring functional impact of cognitive impairment: validation of the Parkinson’s disease cognitive functional rating scale. Parkinsonism Relat Disord 19(9):812–817. https://doi.org/10.1016/j.parkreldis.2013.05.007
Laatu S, Karrasch M, Martikainen K, Marttila R (2013) Apathy is associated with activities of daily living ability in Parkinson’s disease. Dement Geriatr Cogn Disord 35(5–6):249–255. https://doi.org/10.1159/000347129
Lamont RM, Morris ME, Woollacott MH, Brauer SG (2015) Ambulatory Activity in People with Early Parkinson’s Disease. Brain Impairment 17(1):87–98. https://doi.org/10.1017/BrImp.2015.23
Landers MR, Jacobson KM, Matsunami NE, McCarl HE, Regis MT, Longhurst JK (2021) A vicious cycle of fear of falling avoidance behavior in Parkinson’s disease: a path analysis. Clin Park Relat Disord 4:100089. https://doi.org/10.1016/j.prdoa.2021.100089
Lang AE, Eberly S, Goetz CG, Stebbins G, Oakes D, Marek K, Ravina B, Tanner CM, Shoulson I (2013) Movement disorder society unified Parkinson disease rating scale experiences in daily living: longitudinal changes and correlation with other assessments. Mov Disord 28(14):1980–1986. https://doi.org/10.1002/mds.25671
Lawson RA, Yarnall AJ, Duncan GW, Breen DP, Khoo TK, Williams-Gray CH, Barker RA, Burn DJ, Group I-Ps (2017) Stability of mild cognitive impairment in newly diagnosed Parkinson’s disease. J Neurol Neurosurg Psychiatry 88(8):648–652. https://doi.org/10.1136/jnnp-2016-315099
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Lazzari C, Rabottini M (2022) COVID-19, loneliness, social isolation and risk of dementia in older people: a systematic review and meta-analysis of the relevant literature. Int J Psychiatry Clin Pract 26(2):196–207. https://doi.org/10.1080/13651501.2021.1959616
Lee WJ, Chang YY, Lin JJ, Sung YF, Li JY, Wang SJ, Chen RS, Yang YH, Hu CJ, Tsai CH, Wang HC, Wu SL, Chang MH, Fuh JL (2014) Comparison of activities of daily living impairments in Parkinson’s disease patients as defined by the Pill Questionnaire and assessments by neurologists. J Neurol Neurosurg Psychiatry 85(9):969–973. https://doi.org/10.1136/jnnp-2013-306381
Lee B, Ahn CR, Mohan P, Chaspari T, Lee H-S (2020) Evaluating Routine Variability of Daily Activities in Smart Homes with Image Complexity Measures. J Comput Civ Eng 34(6):282–285. https://doi.org/10.1061/(asce)cp.1943-5487.0000924
Lehrner J, Kogler S, Lamm C, Moser D, Klug S, Pusswald G, Dal-Bianco P, Pirker W, Auff E (2015) Awareness of memory deficits in subjective cognitive decline, mild cognitive impairment, Alzheimer’s disease and Parkinson’s disease. Int Psychogeriatr 27(3):357–366. https://doi.org/10.1017/S1041610214002245
Leonard A (2016) The relationship between circadian dysfunction and cognitive impairment in individuals with Parkinson’s disease. Undergraduate Review 12(15):80–89
Leroi I, McDonald K, Pantula H, Harbishettar V (2012) Cognitive impairment in Parkinson disease: impact on quality of life, disability, and caregiver burden. J Geriatr Psychiatry Neurol 25(4):208–214. https://doi.org/10.1177/0891988712464823
Leung IH, Walton CC, Hallock H, Lewis SJ, Valenzuela M, Lampit A (2015) Cognitive training in Parkinson disease: A systematic review and meta-analysis. Neurology 85(21):1843–1851. https://doi.org/10.1212/WNL.0000000000002145
Liebermann-Jordanidis H, Roheger M, Boosfeld L, Franklin J, Kalbe E (2022) Which test is the best to assess visuo-cognitive impairment in patients with Parkinson’s disease with mild cognitive impairment and dementia? a systematic review and meta-analysis. J Parkinsons Dis 12(6):1749–1782. https://doi.org/10.3233/JPD-223238
Liepelt-Scarfone I, Fruhmann Berger M, Prakash D, Csoti I, Graber S, Maetzler W, Berg D (2013) Clinical characteristics with an impact on ADL functions of PD patients with cognitive impairment indicative of dementia. PLoS ONE 8(12):e82902. https://doi.org/10.1371/journal.pone.0082902
Liepelt-Scarfone I, Ophey A, Kalbe E (2022) Cognition in prodromal Parkinson’s disease. Prog Brain Res 269(1):93–111. https://doi.org/10.1016/bs.pbr.2022.01.003
Lina C, Guoen C, Huidan W, Yingqing W, Ying C, Xiaochun C, Qinyong Y (2020) The effect of virtual reality on the ability to perform activities of daily living, balance during gait, and motor function in parkinson disease patients: a systematic review and meta-analysis. Am J Phys Med Rehabil 99(10):917–924. https://doi.org/10.1097/PHM.0000000000001447
