Abstract
Both cerebrospinal fluid (CSF) homovanillic acid (HVA) and striatal dopamine transporter (DAT) binding on single-photon emission computed tomography (SPECT) reflect nigrostriatal dopaminergic function, but studies on the relationship between the two have been limited. It is also unknown whether the reported variance in striatal DAT binding among diseases reflects the pathophysiology or characteristics of the subjects. We included 70 patients with Parkinson’s disease (PD), 12 with progressive supranuclear palsy (PSP), 12 with multiple system atrophy, six with corticobasal syndrome, and nine with Alzheimer’s disease as disease control, who underwent both CSF analysis and 123I-N-ω-fluoropropyl-2β-carbomethoxy-3β-(4-iodophenyl)nortropane (123I-ioflupane) SPECT. We evaluated the correlation between CSF HVA concentration and the specific binding ratio (SBR) of striatal DAT binding. We also compared the SBR for each diagnosis, controlling for CSF HVA concentration. The correlations between the two were significant in patients with PD (r = 0.34, p = 0.004) and PSP (r = 0.77, p = 0.004). The mean SBR value was the lowest in patients with PSP and was significantly lower in patients with PSP than in those with PD (p = 0.037) after adjusting for CSF HVA concentration. Our study demonstrates that striatal DAT binding correlates with CSF HVA concentration in both PD and PSP, and striatal DAT reduction would be more advanced in PSP than in PD at an equivalent dopamine level. Striatal DAT binding may correlate with dopamine levels in the brain. The pathophysiology of each diagnosis may explain this difference.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative parkinsonian syndromes include idiopathic Parkinson’s disease (PD), progressive supranuclear palsy (PSP), multiple system atrophy (MSA), and corticobasal syndrome (CBS). Although the clinical course and neurological findings are indispensable for disease monitoring, biomarkers that reflect the underlying pathophysiology are important to further understand these diseases.
Homovanillic acid (HVA) is a major metabolite of dopamine that is metabolized by monoamine oxidase and catechol-O-methyltransferase (Mena et al. 1984). Since previous studies have shown that the cerebrospinal fluid (CSF) concentration of HVA is decreased in patients with untreated PD, increases after the introduction of levodopa therapy, and correlates with motor impairment in patients with PD, it is generally considered that low CSF HVA concentration reflects the depletion of dopamine in the brain, mainly in the nigrostriatal system (Jiménez-Jiménez et al. 2014; Kremer et al. 2021; Mena et al. 1984; Stefani et al. 2017). Although a previous multicenter study questioned the utility of its measurement as a disease progression marker (Parkinson Study Group 1995), a recent single-center study using a better measurement protocol suggested its utility in evaluating nigrostriatal pathway damage (Kremer et al. 2021). CSF HVA measurement can also be useful in parkinsonian syndromes besides PD (Duvoisin et al. 1987).
The dopamine transporter (DAT) is a transmembrane protein that regulates the reuptake of dopamine, located at the presynaptic terminal of the dopaminergic neuron axon in the striatum (Booij et al. 1997; Palermo and Ceravolo 2019). Striatal DAT binding on DAT single-photon emission computed tomography (SPECT) has been proposed to represent the amount of DAT (Booij et al. 1997; Palermo and Ceravolo 2019). While it is widely used to assess presynaptic dopaminergic deficits in the diagnosis of parkinsonian syndromes (Booij et al. 1997), it remains to be known what the quantitative measurement of striatal DAT binding intensity reflects (Brücke and Brücke 2022). Although several autopsy studies have reported that antemortem striatal DAT binding is proportional to the number of nigral dopaminergic cells at autopsy (Snow et al. 1993; Colloby et al. 2012; Kraemmer et al. 2014), others have reported conflicting results (Saari et al. 2017; Honkanen et al. 2019). Studies using autopsy brains may have some limitations, including the time interval and effect of dopaminergic treatment.
As these examinations are both considered to be related to dopaminergic deficits in the central nervous system, mainly in the nigrostriatal system (Mena et al. 1984), the results of these two tests would correlate with each other. However, the association between the two has not been investigated among parkinsonian syndromes other than PD. A demonstration of this correlation would clarify the clinical significance of striatal DAT binding. Moreover, although striatal DAT binding has been previously reported to be lower in PSP than in PD and MSA (Badoud et al. 2016; Kaasinen et al. 2019), it is unknown whether the difference reflects the pathophysiological differences between diseases, since disease duration and severity were not consistent among the diagnoses in these studies. Comparing the correlations between each diagnosis would be useful in determining the cause of the difference.
