Abstract
Purpose
Intraoperative neuromonitoring (IONM) aims to preserve facial nerve (FN) function during vestibular schwannoma (VS) surgery. However, current techniques such as facial nerve motor evoked potentials (FNMEP) or electromyography (fEMG) alone are limited in predicting postoperative facial palsy (FP). The objective of this study was to analyze a compound fEMG/FNMEP approach.
Methods
Intraoperative FNMEP amplitude and the occurrence of fEMG-based A-trains were prospectively determined for the orbicularis oris (ORI) and oculi (OCU) muscle in 322 VS patients. Sensitivity and specificity of techniques to predict postoperative FN function were calculated. Confounding factors as tumor size, volume of intracranial air, or IONM duration were analyzed.
Results
A relevant immediate postoperative FP was captured in 105/322 patients with a significant higher risk in large VS. While fEMG demonstrated a high sensitivity (77% and 86% immediately and 15 month postoperative, respectively) for identifying relevant FP, specificity was low. In contrast, FNMEP have a significantly higher specificity of 80.8% for predicting postoperative FP, whereas the sensitivity is low. A retrospective combination of techniques demonstrated still an incorrect prediction of FP in ~ 1/3 of patients.
Conclusions
FNMEP and fEMG differ in sensitivity and specificity to predict postoperative FP. Although a combination of IONM techniques during VS surgery may improve prediction of FN function, current techniques are still inaccurate. Further development is necessary to improve IONM approaches for FP prediction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular schwannomas (VS) account for ~80% of all tumors of the cerebellopontine angle, constituting the most common entity in this location [13, 23, 38]. Due to the anatomic relation to the internal auditory canal and the traversing vestibulocochlear (VIII) and facial (VII) nerve, surgical resection of VS entails the risk of hearing loss and facial palsy (FP). Continuous intraoperative neuromonitoring (IONM) and advances in surgical techniques have improved anatomical facial nerve (FN) preservation. However, literature suggests that severe FP still occurs in 7–15% of the cases, with tumor size as the most important predictive factor [15] and potential reduction of physical and mental health as clinical consequence [21].
IONM is accepted as a general standard in VS surgery and is intended to provide anatomic identification of the FN, protect against potentially damaging events causing functional FN deterioration, and prognostically predict postoperative FN function [31]. However, a standardized IONM approach is lacking. Depending on the center facial electromyography (fEMG) [27, 28, 33], facial nerve motor–evoked potentials (FNMEP) via transcranial electrical stimulation (TES) [1, 3, 4, 22], or a combination of techniques are used for monitoring. fEMG can be performed continuously, but quantitative analysis of pathological A-trains during surgery is difficult. Even with techniques for automated processing of A-train duration, previous studies yield positive predictive values of only ~64% for predicting FN outcome [29, 30]. FNMEP monitoring allows simple analyses of final-to-baseline amplitudes and can be performed frequently but not continuously like the fEMG. Positive predictive values for FNMEP also range only between 53 and 61% [31].
In conclusion, previous studies have demonstrated limited predictive power of monitoring techniques. The analyses, however, mostly enrolled only a small number of patients (< 100 persons). In addition, an evaluation that combines techniques and systematically investigates confounding factors is lacking. This study aims to describe the FN monitoring technique used in our tertiary neurosurgical center and analyses the predictive power of methods in 322 patients.
Methods
Clinical data
This retrospective analysis of prospectively collected data enrolled 322 patients (49.4 ± 13.1 years, 169 female) who underwent neurosurgical resection of a VS at the Department of Neurosurgery of the University of Tuebingen between 2011 and 2016. Decision for resection was based on patients’ age, tumor size, VS-associated symptoms and patients’ therapeutic preference. Patients with prior (radio-)surgery of the VS and preoperative facial nerve palsy were excluded. Tumor extent was graded according to the Koos classification (Koos 1: purely intrameatal, Koos 2: intra- and extrameatal, Koos 3: filling the cerebellopontine cistern, Koos 4: compressing or shifting the brainstem). Intraoperative positioning was dependent on tumor size. The majority of patients with Koos 1 and 2 tumors were operated in supine position, whereas Koos 3 and 4 tumors were operated in semi-sitting position. The study was approved by the local ethics committee of the Eberhard Karls University Tuebingen and performed in accordance with the Declaration of Helsinki. Patients‘ characteristics are summarized in Table 1.