Litvan I, Aarsland D, Adler CH, Goldman JG, Kulisevsky J, Mollenhauer B, Rodriguez-Oroz MC, Troster AI, Weintraub D (2011) MDS Task Force on mild cognitive impairment in Parkinson’s disease: critical review of PD-MCI. Mov Disord 26(10):1814–1824. https://doi.org/10.1002/mds.23823
Litvan I, Goldman JG, Troster AI, Schmand BA, Weintraub D, Petersen RC, Mollenhauer B, Adler CH, Marder K, Williams-Gray CH, Aarsland D, Kulisevsky J, Rodriguez-Oroz MC, Burn DJ, Barker RA, Emre M (2012) Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Mov Disord 27(3):349–356. https://doi.org/10.1002/mds.24893
Lopez FV, Ferencz B, Rohl BY, Trifilio E, Scott B, Okun MS, Marsiske M, Bowers D (2019) Everyday functioning in Parkinson’s disease: evidence from the revised-observed tasks of daily living (OTDL-R). Parkinsonism Relat Disord 60:167–170. https://doi.org/10.1016/j.parkreldis.2018.08.026
Loprinzi PD, Danzl MM, Ulanowski E, Paydo C (2018) A pilot study evaluating the association between physical activity and cognition among individuals with Parkinson’s disease. Disabil Health J 11(1):165–168. https://doi.org/10.1016/j.dhjo.2017.05.004
Mahieux F, Fenelon G, Flahault A, Manifacier MJ, Michelet D, Boller F (1998) Neuropsychological prediction of dementia in Parkinson’s disease. J Neurol Neurosurg Psychiatry 64(2):178–183
Mamikonyan E, Xie SX, Melvin E, Weintraub D (2015) Rivastigmine for mild cognitive impairment in Parkinson disease: a placebo-controlled study. Mov Disord 30(7):912–918. https://doi.org/10.1002/mds.26236
Manning KJ, Clarke C, Lorry A, Weintraub D, Wilkinson JR, Duda JE, Moberg PJ (2012) Medication management and neuropsychological performance in Parkinson’s disease. Clin Neuropsychol 26(1):45–58. https://doi.org/10.1080/13854046.2011.639312
Marson DC, Sawrie SM, Snyder S, McInturff B, Stalvey T, Boothe A, Aldridge T, Chatterjee A, Harrell LE (2000) Assessing financial capacity in patients with Alzheimer disease: a conceptual model and prototype instrument. Arch Neurol 57(6):877–884. https://doi.org/10.1001/archneur.57.6.877
Martin RC, Triebel KL, Kennedy RE, Nicholas AP, Watts RL, Stover NP, Brandon M, Marson DC (2013) Impaired financial abilities in Parkinson’s disease patients with mild cognitive impairment and dementia. Parkinsonism Relat Disord 19(11):986–990. https://doi.org/10.1016/j.parkreldis.2013.06.017
Martinez-Martin P (2013) Dementia in Parkinson’s disease: usefulness of the pill questionnaire. Mov Disord 28(13):1832–1837. https://doi.org/10.1002/mds.25649
Mathie MJ, Coster AC, Lovell NH, Celler BG (2004) Accelerometry: providing an integrated, practical method for long-term, ambulatory monitoring of human movement. Physiol Meas 25(2):R1-20. https://doi.org/10.1088/0967-3334/25/2/r01
Matsunaga S, Kishi T, Yasue I, Iwata N (2015) Cholinesterase Inhibitors for Lewy Body Disorders: A Meta-Analysis. Int J Neuropsychopharmacol 19(2):086. https://doi.org/10.1093/ijnp/pyv086
Matthews CE, Moore SC, George SM, Sampson J, Bowles HR (2012) Improving self-reports of active and sedentary behaviors in large epidemiologic studies. Exerc Sport Sci Rev 40(3):118–126. https://doi.org/10.1097/JES.0b013e31825b34a0
Mc Ardle R, Del Din S, Donaghy P, Galna B, Thomas A, Rochester L (2020) Factors that influence habitual activity in mild cognitive impairment and dementia. Gerontology 66(2):197–208. https://doi.org/10.1159/000502288
Mc Ardle R, Jabbar KA, Del Din S, Thomas AJ, Robinson L, Kerse N, Rochester L, Callisaya M (2023) Using digital technology to quantify habitual physical activity in community dwellers with cognitive impairment: systematic review. J Med Internet Res 25:e44352. https://doi.org/10.2196/44352
McRae C, Diem G, Vo A, O’Brien C, Seeberger L (2000) Schwab & England: standardization of administration. Movement Disorders: Official Journal of the Movement Disorder Society 15(2):335–336. https://doi.org/10.1002/1531-8257(200003)15:2%3c335::AID-MDS1022%3e3.0.CO;2-V
McShane R, Westby MJ, Roberts E, Minakaran N, Schneider L, Farrimond LE, Maayan N, Ware J, Debarros J (2019) Memantine for dementia. Cochrane Database Syst Rev 3(3):CD003154. https://doi.org/10.1002/14651858.CD003154.pub6