In this study, we aimed to elucidate the clinical significance of DAT SPECT by examining the association between CSF HVA concentration and striatal DAT binding in each parkinsonian syndrome and discuss the differences in the pathophysiology by comparing them among each diagnosis after adjustment.
Materials and methods
Patients
This study was approved by the Institutional Review Board of the Tokyo Metropolitan Institute of Gerontology and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all participants or their caregivers. In this study, we retrospectively recruited patients who were diagnosed with parkinsonian syndromes, or Alzheimer’s disease (AD) as disease controls, and underwent both CSF HVA measurement and 123I-ioflupane SPECT at our hospital between March 2014 and June 2022. The interval between the two tests was < 3 months. We excluded patients who had other known neurological comorbidities or had ever been on medications that could affect the test results, such as anti-parkinsonian drugs, sulpiride, or mirtazapine (Kadoguchi et al. 2014) before HVA measurement and those drugs previously reported to affect DAT SPECT results (Kägi et al. 2010). Patients with clinical diagnoses of PD fulfilling the UK Parkinson’s Disease Society Brain Bank clinical diagnostic criteria (Hughes et al. 1992), probable PSP according to the 2017 MDS clinical diagnostic criteria (Höglinger et al. 2017), probable MSA according to the second consensus criteria (Gilman et al. 2008), CBS fulfilling the modified Cambridge criteria (Mathew et al. 2012), and AD dementia confirmed as A + T + N + by CSF biomarkers according to the 2018 National Institute on Aging-Alzheimer’s Association research framework (Jack et al. 2018) were included. Clinical data, including age, sex, past medical history, presenting symptoms, clinical course, medications, neurological findings including the Geriatric Depression Scale (GDS), and cognitive function tests such as the Mini-Mental State Examination (MMSE) and Frontal Assessment Battery (FAB) at the time CSF analysis was performed, were retrospectively collected for all patients.
CSF analysis
CSF was obtained via lumbar puncture in all patients. The first 3 mL of CSF was used for cell counting and routine biochemical testing, and an additional 2 mL was collected directly in polypropylene tubes. CSF HVA concentration was measured using a high-performance liquid chromatography system equipped with electrochemical sensors, as previously described (Morimoto et al. 2017).
SPECT imaging
DAT SPECT images were acquired 3 h after intravenous administration of 185 MBq of 123I-N-ω-fluoropropyl-2β-carbomethoxy-3β-(4-iodophenyl)nortropane (123I-ioflupane, DaT SCAN®, Nihon Medi-Physics) using a gamma camera Infinia Hawkeye 4 (GE Healthcare, Milwaukee, WI) equipped with an extended low-energy general-purpose collimator. Imaging parameters were as follows: matrix size, 128 × 128; pixel size, 3.22 mm; and energy window, 159 keV ± 10%. Data were acquired for 34 min and reconstructed using an ordered subset expectation maximization method (iteration, 6; subset, 10) on a Xeleris workstation (GE Healthcare) without attenuation correction or scatter correction.
The specific binding ratio (SBR) of the striatal DAT binding was semi-quantitatively calculated with DAT VIEW software (Nihon Medi-Physics, Tokyo, Japan) using the Southampton method (Tossici-Bolt et al. 2006) after phantom calibration, according to a previously reported method (Matsuda et al. 2018). The mean of the left and right SBRs was used to evaluate the association in the analyses. The asymmetry index (A.I.) of the SBR was calculated using software.
Statistics
Categorical variables were compared using the χ2 test. Normally distributed continuous variables were expressed as mean ± standard deviation and were compared using analysis of variance, while continuous variables without a normal distribution were expressed as median (interquartile range) and were compared using the Kruskal–Wallis test among each diagnosis. Pearson’s correlation test was used to verify the correlation between HVA concentration and SBR. In disease groups for which a significant correlation between the two was identified, we also conducted a one-way analysis of covariance (ANCOVA) to evaluate the differences in SBRs among each diagnosis, controlling for CSF HVA concentrations. The estimated SBR values when the CSF HVA concentrations were aligned to the overall average were compared for each diagnosis. Statistical significance was set at p < 0.05 and was adjusted according to the Bonferroni correction for multiple comparisons.