Intraoperative neuromonitoring (IONM)
Electrophysiological measurements during the surgery were performed by experienced electrophysiologists using an Endeavor monitoring unit (Endeavor, Viasys Healthcare, Madison, WI, USA). In addition to continuously electromyography (fEMG) of the facial nerve and facial motor evoked potentials (FNMEP), motor (MEP) and somatosensory evoked potentials (SEP) of the hands and legs were monitored, as described in detail previously [1, 4]. In patients with tumors reaching the lower cranial nerves, EMG of the glossopharyngeal, vagal, accessory, and hypoglossal nerve was measured as well. Furthermore, brainstem auditory evoked potentials (BAEP) of the tumor side were monitored in patients with residual hearing function.
Transcranial electrical stimulation (TES) for FNMEP monitoring was performed using corkscrew-like electrodes, which were positioned at Cz and C3 or C4 according to the international 10/20 system for left or right sided stimulation, respectively (Fig. 1). Stimulation was always applied using one, three, or five rectangular pulses, ranging from 200 to 400 V with a 500-μs pulse duration and an interstimulus interval (ISI) of 2 ms. Facial potentials were recorded from needles placed in the orbicularis oculi (OCU) and oris (ORI) muscles of the affected and healthy side (Fig. 1). Stimulations with one and five pulses were matched to ensure that the facial nerve was not stimulated extracranially. The abductor pollicis brevis (APB) muscle was used as a control of the general motor cortical excitability. MEPs of the hands and legs were stimulated by C1 and C2. TES was performed intermittently with SEP and BAEP recordings. The surgeon was always informed prior to stimulation, as TES may cause undesirable movements. For facial nerve function estimation and further analyses, the best response before dural opening was used as baseline value. Final values were defined at the moment of dural closure, and the final-to-baseline amplitude (FBR) was estimated. FNMEP amplitude was defined as the voltage between the maximum positive and negative deflection of the waveforms. FNMEP latency was defined as the time from stimulus onset to the first wave deflection.
Schematic illustration of A the electrode positioning with corkscrew electrodes in Cz, C2 and C4 as well as needle electrodes in the orbicularis oris and oculi muscle and B the facial nerve motor evoked potentials (FNMEP) as well as facial nerve electromyography (fEMG) demonstrating A-trains in the orbicularis oculi muscle.
For the fEMG, the same needle electrodes in the OCU and ORI as for FNMEP were used. The occurrence of A-trains, which are considered pathological [33], was detected and reported to the surgeon.
Facial nerve function
Facial nerve function was categorized according to the House–Brackmann (HB) grading system within 1 week after the surgery (immediately postoperative) as well as 15 months after surgery by experienced neurosurgeons. HB grades I and II were classified as satisfactory, while HB grades III to VI were assessed as unsatisfactory.
Statistics
Statistical tests were performed using the SPSS (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.). Sensitivity, specificity, and positive and negative predictive values of FNMEP and fEMG to predict the FN outcome were determined by differentiating the occurrence of A-trains (yes/no) and using various amplitude FBR thresholds (0.5, 0.6, 0.7) in FNMEP (Table 2). The sensitivity (1) informs us how often the monitoring test (e.g., A-train yes or ORI-MEP <0.6) detects a facial palsy when postoperative a relevant facial palsy is apparent (true positive rate, TPR). The specificity (2) indicates how often the monitoring test detects “no palsy” while there is no postoperative facial palsy (true negative rate, TNR). The positive (PPV) predictive values are the proportions of patients with positive test results (e.g., A-train yes or ORI-MEP <0.6) who already have a facial palsy (3), while the negative predictive value (NPV) is the proportion of the cases giving negative test results who are already healthy (4) (Table 2)
Group differences of clinical characteristics (e.g., patients‘ age, tumor size) in patients with and without satisfactory FN outcome as well as true and false classified patients were determined by chi-squared or Kruskal-Wallis tests. Correlation analyses were performed by Spearman’s correlation. Statistical significance was considered at p < 0.05 for each statistical test.