Miller EK, Wallis JD (2009) Executive function and higher-order cognition: definition and neural substrates. In: LR S (ed) Encyclopedia of neuroscience, vol 4. Academic Press:Oxford 99 104
Monticone M, Ambrosini E, Laurini A, Rocca B, Foti C (2015) In-patient multidisciplinary rehabilitation for Parkinson’s disease: A randomized controlled trial. Mov Disord 30(8):1050–1058. https://doi.org/10.1002/mds.26256
Morgan C, Jameson J, Craddock I, Tonkin EL, Oikonomou G, Isotalus HK, Heidarivincheh F, McConville R, Tourte GJL, Kinnunen KM, Whone A (2022) Understanding how people with Parkinson’s disease turn in gait from a real-world in-home dataset. Parkinsonism Relat Disord 105:114–122. https://doi.org/10.1016/j.parkreldis.2022.11.007
Morris ME, Menz HB, McGinley JL, Watts JJ, Huxham FE, Murphy AT, Danoudis ME, Iansek R (2015) A Randomized Controlled Trial to Reduce Falls in People With Parkinson’s Disease. Neurorehabil Neural Repair 29(8):777–785. https://doi.org/10.1177/1545968314565511
Muslimovic D, Post B, Speelman JD, Schmand B (2005) Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology 65(8):1239–1245. https://doi.org/10.1212/01.wnl.0000180516.69442.95
Novakova L, Gajdos M, Markova J, Martinkovicova A, Kosutzka Z, Svantnerova J, Valkovic P, Csefalvay Z, Rektorova I (2023) Language impairment in Parkinson’s disease: fMRI study of sentence reading comprehension. Front Aging Neurosci 15:1117473. https://doi.org/10.3389/fnagi.2023.1117473
Numbers K, Jang S, Brodaty H, Sachdev PS, Draper B, Reppermund S (2022) Instrumental activities of daily living by subjective and objective measures: the impact of depression and personality. Front Aging Neurosci 14:829544. https://doi.org/10.3389/fnagi.2022.829544
Pagano G, Rengo G, Pasqualetti G, Femminella GD, Monzani F, Ferrara N, Tagliati M (2015) Cholinesterase inhibitors for Parkinson’s disease: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 86(7):767–773. https://doi.org/10.1136/jnnp-2014-308764
Palamara G, Gotti F, Maestri R, Bera R, Gargantini R, Bossio F, Zivi I, Volpe D, Ferrazzoli D, Frazzitta G (2017) Land plus aquatic therapy versus land-based rehabilitation alone for the treatment of balance dysfunction in Parkinson disease: a randomized controlled study with 6-month follow-up. Arch Phys Med Rehabil 98(6):1077–1085. https://doi.org/10.1016/j.apmr.2017.01.025
Paolucci T, Zangrando F, Piccinini G, Deidda L, Basile R, Bruno E, Buzi E, Mannocci A, Tirinelli F, Haggiag S, Lispi L, Villani C, Saraceni VM (2017) Impact of mezieres rehabilitative method in patients with Parkinson’s disease: a randomized controlled trial. Parkinsons Dis 2017:2762987. https://doi.org/10.1155/2017/2762987
Paradis E, Sutkin G (2017) Beyond a good story: from Hawthorne Effect to reactivity in health professions education research. Med Educ 51(1):31–39. https://doi.org/10.1111/medu.13122
París AP, Saleta HG, de la Maraver MCC, Silvestre E, Freixa MG, Torrellas CP, Pont SA, Nadal MF, Garcia SA, Bartolomé MV, Fernández VL, Bayés AR (2011) Blind randomized controlled study of the efficacy of cognitive training in Parkinson’s disease. Mov Disord 26(7):1251–1258. https://doi.org/10.1002/mds.23688
Park J-H (2022) Does the virtual shopping training improve executive function and instrumental activities of daily living of patients with mild cognitive impairment? Asian J Psychiatr 69:102977. https://doi.org/10.1016/j.ajp.2021.102977
Parsons C, Lim WY, Loy C, McGuinness B, Passmore P, Ward SA, Hughes C (2021) Withdrawal or continuation of cholinesterase inhibitors or memantine or both, in people with dementia. Cochrane Database Syst Rev 2(2):CD009081. https://doi.org/10.1002/14651858.CD009081.pub2
Patterson TL, Lacro J, McKibbin CL, Moscona S, Hughs T, Jeste DV (2002) Medication management ability assessment: results from a performance-based measure in older outpatients with schizophrenia. J Clin Psychopharmacol 22(1):11–19
Pedreira G, Prazeres A, Cruz D, Gomes I, Monteiro L, Melo A (2013) Virtual games and quality of life in Parkinson’s disease: a randomised controlled trial. Advances in Parkinson’s Disease 02(04):97–101. https://doi.org/10.4236/apd.2013.24018
Peña J, Ibarretxe-Bilbao N, García-Gorostiaga I, Gomez-Beldarrain MA, Díez-Cirarda M, Ojeda N (2014) Improving functional disability and cognition in Parkinson disease: randomized controlled trial. Neurology 83(23):2167–2174. https://doi.org/10.1212/WNL.0000000000001043