All statistical analyses were performed using R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical features of the patient groups
A total of 74 patients with PD, 13 with PSP, 12 with MSA, six with CBS, and nine with AD as disease controls fulfilled the inclusion criteria. Four patients with PD and one with PSP were excluded from the analyses because of comorbidities. The MSA patients consisted of five with MSA-P and seven with MSA-C. MMSE scores were recorded in 56 patients with PD, 11 with MSA, and all patients with PSP, CBS, or AD. FAB was recorded in all patients whose MMSE scores were recorded, except for one patient with PD and one with AD. The GDS was recorded in 54 patients with PD, 11 with MSA, eight with PSP, four with CBS, and five with AD. Two patients with PSP were conducted autopsy. In both cases, intracerebral aggregation of four repeat-tau neurofibrillary tangles and tufted astrocytes was observed, and consistent with both decreased CSF HVA concentration and low striatal DAT binding, melanin-containing neurons were depleted in the substantia nigra (Table S1 and Fig. S1 provided as Online Resource).
Patient characteristics are presented in Table 1. No significant difference was observed among the diagnoses regarding age, sex, duration of symptoms, interval period, or GDS. The mean Hoehn–Yahr score was lower in patients with PD than in those with PSP (p = 0.006, after p-value correction for multiple comparisons). The mean MMSE score was higher in patients with PD than in patients with PSP (p < 0.001), CBS (p = 0.003), and AD (p < 0.001), and was lower in patients with PSP than in those with MSA (p < 0.001). The A.I. was also significantly lower in patients with PD than in those with PSP (p = 0.011), and in AD than in those with PSP (p = 0.002).
Correlations between CSF HVA concentration and SBR of striatal DAT binding
Compared with patients with AD, CSF HVA concentration was significantly lower in those with PD (p < 0.001), PSP (p = 0.017), or MSA (p = 0.001), although the differences among each parkinson syndrome were relatively small. The mean SBR was significantly lower in patients with PD (p < 0.001), PSP (p < 0.001), or CBS (p = 0.013) than in AD, and it was significantly lower in PSP than in MSA (p = 0.043), even after correction for multiple comparisons.
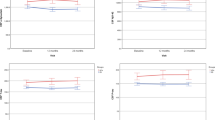
The association between the CSF HVA concentration and SBR was examined for each diagnosis. The correlation was significant in patients with PD (r = 0.34, p = 0.004) and PSP (r = 0.77, p = 0.004) but not in those with MSA (r = 0.24, p = 0.45), CBS (r = 0.15, p = 0.78), or AD (r = 0.33, p = 0.40). The scatter plot of patients with regression lines is shown in Fig. 1, and the distribution of SBR for each diagnosis is shown in Fig. 2a.
Distributions of CSF HVA concentrations and calibrated average SBRs from DAT SPECT in each diagnosis: PD a PSP b MSA c CBS d and AD as disease controls (e). A scatter plot is shown with the regression lines for each diagnosis. Significant correlations were observed between the patients with PD (r = 0.34, p = 0.004) and PSP (r = 0.77, p = 0.004). AD Alzheimer’s disease, CBS corticobasal syndrome, CSF cerebrospinal fluid, DAT dopamine transporter, HVA homovanillic acid, MSA multiple system atrophy, PD Parkinson’s disease, PSP progressive supranuclear palsy, SBR specific binding ratio, SPECT single-photon emission computed tomography
Bar graphs displaying the distribution of SBR in each diagnosis. a The mean values of SBR in each diagnosis are shown as bar charts. Standard deviations are shown as error bars. Compared with patients with AD, SBR was significantly lower in patients with PD (p < 0.001), PSP (p < 0.001), or CBS (p = 0.013), and it was significantly lower in PSP than in MSA (p = 0.043), after p-value correction for multiple comparisons. b The estimated values of SBR in PD and PSP, for which a significant correlation was identified, when CSF HVA concentrations were aligned to the overall average by analysis of covariance with CSF HVA concentrations as covariates are shown as bar charts. The SBR was significantly lower in patients with PSP than in those with PD (p = 0.037). The error bars indicate a standard error. *p < 0.05, ***p < 0.001. CBS corticobasal syndrome, CSF cerebrospinal fluid, HVA homovanillic acid, MSA multiple system atrophy, PD Parkinson’s disease, PSP progressive supranuclear palsy, SBR specific binding ratio
Comparison of SBR among each diagnosis
We also compared striatal DAT binding after controlling for the CSF HVA concentration between PD and PSP, for which a significant correlation was identified. After confirming that the interaction effect was not significant (p = 0.24), we conducted an ANCOVA with CSF HVA concentrations as covariates. In the analysis, the SBR was significantly lower in patients with PSP than in those with PD (p = 0.037). Bar charts considering the covariates are shown in Fig. 2b.