Results
Patient cohort and surgical results
Continuous fEMG and FNMEP monitoring was performed in 322 patients (49.4 ± 13.1 years, 169 female) during VS surgery in semi-sitting (262/322) or supine (60/322) position (Table 1). In 83/322 (25.8%) patients, the VS corresponded to a tumor size Koos 1 or 2 and in 239/322 (74.2%) to Koos 3 or 4. Patients with preoperative facial nerve paresis were excluded. A total of 105 patients (32.6%) suffered from relevant facial nerve paresis (≥ HB III°) immediately postoperatively. At 15-month follow-up, most of them improved to HB I-II°, and 22/281 (6.8%) remained with HB ≥ III°. Forty-one patients (15 with HB I–II° and 36 with HB (≥ HB III° immediately postoperative) did not present for follow-up examination. Tumor size correlated significantly with the grade of postoperative facial palsy (r = 0.42, p < 0.001; Spearman’s). Only 12/83 (15%) patients with tumor size Koos 1 or 2 had relevant facial palsy, while 93/239 (39%) patients with tumor size Koos 3 or 4 suffered from postoperative facial nerve paresis ≥ HB III° immediately after surgery. This difference was also evident for positioning as Koos 1/2 mostly were treated in supine position, while Koos 3/4 VS are operated in semi-sitting position.
Predictive value of facial nerve EMG and MEP
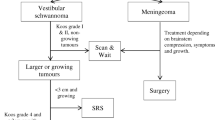
In a total of 216/322 (67.1%) patients, A-trains were detected during fEMG monitoring. Sensitivity for detecting a facial palsy ≥ HB III° was 77.1% immediately postoperative (days 1–6) and 86.4% 15 months postoperative. However, there was a low specificity of 37.8% for A-trains predicting facial nerve outcome (Table 3). These values resulted in a total of 163/322 (50.6%) correct classified patients (TP + TN), 135/322 (41.9%) false positive (FPR), and 24/322 (7.4%) false negative (FNR) detected patients by fEMG (Fig. 2A). There were no differences between correct classified patients (TPR + TNR) compared to FPR and FNR groups regarding age, gender, tumor size and side, positioning, or volume of postoperative pneumocephalus. In contrast, FNMEP final-to-baseline ratios showed overall a high specificity, but low sensitivity for predicting a relevant facial palsy ≥ HB III° (Table 3). FNMEP of the orbicularis oris muscle (ORI-MEP) had a significant higher predictive power than FNMEP of the orbicularis oculi (OCU-MEP). Hence, further FNMEP analysis and descriptions refer to the ORI-MEP with a 0.6-FBR. A total of 221/318 (69.5%) patients were classified correctly by these 0.6-FBR ORI-MEP, while the facial nerve outcome was false positive and negative predicted in 41/318 (12.9%) and 56/318 (17.6%) cases. In four patients, the ORI-MEP was not recordable.
Intraoperative facial nerve monitoring by electromyography (fEMG) and motor evoked potentials (FNMEP). A and B demonstrate separately the predictive values of the fEMG and FNMEP technique. C presents a combined monitoring approach with fEMG as screening and FNMEP as confirmatory test. FNR, false negative rate; FPR, false positive rate; HB, House-Brackmann score; ORI, orbicularis oris; TNR, true negative rate; TPR, true positive rate
A combined EMG/MEP-approach
Retrospectively, we analyzed a combined approach of fEMG and FNMEP monitoring based on the presented data (Fig. 2C). Diagnostic tests with a high sensitivity are well suited as screening test. Therefore, fEMG was used as screening test and only the 216 patients in whom intraoperative A-trains were detected were examined by 0.6-FBR ORI-MEP (confirmatory test). In two of the patients, no ORI-MEP was recordable. A total of 69/214 (32.2%) patients had a decline in ORI-MEP <0.6, whereas 145/214 (67.8%) patients had no decrease below the threshold. Forty out of the 69 (58%) patients with an ORI-MEP <0.6 showed a relevant postoperative facial paresis immediately postoperative and where therefore classified as TP. In contrast, 104/145 (71.7%) patients were classified true negative resulting in 144/214 (67%) correctly classified (TPR + TNR) cases in this cohort. However, there were still 41/145 (28.3%) or 41/214 (19.2%) which were considered false negative (FNR). To improve the combined approach in future, it should be therefore the main effort to better differentiate between true and false negative FNMEP in patients with detected A-trains and define relevant factors affecting measurements. However, while there was a trend of higher weights in the false negative group (H = 3.43, p = 0.064), we could not detect significant differences between the TNR and FNR group in our data (Table 4).