Pennington C, Duncan G, Ritchie C (2021) Altered awareness of cognitive and neuropsychiatric symptoms in Parkinson’s disease and Dementia with Lewy Bodies: a systematic review. Int J Geriatr Psychiatry 36(1):15–30. https://doi.org/10.1002/gps.5415
Perry SIB, Nelissen PM, Siemonsma P, Lucas C (2019) The effect of functional-task training on activities of daily living for people with Parkinson;s disease, a systematic review with meta-analysis. Complement Ther Med 42:312–321. https://doi.org/10.1016/j.ctim.2018.12.008
Pfeffer RI, Kurosaki TT, Harrah CH Jr, Chance JM, Filos S (1982) Measurement of functional activities in older adults in the community. J Gerontol 37(3):323–329
Pirogovsky E, Woods SP, Vincent Filoteo J, Gilbert PE (2012) Prospective memory deficits are associated with poorer everyday functioning in Parkinson’s disease. J Int Neuropsychol Soc 18(6):986–995. https://doi.org/10.1017/S1355617712000781
Pirogovsky E, Martinez-Hannon M, Schiehser DM, Lessig SL, Song DD, Litvan I, Filoteo JV (2013) Predictors of performance-based measures of instrumental activities of daily living in nondemented patients with Parkinson’s disease. J Clin Exp Neuropsychol 35(9):926–933. https://doi.org/10.1080/13803395.2013.838940
Pirogovsky E, Schiehser DM, Obtera KM, Burke MM, Lessig SL, Song DD, Litvan I, Filoteo JV (2014) Instrumental activities of daily living are impaired in Parkinson’s disease patients with mild cognitive impairment. Neuropsychology 28(2):229–237. https://doi.org/10.1037/neu0000045
Pompeu JE, Mendes FA, Silva KG, Lobo AM, Oliveira Tde P, Zomignani AP, Piemonte ME (2012) Effect of Nintendo Wii-based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: a randomised clinical trial. Physiotherapy 98(3):196–204. https://doi.org/10.1016/j.physio.2012.06.004
Puente AN, Cohen ML, Aita S, Brandt J (2016) Behavioral ratings of executive functioning explain instrumental activities of daily living beyond test scores in Parkinson’s disease. Clin Neuropsychol 30(1):95–106. https://doi.org/10.1080/13854046.2015.1133847
Rabinowitz JA, An Y, He L, Alfini AJ, Zipunnikov V, Wu MN, Wanigatunga SK, Schrack JA, Jackson CL, Ferrucci L, Simonsick EM, Resnick SM, Spira AP (2022) Associations of circadian rest/activity rhythms with cognition in middle-aged and older adults: Demographic and genetic interactions. Front Neurosci 16:952204. https://doi.org/10.3389/fnins.2022.952204
Raffegeau TE, Krehbiel LM, Kang N, Thijs FJ, Altmann LJP, Cauraugh JH, Hass CJ (2019) A meta-analysis: Parkinson’s disease and dual-task walking. Parkinsonism Relat Disord 62:28–35. https://doi.org/10.1016/j.parkreldis.2018.12.012
Ranchet M, Broussolle E, Poisson A, Paire-Ficout L (2012) Relationships between cognitive functions and driving behavior in Parkinson’s disease. Eur Neurol 68(2):98–107. https://doi.org/10.1159/000338264
Ransmayr G (2020) Caregiver burden in patients with Parkinson’s disease. Fortschr Neurol Psychiatr 88(9):567–572. https://doi.org/10.1055/a-1120-8567
Rawtaer I, Mahendran R, Kua EH, Tan HP, Tan HX, Lee TS, Ng TP (2020) Early detection of mild cognitive impairment with in-home sensors to monitor behavior patterns in community-dwelling senior citizens in Singapore: cross-sectional feasibility study. J Med Internet Res 22(5):e16854. https://doi.org/10.2196/16854
Reginold W, Armstrong MJ, Duff-Canning S, Lang A, Tang-Wai D, Fox S, Rothberg B, Zadikoff C, Kennedy N, Gill D, Eslinger P, Mapstone M, Chou K, Persad C, Litvan I, Mast B, Marras C (2012) The pill questionnaire in a nondemented Parkinson’s disease population. Mov Disord 27(10):1308–1311. https://doi.org/10.1002/mds.25124
Rehman RZU, Guan Y, Shi JQ, Alcock L, Yarnall AJ, Rochester L, Del Din S (2022) Investigating the Impact of Environment and Data Aggregation by Walking Bout Duration on Parkinson’s Disease Classification Using Machine Learning. Front Aging Neurosci 14:808518. https://doi.org/10.3389/fnagi.2022.808518
Ribas CG, Alves da Silva L, Correa MR, Teive HG, Valderramas S (2017) Effectiveness of exergaming in improving functional balance, fatigue and quality of life in Parkinson’s disease: A pilot randomized controlled trial. Parkinsonism Relat Disord 38:13–18. https://doi.org/10.1016/j.parkreldis.2017.02.006