Discussion
A significant correlation between CSF HVA concentration and SBR of striatal DAT binding was observed not only in patients with PD, but also in those with PSP. Furthermore, striatal DAT binding was lower in PSP than in those with PD, after adjusting for CSF HVA concentration.
The correlation between CSF HVA concentration and striatal DAT binding in patients with PD and PSP indicates the clinical significance of DAT SPECT. The number of previous studies comparing CSF HVA concentrations and striatal DAT binding is scarce, and these studies were limited to patients with PD. Ishibashi et al. (2010) found a significant correlation (r = 0.76, p < 0.01) between CSF HVA concentrations and the striatal uptake of 11C-2β-carbomethoxy-3β-(4-fluorophenyl) tropane positron emission tomography in drug naïve PD patients (n = 21). Kremer et al. (2021) reported CSF HVA/dopamine correlating with 123I-ioflupane SPECT uptake ratios of the mean caudate (r = 0.28, p < 0.01) and ipsilateral caudate nucleus (r = 0.29, p < 0.01) in patients with PD (n = 95). As for the comparison of dopaminergic imaging with neuropathology findings, several autopsy studies have reported correlations between striatal DAT binding and the number of nigral dopaminergic cells (Snow et al. 1993; Colloby et al. 2012; Kraemmer et al. 2014). On the other hand, in studies limited to patients with parkinsonian syndromes, no correlation was found between striatal DAT binding and substantia nigra cell counts (Saari et al. 2017) or striatal dopaminergic axons (Honkanen et al. 2019) at autopsy. In a study in monkeys with a one-sided 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) lesion, there was also no link between striatal DAT binding and cell density of dopaminergic neurons in the substantia nigra when the cell loss exceeded 50%, while the uptake correlated with striatal dopamine levels throughout the full range of dopaminergic cell loss (Karimi et al. 2013). Since a low CSF HVA concentration has been proposed to reflect the depletion of dopamine in the brain, the results of our study suggest that striatal DAT binding correlates with dopamine levels in the brain both in PD and PSP, although further research is required to elucidate the mechanism.
The lower SBR in PSP than in PD after adjusting for CSF HVA concentration may be attributable to the difference in pathophysiology. Several previous studies have reported that striatal DAT binding is lower in patients with PSP than in those with PD and MSA (Badoud et al. 2016; Kaasinen et al. 2019). However, since the baseline characteristics, including disease duration and severity, were not consistent among disease groups in these studies, it was uncertain whether the differences reflect pathophysiological differences between diseases. Although there were no differences in baseline characteristics such as age, sex, or duration of symptoms in our study, it was difficult to match disease severity because of the different nature of the diseases. Therefore, we compared striatal DAT binding among each diagnosis after controlling for CSF HVA concentration. Our results showed that striatal DAT binding was lower in PSP patients than in PD patients, even after adjusting for CSF HVA values. Since all patients underwent CSF collection before the initiation of dopaminergic treatment and the intervals between the two tests were short within 3 months, it is unlikely that the medication or the progression during the intervals influenced the results. These results suggest that striatal DAT reduction is more advanced in patients with PSP than in those with PD at equivalent dopamine levels in the brain. The differences in the pathophysiology of each diagnosis may underlie the discrepancy in striatal DAT binding. As DAT is a protein expressed in the dopaminergic neuron terminals in the striatum, several factors have been assumed to contribute to striatal DAT reduction, including dopaminergic cell loss, axonal dysfunction (Cheng et al. 2010; Kneynsberg et al. 2017; Koziorowski et al. 2021; Schirinzi et al. 2016), and compensatory downregulation of DAT at the presynaptic terminal (Lee et al. 2000; Palermo and Ceravolo 2019). The relative reduction in striatal DAT in PSP may be due to the relative severity of axonal dysfunction or downregulation of DAT at the presynaptic terminal, although we cannot rule out the possibility that CSF HVA values are increased due to differences in the dopamine turnover (Kish et al. 1985; Palermo and Ceravolo 2019), reduction in delivery from the brain into the CSF (Rapoport et al. 2004), or dopamine levels outside the nigrostriatal pathway (Ruberg et al. 1985).