Impact of intracranial air on monitoring results
Since the previous analyses could not demonstrate any clear factors influencing the “false prediction,”, we further analyzed the influence of postoperative pneumocephalus (PP) in facial nerve monitoring, since an influence of PP on electrophysiological measurements has been postulated repeatedly. The mean intracranial air of the total cohort was 33.6 ± 33 ml. Patients operated in a semi-sitting position had a significantly larger amount of intracranial air than those operated supine (41.0 ± 32 ml and 1.0 ± 2 ml) (H = 132.86, p < 0.001). To analyze the influence of intracranial air on FNMEP, a subcohort analysis of patients who did not have relevant facial nerve palsy (Table 1) was performed, as there was no change in FNMEP due to surgical lesions in these patients. In this cohort of 217 patients (111 female), mean intracranial air was 35.8 ± 24 ml. There was no significant correlation of the volume of intracranial air to the 0.6-FBR ORI-MEP (r = −0.004, p = 0.957; Spearman’s). However, the final-to-baseline MEP amplitude ratio of the ipsilateral hand correlated significantly negative with the volume of intracranial air (r = −0.36; p < 0.001; Spearman’s) predisposing the hand MEP for estimating the amount of intracranial air.
Discussion
Intraoperative facial nerve monitoring is considered as a gold standard in VS surgery to preserve facial integrity [39]. The occurrence of A-trains is regarded as a warning criterion in fEMG monitoring (i.e., train-time criterion) [29, 30], while a reduction in amplitude of more than 40–50% is assessed as critical in FNMEP (i.e., final-to-baseline ratio, FBR) [5, 7, 8, 14, 41]. However, quantitative analysis of pathological A-trains with differentiation to other EMG patterns during surgery is difficult [29, 30, 33]. In addition, the fEMG has a high sensitivity with low specificity for predicting significant FN deterioration. In contrast, FNMEP has a better specificity with low sensitivity to predict significant FN deterioration [1, 7, 14, 41]. The present study analyzed the prognostic value of a combination of both techniques in a large cohort of >300 VS patients.
Our results demonstrate that facial outcome prediction remains incorrect in nearly one-third of patients by combining FNMEP and fEMG as presented. The subsequent purpose of further investigations has to be an improvement of this rating. However, there is little interpretive margin for the monitoring assistant during surgery with homogeneous, but false results of both techniques. Although monitoring methods in these cases provide an incorrect prediction, the homogeneous rating of different techniques suggests that the measurement works properly from a technical point of view. Other factors (e.g. anesthetics, blood pressure, temperature) may influence the FN outcome. Overall, 4.7% of our patient cohort were detected false negative by fEMG and FNMEP. In these cases, the facial nerve may be unaffected during surgery, while there are adverse factors immediately after the monitoring or surgery phase deteriorating the FN — e.g., fluctuations of blood pressure with hypotonia, which can lead to vascular events. This hypothesis is supported by the fact that various studies have demonstrated the neuroprotective value of vasoactive drugs (e.g., nimodipine) [29,30,31]. It has been shown that the occurrence of delayed facial palsy was more likely after the discontinuation of a nimodipine therapy and that patients with postoperative facial palsy had a better long-term outcome with nimodipine therapy [29, 31]. Thus, good blood pressure control and the administration of vasoactive drugs should be aspired in postoperative management. However, these factors cannot be controlled by the monitoring assistant intraoperatively. In this situation, the correct interpretation of discrepant results with e.g. true-positive A-trains in the screening test, but false-negative, stable FNMEP-amplitudes is crucial. The lower sensitivity of FNMEPs, which is responsible for this, can be improved by re-defining the critical threshold. Whereas previous studies mostly considered an amplitude reduction of 50% as relevant [5, 22, 41], our results — in line with other recent studies [7, 14] — demonstrated a higher predictive value of FN outcome for a threshold of 0.6 (i.e., an amplitude reduction of 40%). Furthermore, alternative FNMEP analysis techniques than the FBR analysis — as e.g., event-to-baseline amplitude or a minimal-to-baseline ratio — may can improve the sensitivity [14]. Alternatively to the improvement of fEMG and FNMEP analyses, an evoked facial nerve EMG within the cerebellopontine angle [6, 42] or the application of direct nerve stimulation (DNS) [11, 25, 35] as further monitoring technique is also possible. DNS enables anatomic identification of the FN. However, usually, it can only be applied intermittently, as the stimulation probe has to be used selective by the surgeon. The implementation of a combined surgical suction-and-mapping probe can partially resolve this problem by a continuous dynamic mapping [36]. However, as in VS surgery often a bimanual preparation technique [10, 40] is used, even such a probe cannot be used continuously. Furthermore, prognostic analyses based on proximal-to-distal amplitude ratios in DNS could demonstrate positive predictive values of only ~46% [35].