Rider JV, Longhurst JK, Navalta JW, Young DL, Landers MR (2023) Fear of falling avoidance behavior in Parkinson’s disease: most frequently avoided activities. OTJR (thorofare N j) 43(2):228–236. https://doi.org/10.1177/15394492221106103
Riedel O, Klotsche J, Spottke A, Deuschl G, Forstl H, Henn F, Heuser I, Oertel W, Reichmann H, Riederer P, Trenkwalder C, Dodel R, Wittchen HU (2010) Frequency of dementia, depression, and other neuropsychiatric symptoms in 1,449 outpatients with Parkinson’s disease. J Neurol 257(7):1073–1082. https://doi.org/10.1007/s00415-010-5465-z
Rolinski M, Fox C, Maidment I (2012) McShane R (2012) Cholinesterase inhibitors for dementia with Lewy bodies, Parkinson’s disease dementia and cognitive impairment in Parkinson’s disease. Cochrane Database Syst Rev 3:CD006504. https://doi.org/10.1002/14651858.CD006504.pub2
Roll EE, Giovannetti T, Libon DJ, Eppig J (2019) Everyday task knowledge and everyday function in dementia. J Neuropsychol 13(1):96–120. https://doi.org/10.1111/jnp.12135
Rosenblum S, Meyer S, Richardson A, Hassin-Baer S (2022) Early identification of subjective cognitive functional decline among patients with Parkinson’s disease: a longitudinal pilot study. Sci Rep 12(1):22242. https://doi.org/10.1038/s41598-022-26280-1
Rosenthal E, Brennan L, Xie S, Hurtig H, Milber J, Weintraub D, Karlawish J, Siderowf A (2010) Association between cognition and function in patients with Parkinson disease with and without dementia. Movement Disorders: Official Journal of the Movement Disorder Society 25(9):1170–1176. https://doi.org/10.1002/mds.23073
Ruzafa-Valiente E, Fernandez-Bobadilla R, Garcia-Sanchez C, Pagonabarraga J, Martinez-Horta S, Kulisevsky J (2016) Parkinson’s disease-cognitive functional rating scale across different conditions and degrees of cognitive impairment. J Neurol Sci 361:66–71. https://doi.org/10.1016/j.jns.2015.12.018
Santangelo G, Vitale C, Picillo M, Moccia M, Cuoco S, Longo K, Pezzella D, di Grazia A, Erro R, Pellecchia MT (2015) Mild cognitive impairment in newly diagnosed parkinson’s disease: a longitudinal prospective study. Parkinsonism Relat Disord 21(10):1219–1226. https://doi.org/10.1016/j.parkreldis.2015.08.024
Sardinha LB, Ekelund U, dos Santos L, Cyrino ES, Silva AM, Santos DA (2015) Breaking-up sedentary time is associated with impairment in activities of daily living. Exp Gerontol 72:57–62. https://doi.org/10.1016/j.exger.2015.09.011
Saredakis D, Collins-Praino LE, Gutteridge DS, Stephan BCM, Keage HAD (2019) Conversion to MCI and dementia in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord 65:20–31. https://doi.org/10.1016/j.parkreldis.2019.04.020
Sawada H, Oeda T, Kohsaka M, Umemura A, Tomita S, Park K, Mizoguchi K, Matsuo H, Hasegawa K, Fujimura H, Sugiyama H, Nakamura M, Kikuchi S, Yamamoto K, Fukuda T, Ito S, Goto M, Kiyohara K, Kawamura T (2018) Early use of donepezil against psychosis and cognitive decline in Parkinson’s disease: a randomised controlled trial for 2 years. J Neurol Neurosurg Psychiatry 89(12):1332–1340. https://doi.org/10.1136/jnnp-2018-318107
Sawada H, Oeda T, Kohsaka M, Tomita S, Umemura A, Park K, Yamamoto K, Kiyohara K (2021) Early-start vs delayed-start donepezil against cognitive decline in Parkinson disease: a randomized clinical trial. Expert Opin Pharmacother 22(3):363–371. https://doi.org/10.1080/14656566.2020.1814255
Schenkman M, Hall DA, Barón AE, Schwartz RS, Mettler P, Kohrt WM (2012) Exercise for people in early-or mid-stage Parkinson disease: a 16-month randomized controlled trial. Phys Ther 92(11):1395–1410. https://doi.org/10.2522/ptj.20110472
Schmitter-Edgecombe M, Dyck DG (2014) Cognitive rehabilitation multi-family group intervention for individuals with mild cognitive impairment and their care-partners. J Int Neuropsychol Soc 20(9):897–908. https://doi.org/10.1017/S1355617714000782
Schmitter-Edgecombe M, Parsey C, Cook DJ (2011) Cognitive correlates of functional performance in older adults: comparison of self-report, direct observation, and performance-based measures. J Int Neuropsychol Soc 17(5):853–864. https://doi.org/10.1017/S1355617711000865
Schmitter-Edgecombe M, McAlister C, Greeley D (2022) A comparison of functional abilities in individuals with mild cognitive impairment and Parkinson’s disease with mild cognitive impairment using multiple assessment methods. J Int Neuropsychol Soc 28(8):798–809. https://doi.org/10.1017/S1355617721001077