This study had several limitations. First, the number of cases was rather limited, especially for atypical parkinsonian syndromes. The correlations could have been significant if evaluated in a larger number of patients with MSA and CBS, considering the variability in each test result. Second, the diagnoses were based on clinical criteria rather than neuropathological examinations. Only two cases with PSP were performed the autopsy in this study. Although studies with more cases with neuropathologically confirmed diagnoses and comparing those findings would be desirable, since the diagnostic criteria have been well-established and most patients have been followed up by neurologists to review their diagnoses, we presume that the possibility of misdiagnosis would be minimal. Moreover, the Southampton method, which we used in this study for the analysis of the striatal DAT binding, does not allow the analysis by separation of striatal subregions. It has been reported that the striatal DAT binding is lower in patients with PSP than in those with PD or MSA-P, especially in the caudate (Chen et al. 2022; Kaasinen et al. 2019). Future studies should consider evaluating the striatal DAT binding of each subregion separately and comparing the differences among each diagnosis.
Our study showed that striatal DAT binding correlated with the CSF concentration of HVA, a major metabolite of dopamine, in both PD and PSP, and that striatal DAT binding in PSP was significantly lower than that in PD, adjusting for CSF HVA concentration. Both CSF HVA and striatal DAT binding are useful ancillary markers for assessing dopamine levels in the brains of patients with PD and PSP. Further discovery could be expected by comparing DAT SPECT findings with CSF biomarkers, such as HVA.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Badoud S, Van De Ville D, Nicastro N, Garibotto V, Burkhard PR, Haller S (2016) Discriminating among degenerative parkinsonisms using advanced (123)I-ioflupane SPECT analyses. Neuroimage Clin 12:234–240. https://doi.org/10.1016/j.nicl.2016.07.004
Booij J, Tissingh G, Boer GJ et al (1997) [123I]FP-CIT SPECT shows a pronounced decline of striatal dopamine transporter labelling in early and advanced Parkinson’s disease. J Neurol Neurosurg Psychiatry 62(2):133–140. https://doi.org/10.1136/jnnp.62.2.133
Brücke T, Brücke C (2022) Dopamine transporter (DAT) imaging in Parkinson’s disease and related disorders. J Neural Transm (vienna) 129(5–6):581–594. https://doi.org/10.1007/s00702-021-02452-7
Chen QS, Li XY, Li L et al (2022) Dopamine transporter imaging in progressive supranuclear palsy: severe but nonspecific to subtypes. Acta Neurol Scand 146(3):237–245. https://doi.org/10.1111/ane.13653
Cheng HC, Ulane CM, Burke RE (2010) Clinical progression in Parkinson disease and the neurobiology of axons. Ann Neurol 67(6):715–725. https://doi.org/10.1002/ana.21995
Colloby SJ, McParland S, O’Brien JT, Attems J (2012) Neuropathological correlates of dopaminergic imaging in Alzheimer’s disease and Lewy body dementias. Brain J Neurol 135(Pt 9):2798–2808. https://doi.org/10.1093/brain/aws211
Duvoisin RC, Golbe LI, Lepore FE (1987) Progressive supranuclear palsy. Can J Neurol Sci 14(3 Suppl):547–554. https://doi.org/10.1017/S0317167100038099
Gilman S, Wenning GK, Low PA et al (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71(9):670–676. https://doi.org/10.1212/01.wnl.0000324625.00404.15
Höglinger GU, Respondek G, Stamelou M et al (2017) Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Mov Disord 32(6):853–864. https://doi.org/10.1002/mds.26987
Honkanen EA, Saari L, Orte K et al (2019) No link between striatal dopaminergic axons and dopamine transporter imaging in Parkinson's disease. Mov Disord 34(10):1562–1566. https://doi.org/10.1002/mds.27777
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184. https://doi.org/10.1136/jnnp.55.3.181
Ishibashi K, Kanemaru K, Saito Y et al (2010) Cerebrospinal fluid metabolite and nigrostriatal dopaminergic function in Parkinson’s disease. Acta Neurol Scand 122(1):46–51. https://doi.org/10.1111/j.1600-0404.2009.01255.x