Schmitter-Edgecombe M, Brown K, Chilton RC, Whiteley N, Greeley D (2024) Naturalistic assessment of everyday multitasking in Parkinson’s disease with and without mild cognitive impairment. Clin Neuropsychol 12:1–21. https://doi.org/10.1080/13854046.2024.2325681
Schrag A, Horsfall L, Walters K, Noyce A, Petersen I (2015) Prediagnostic presentations of Parkinson’s disease in primary care: a case-control study. Lancet Neurol 14(1):57–64. https://doi.org/10.1016/S1474-4422(14)70287-X
Schütz N, Saner H, Rudin B, Botros A, Pais B, Santschi V, Buluschek P, Gatica-Perez D, Urwyler P, Marchal-Crespo L, Muri RM, Nef T (2019) Validity of pervasive computing based continuous physical activity assessment in community-dwelling old and oldest-old. Sci Rep 9(1):9662. https://doi.org/10.1038/s41598-019-45733-8
Schwab R, England A (1968) Projection technique for evaluating surgery in Parkinson’s disease. In: Gillingham FJ, Donaldson IML (eds) Third Symposium on Parkinson’s Disease. Livingstone Ltd, Edinburgh, Scotland
Shen C, Rolls E, Cheng W, Kang J, Dong G, Xie C, Zhao XM, Sahakian B, Feng J (2022) Associations of social isolation and loneliness with later Dementia. Neurology. https://doi.org/10.1212/WNL.0000000000200583
Shulman LM, Pretzer-Aboff I, Anderson KE, Stevenson R, Vaughan CG, Gruber-Baldini AL, Reich SG, Weiner WJ (2006) Subjective report versus objective measurement of activities of daily living in Parkinson’s disease. Mov Disord 21(6):794–799. https://doi.org/10.1002/mds.20803
Shulman LM, Armstrong M, Ellis T, Gruber-Baldini A, Horak F, Nieuwboer A, Parashos S, Post B, Rogers M, Siderowf A, Goetz CG, Schrag A, Stebbins GT, Martinez-Martin P (2016) Disability Rating Scales in Parkinson’s Disease: Critique and Recommendations. Mov Disord 31(10):1455–1465. https://doi.org/10.1002/mds.26649
Siciliano M, Trojano L, De Micco R, Sant’Elia V, Giordano A, Russo A, Passamonti L, Tedeschi G, Chiorri C, Tessitore A (2021) Correlates of the discrepancy between objective and subjective cognitive functioning in non-demented patients with Parkinson’s disease. J Neurol 268(9):3444–3455. https://doi.org/10.1007/s00415-021-10519-4
Skinner JW, Lee HK, Roemmich RT, Amano S, Hass CJ (2015) Execution of activities of daily living in persons with Parkinson disease. Med Sci Sports Exerc 47(9):1906–1912. https://doi.org/10.1249/mss.0000000000000598
Small JA, Lyons K, Kemper S (1997) Grammatical abilities in Parkinson’s disease: evidence from written sentences. Neuropsychologia 35(12):1571–1576. https://doi.org/10.1016/S0028-3932(97)00089-4
Son JY, Zhou W, Webster-Dekker KE, Marriott DJ, Larson JL (2024) Association between accelerometry measured patterns of sedentary behaviors and functional status in older adults. Aging Clin Exp Res 36(1):11. https://doi.org/10.1007/s40520-023-02644-z
Sousa NMF, Neri A, Brandi IV, Brucki SMD (2021) Impact of cognitive intervention on cognitive symptoms and quality of life in idiopathic Parkinson’s disease: a randomized and controlled study. Dement Neuropsychol 15(1):51–59. https://doi.org/10.1590/1980-57642021dn15-010005
Sperens M, Georgiev D, Eriksson Domellof M, Forsgren L, Hamberg K, Hariz GM (2020) Activities of daily living in Parkinson’s disease: Time/gender perspective. Acta Neurol Scand 141(2):168–176. https://doi.org/10.1111/ane.13189
Staunton H, Kelly K, Newton L, Leddin M, Rodriguez-Esteban R, Chaudhuri KR, Weintraub D, Postuma RB, Martinez-Martin P (2022) A patient-centered conceptual model of symptoms and their impact in early Parkinson’s disease: a qualitative study. J Parkinsons Dis 12(1):137–151. https://doi.org/10.3233/JPD-202457
Suchy Y, Ziemnik RE, Niermeyer MA, Brothers SL (2020) Executive functioning interacts with complexity of daily life in predicting daily medication management among older adults. Clin Neuropsychol 34(4):797–825. https://doi.org/10.1080/13854046.2019.1694702
Sulzer P, Baumer A, Hoang HG, Becker S, Lonneker HD, Graessel E, Liepelt-Scarfone I (2020) Assessment of cognitive-driven performance-based activities of daily living dysfunction in Parkinson’s disease. J Int Neuropsychol Soc 26(4):430–440. https://doi.org/10.1017/S1355617719001322
Sumida CA, Lopez FV, Van Etten EJ, Whiteley N, Moore RC, Litvan I, Lessig S, Gilbert PE, Schmitter-Edgecombe M, Filoteo JV, Schiehser DM (2021) Medication management performance in Parkinson’s disease: examination of process errors. Arch Clin Neuropsychol 36(7):1307–1315. https://doi.org/10.1093/arclin/acab004
Tafiadis D, Siafaka V, Voniati L, Prentza A, Papadopoulos A, Ziavra N, Konitsiotis S (2023) Lawton’s instrumental activities of daily living for greek-speaking adults with cognitive impairment: a psychometric evaluation study with additional receiver operating characteristic curve analysis. Brain Sci 13(7):1093. https://doi.org/10.3390/brainsci13071093
Tamir R, Dickstein R, Huberman M (2007) Integration of motor imagery and physical practice in group treatment applied to subjects with Parkinson’s disease. Neurorehabil Neural Repair 21(1):68–75. https://doi.org/10.1177/1545968306292608
Terashi H, Mitoma H, Yoneyama M, Aizawa H (2017) Relationship between Amount of daily movement measured by a triaxial accelerometer and motor symptoms in patients with Parkinson’s disease. Appl Sci 7(5):486. https://doi.org/10.3390/app7050486
Thaler A, Mirelman A, Gurevich T, Simon E, Orr-Urtreger A, Marder K, Bressman S, Giladi N, Consortium ObotLAJ (2012) Lower cognitive performance in healthy G2019S LRRK2 mutation carriers. Neurology 79(10):1027–1032. https://doi.org/10.1212/WNL.0b013e3182684646
Thordardottir B, Nilsson MH, Iwarsson S, Haak M (2014) “You plan, but you never know”–participation among people with different levels of severity of Parkinson’s disease. Disabil Rehabil 36(26):2216–2224. https://doi.org/10.3109/09638288.2014.898807
Tieges Z, Mead G, Allerhand M, Duncan F, van Wijck F, Fitzsimons C, Greig C, Chastin S (2015) Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil 96(1):15–23. https://doi.org/10.1016/j.apmr.2014.08.015
Tulliani N, Bissett M, Fahey P, Bye R, Liu KPY (2022) Efficacy of cognitive remediation on activities of daily living in individuals with mild cognitive impairment or early-stage dementia: a systematic review and meta-analysis. Syst Rev 11(1):156. https://doi.org/10.1186/s13643-022-02032-0
Urwyler P, Stucki R, Rampa L, Muri R, Mosimann UP, Nef T (2017) Cognitive impairment categorized in community-dwelling older adults with and without dementia using in-home sensors that recognise activities of daily living. Sci Rep 7:42084. https://doi.org/10.1038/srep42084
van Uem JMT, Cerff B, Kampmeyer M, Prinzen J, Zuidema M, Hobert MA, Graber S, Berg D, Maetzler W, Liepelt-Scarfone I (2018) The association between objectively measured physical activity, depression, cognition, and health-related quality of life in Parkinson’s disease. Parkinsonism Relat Disord 48:74–81. https://doi.org/10.1016/j.parkreldis.2017.12.023
Vann-Ward T, Morse JM, Charmaz K (2017) Preserving self: theorizing the social and psychological processes of living with Parkinson disease. Qual Health Res 27(7):964–982. https://doi.org/10.1177/1049732317707494
Vlagsma TT, Koerts J, Tucha O, Dijkstra HT, Duits AA, van Laar T, Spikman JM (2017) Objective versus subjective measures of executive functions: predictors of participation and quality of life in Parkinson disease? Arch Phys Med Rehabil 98(11):2181–2187. https://doi.org/10.1016/j.apmr.2017.03.016
Volpe D, Giantin MG, Maestri R, Frazzitta G (2014) Comparing the effects of hydrotherapy and land-based therapy on balance in patients with Parkinson’s disease: a randomized controlled pilot study. Clin Rehabil 28(12):1210–1217. https://doi.org/10.1177/0269215514536060
Warden C, Hwang J, Marshall A, Fenesy M, Poston KL (2016) The effects of dopamine on digit span in Parkinson’s disease. J Clin Mov Disord 3:5. https://doi.org/10.1186/s40734-016-0033-z
Warmerdam E, Hausdorff JM, Atrsaei A, Zhou Y, Mirelman A, Aminian K, Espay AJ, Hansen C, Evers LJW, Keller A, Lamoth C, Pilotto A, Rochester L, Schmidt G, Bloem BR, Maetzler W (2020) Long-term unsupervised mobility assessment in movement disorders. Lancet Neurol 19(5):462–470. https://doi.org/10.1016/S1474-4422(19)30397-7
Weakley A, Weakley AT, Schmitter-Edgecombe M (2019) Compensatory strategy use improves real-world functional performance in community dwelling older adults. Neuropsychology 33(8):1121–1135. https://doi.org/10.1037/neu0000591