Jack CR Jr, Bennett DA, Blennow K et al (2018) NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement 14(4):535–562. https://doi.org/10.1016/j.jalz.2018.02.018
Jiménez-Jiménez FJ, Alonso-Navarro H, García-Martín E, Agúndez JA (2014) Cerebrospinal fluid biochemical studies in patients with Parkinson’s disease: toward a potential search for biomarkers for this disease. Front Cell Neurosci 8:369. https://doi.org/10.3389/fncel.2014.00369
Kaasinen V, Kankare T, Joutsa J, Vahlberg T (2019) Presynaptic striatal dopaminergic function in atypical parkinsonism: a metaanalysis of imaging studies. J Nucl Med 60(12):1757–1763. https://doi.org/10.2967/jnumed.119.227140
Kadoguchi N, Okabe S, Yamamura Y et al (2014) Mirtazapine has a therapeutic potency in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced mice model of Parkinson’s disease. BMC Neurosci 15:79. https://doi.org/10.1186/1471-2202-15-79
Kägi G, Bhatia KP, Tolosa E (2010) The role of DAT-SPECT in movement disorders. J Neurol Neurosurg Psychiatry 81(1):5–12. https://doi.org/10.1136/jnnp.2008.157370
Karimi M, Tian L, Brown CA et al (2013) Validation of nigrostriatal positron emission tomography measures: critical limits. Ann Neurol 73(3):390–396. https://doi.org/10.1002/ana.23798
Kish SJ, Chang LJ, Mirchandani L, Shannak K, Hornykiewicz O (1985) Progressive supranuclear palsy: relationship between extrapyramidal disturbances, dementia, and brain neurotransmitter markers. Ann Neurol 18(5):530–536. https://doi.org/10.1002/ana.410180504
Kneynsberg A, Combs B, Christensen K, Morfini G, Kanaan NM (2017) Axonal degeneration in tauopathies: disease relevance and underlying mechanisms. Front Neurosci 11:572. https://doi.org/10.3389/fnins.2017.00572
Koziorowski D, Figura M, Milanowski ŁM et al (2021) Mechanisms of neurodegeneration in various forms of parkinsonism-similarities and differences. Cells 10(3):656. https://doi.org/10.3390/cells10030656
Kraemmer J, Kovacs GG, Perju-Dumbrava L, Pirker S, Traub-Wei-dinger T, Pirker W (2014) Correlation of striatal dopamine transporter imaging with post mortem substantia nigra cell counts. Mov Disord 29(14):1767–1773. https://doi.org/10.1002/mds.25975
Kremer T, Taylor KI, Siebourg-Polster J et al (2021) Longitudinal analysis of multiple neurotransmitter metabolites in cerebrospinal fluid in early Parkinson’s disease. Mov Disord 36(8):1972–1978. https://doi.org/10.1002/mds.28608
Lee CS, Samii A, Sossi V et al (2000) In vivo positron emission tomographic evidence for compensatory changes in presynaptic dopaminergic nerve terminals in Parkinson’s disease. Ann Neurol 47(4):493–503. https://doi.org/10.1002/1531-8249(200004)47:4%3c493::AID-ANA13%3e3.0.CO;2-4
Mathew R, Bak TH, Hodges JR (2012) Diagnostic criteria for corticobasal syndrome: a comparative study. J Neurol Neurosurg Psychiatry 83(4):405–410. https://doi.org/10.1136/jnnp-2011-300875
Matsuda H, Murata M, Mukai Y et al (2018) Japanese multicenter database of healthy controls for [123I]FP-CIT SPECT. Eur J Nucl Med Mol Imaging 45(8):1405–1416. https://doi.org/10.1007/s00259-018-3976-5
Mena MA, Aguado EG, de Yebenes JG (1984) Monoamine metabolites in human cerebrospinal fluid HPLC/ED method. Acta Neurol Scand 69(4):218–225. https://doi.org/10.1111/j.1600-0404.1984.tb07804.x
Morimoto S, Takao M, Hatsuta H et al (2017) Homovanillic acid and 5-hydroxyindole acetic acid as biomarkers for dementia with Lewy bodies and coincident Alzheimer’s disease: an autopsy-confirmed study. PLoS ONE 12(2):e0171524. https://doi.org/10.1371/journal.pone.0171524
Palermo G, Ceravolo R (2019) Molecular imaging of the dopamine transporter. Cells 8(8):872. https://doi.org/10.3390/cells8080872
Parkinson Study Group (1995) Cerebrospinal fluid homovanillic acid in the DATATOP study on Parkinson’s disease. Arch Neurol 52(3):237–245. https://doi.org/10.1001/archneur.1995.00540270025015
Rapoport SI, Schapiro MB, May C (2004) Reduced brain delivery of homovanillic acid to cerebrospinal fluid during human aging. Arch Neurol 61(11):1721–1724. https://doi.org/10.1001/archneur.61.11.1721