Weintraub D, Marras C, Amara A, Anderson KE, Chahine LM, Eberly S, Hosamath A, Kinel D, Mantri S, Mathur S, Oakes D, Purks JL, Standaert DG, Shoulson I, Arbatti L (2024) Association between subjective cognitive complaints and incident functional impairment in Parkinson’s disease. Mov Disord. https://doi.org/10.1002/mds.29725
Wettstein M, Wahl HW, Shoval N, Oswald F, Voss E, Seidl U, Frolich L, Auslander G, Heinik J, Landau R (2015) Out-of-home behavior and cognitive impairment in older adults: findings of the SenTra Project. J Appl Gerontol 34(1):3–25. https://doi.org/10.1177/0733464812459373
Williams-Gray CH, Evans JR, Goris A, Foltynie T, Ban M, Robbins TW, Brayne C, Kolachana BS, Weinberger DR, Sawcer SJ, Barker RA (2009) The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain 132(Pt 11):2958–2969. https://doi.org/10.1093/brain/awp245
Wu JQ, Li P, Stavitsky Gilbert K, Hu K, Cronin-Golomb A (2018) Circadian rest-activity rhythms predict cognitive function in early Parkinson’s disease independently of sleep. Mov Disord Clin Pract 5(6):614–619. https://doi.org/10.1002/mdc3.12692
Yamasaki T, Kumagai S (2021) Nonwearable Sensor-Based In-Home Assessment of Subtle Daily Behavioral Changes as a Candidate Biomarker for Mild Cognitive Impairment. J Pers Med 12(1):11. https://doi.org/10.3390/jpm12010011
Yilmaz R, Behnke S, Liepelt-Scarfone I, Roeben B, Pausch C, Runkel A, Heinzel S, Niebler R, Suenkel U, Eschweiler GW, Maetzler W, Berg D (2016) Substantia nigra hyperechogenicity is related to decline in verbal memory in healthy elderly adults. Eur J Neurol 23(5):973–978. https://doi.org/10.1111/ene.12974
Yoo K, Chung SJ, Kim HS, Choung O-h, Lee Y-B, Kim M-J, You S, Jeong Y (2015) Neural substrates of motor and non-motor symptoms in Parkinson’s disease: a resting fMRI study. PLoS ONE 10(4):e0125455. https://doi.org/10.1371/journal.pone.0125455
Zaman A, Ellingson L, Sunken A, Gibson E, Stegemoller EL (2021) Determinants of exercise behaviour in persons with Parkinson’s disease. Disabil Rehabil 43(5):696–702. https://doi.org/10.1080/09638288.2019.1638975
Zhu Z, Yin M, Cui L, Zhang Y, Hou W, Li Y, Zhao H (2018) Aquatic obstacle training improves freezing of gait in Parkinson’s disease patients: a randomized controlled trial. Clin Rehabil 32(1):29–36. https://doi.org/10.1177/0269215517715763
Zolfaghari S, Thomann AE, Lewandowski N, Trundell D, Lipsmeier F, Pagano G, Taylor KI, Postuma RB (2022) Self-Report versus Clinician Examination in Early Parkinson’s Disease. Mov Disord 37(3):585–597. https://doi.org/10.1002/mds.28884
Zokaei N, McNeill A, Proukakis C, Beavan M, Jarman P, Korlipara P, Hughes D, Mehta A, Hu MT, Schapira AH, Husain M (2014) Visual short-term memory deficits associated with GBA mutation and Parkinson's disease. Brain 137 (Pt 8):2303–2311. https://doi.org/10.1093/brain/awu143
Acknowledgements
We thank Daniela Renftle for her critical revision of the Tables and the Supplementary Material.
Funding
Open Access funding enabled and organized by Projekt DEAL. German Ministry of Education and Research, General Joint Committee, Deutsche Gesellschaft für Parkinson und Bewegungsstörungen, STADAPHARM GmbH, AbbVie GmbH Germany, Bayer, Desitin Arzneimittel, Deutsche Gesellschaft für Neurologie
Author information
Authors and Affiliations
Contributions
M. Bode, E. Kalbe, and I. Liepelt-Scarfone created the concept for the article. M. Bode and I. Liepelt-Scarfone drafted the manuscript. E. Kalbe revised the manuscript. M. Bode, E Kalbe, and I. Liepelt-Scarfone performed literature research.
Corresponding author
Ethics declarations
Financial interests
M. Bode reports no financial interests. E. Kalbe has received grants from the German Ministry of Education and Research, General Joint Committee, Germany, the German Parkinson Society, and STADAPHARM GmbH; honoraria from AbbVie GmbH Germany; memodio GmbH Germany; license fees from Prolog GmbH, Germany.
I. Liepelt-Scarfone reports funding from Bayer AG and travel grants from Desitin and the Deutsche Gesellschaft für Neurologie outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bode, M., Kalbe, E. & Liepelt-Scarfone, I. Cognition and Activity of Daily Living Function in people with Parkinson’s disease. J Neural Transm (2024). https://doi.org/10.1007/s00702-024-02796-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00702-024-02796-w