Ruberg M, Javoy-Agid F, Hirsch E et al (1985) Dopaminergic and cholinergic lesions in progressive supranuclear palsy. Ann Neurol 18(5):523–529. https://doi.org/10.1002/ana.410180503
Saari L, Kivinen K, Gardberg M et al (2017) Dopamine transporter imaging does not predict the number of nigral neurons in Parkinson disease. Neurology 88(15):1461–1467. https://doi.org/10.1212/wnl.0000000000003810
Schirinzi T, Madeo G, Martella G et al (2016) Early synaptic dysfunction in Parkinson’s disease: insights from animal models. Mov Disord 31(6):802–813. https://doi.org/10.1002/mds.26620
Snow BJ, Tooyama I, McGeer EG et al (1993) Human positron emission tomographic [18F]fluorodopa studies correlate with dopamine cell counts and levels. Ann Neurol 34(3):324–330. https://doi.org/10.1002/ana.410340304
Stefani A, Pierantozzi M, Olivola E et al (2017) Homovanillic acid in CSF of mild stage Parkinson’s disease patients correlates with motor impairment. Neurochem Int 105:58–63. https://doi.org/10.1016/j.neuint.2017.01.007
Tossici-Bolt L, Hoffmann SM, Kemp PM, Mehta RL, Fleming JS (2006) Quantification of [123I]FP-CIT SPECT brain images: an accurate technique for measurement of the specific binding ratio. Eur J Nucl Med Mol Imaging 33(12):1491–1499. https://doi.org/10.1007/s00259-006-0155-x
Acknowledgements
We would like to thank all the patients and their families for participating in this study. We also thank members of the Department of Diagnostic Radiology and the Department of Neuropathology (Brain Bank for Aging Research) for their technical assistance.
Funding
This study was supported by Intramural Research Grants from Tokyo Metropolitan Geriatric Hospital (M. Kurihara, K.Kanemaru), Research Grant from Integrated Research Initiative for Living Well with Dementia (M. Kameyama), JSPS KAKENHI Grant Numbers JP22H04923 (CoBiA) (Y.Saito, S.Murayama) and JP22K15740 (T.Matsubara), Grants-in Aid from the Research Committee of CNS Degenerative Diseases, Research on Policy Planning and Evaluation for Rare and Intractable Diseases, Health, Labour and Welfare Sciences Research Grants, the Ministry of Health, Labour and Welfare, Japan, Grant No. 20FC1049 (Y.Saito, S.Murayama), and AMED under Grant No. JP22wm0425019 (Y.Saito, S.Murayama) and JP22dk0207057h0001 (A. Iwata).
Author information
Authors and Affiliations
Contributions
RG, MK, and MK contributed to the study conception and design. The study was supervised by AI. Data acquisition was performed by all authors. Data analysis and interpretation were performed by RG, MK, MK, KH, RI, MH, YN, TM, KK, SM, YS, and AI. The first draft of the manuscript was written by RG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Ethical approval
This study was approved by the Institutional Review Board of the Tokyo Metropolitan Institute of Gerontology and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
Written informed consent was obtained from all participants or their caregivers.
Consent for publication
All images are entirely unidentifiable and there are no details on the individuals reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
702_2023_2611_MOESM1_ESM.docx
Supplementary file1 Fig. S1 Neuropathological findings. Both cases displayed moderate to severe loss of pigmentation in the substantia nigra (a, e), where globose-shaped neurofibrillary tangles were detected by Hematoxylin Eosin staining (b, f) and immunostaining for four repeat-tau (c, g). Tufted astrocytes were present in the midbrain tegmentum (d) and the putamen (h). These findings support the diagnosis of progressive supranuclear palsy. Scale bars: 1 cm (a, e), 20 μm (b-d, f-h) (DOCX 1672 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goto, R., Kurihara, M., Kameyama, M. et al. Correlations between cerebrospinal fluid homovanillic acid and dopamine transporter SPECT in degenerative parkinsonian syndromes. J Neural Transm 130, 513–520 (2023). https://doi.org/10.1007/s00702-023-02611-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-023-02611-y