The stepwise monitoring approach (i.e., 1: fEMG as screening test, 2: FNMEP as confirmatory test) enables to reduce the high number of false positive detected A-trains by the FNMEP method. Nevertheless, in our study, 9% of patients were detected false positive by both techniques. Consequently, the false positive rate of the FNMEPs is also a matter of interest in facial nerve monitoring. It might be associated to intracranial air, patient temperature, depth of anesthesia, and fluctuations of the impedances or the excitability: The volume of postoperative pneumocephalus is often postulated as a source of error for false positive deterioration in motor evoked potentials. However, previous studies demonstrated inconclusive results with and without PP-associated MEP-changes [2, 17, 32]. Our results showed a deterioration of the hand MEP, whereas no air-dependent deterioration of the FNMEP could be demonstrated. This fact may be explained by the intraoperative positioning of the patient as well as the positioning of the electrodes: in semi-sitting position, the amount of pneumocephalus is usually higher than in supine position [18]. Since the air usually accumulates at the highest point, it can be assumed that the air is more likely to be present under electrodes C1 and C2 than under electrodes C3 and C4, which are used for measuring the FNMEP (Fig. 1).
Experimental studies in rats demonstrated a decrease of spinal motor evoked potentials in hypothermia [26]. In contrast, hyperthermia in combination with high impedances may increase noise and decrease the statistical power during electrophysiological monitoring [16]. While the influence of intraoperative impedance changes could be reduced by a current-regulated stimulation, spontaneous fluctuations of the cortical excitability with the consequence of a high intra-subject variability of the MEP amplitude [9, 19] could be addressed by alternative FNMEP analyses techniques than the FBR analysis. Previous studies considered the application of an event-to-baseline amplitude or a minimal-to-baseline ratio including a recovery value [14]. Here, the lowest amplitude value during the surgery is measured and related to the baseline amplitude as well as to the amplitude at the end of the surgery. Another method used is the threshold level method, in which the difference in stimulation intensity is evaluated while the response amplitude is kept constant by increasing the stimulation intensity [34, 37]. Greve et al. [12] used the non-lesional side as an additional evaluation criterion to the lesioned side. Finally, time frequency analysis, which has recently shown promising results in the analysis of motor potentials evoked by TMS [19, 20, 24], suggests a promising further development of facial nerve monitoring.
Limitations
While the number of patients analyzed and the use of combined monitoring techniques is the strength of the results presented, the retrospective evaluation is the major weakness. Especially in fEMG analyses, we could only differentiate between the occurrence of A-trains vs. the non-occurrence. A statement about the duration of the A-trains could not be made. Furthermore, in FNMEP analysis, only the FBR was documented, while event-to-baseline amplitude or a minimal-to-baseline ratio is lacking. Finally, we did not evaluate individual anesthetic dosages (e.g., analgesics, muscle relaxants) or body temperatures, which may have influenced the measurement. However, all patients were operated in a highly standardized surgical and anesthesiological setting, which has been described in previous studies [1]. Further prospective studies, which also investigate innovative analysis techniques such as time-frequency analysis, should address these limitations in future.
Conclusion
The combination of fMEP/FNMEP for monitoring the facial nerve still leads to significant false predictions of postoperative facial outcome. Thus, further development of the analysis techniques and parameters is necessary to better predict the facial nerve outcome and thus to guarantee the function-oncological outcome by an extensive resection on the one hand and a good facial function on the other hand.
Data availability
Data can be provided on reasonable request.
Abbreviations
- AUC:
-
area under the curve
- BAEP:
-
brainstem auditory evoked potential
- DNS:
-
direct nerve stimulation
- FBR:
-
final-to-baseline ratio
- fEMG:
-
facial electromyography
- FN:
-
facial nerve
- FNMEP:
-
facial nerve motor evoked potentials
- FNR:
-
false negative rate
- FP:
-
facial palsy
- FPR:
-
false positive rate
- NPV:
-
negative predictive value
- HB:
-
House-Brackmann score
- IONM:
-
intraoperative neuromonitoring
- MEP:
-
motor evoked potential
- OCU:
-
orbicularis oculi muscle
- ORI:
-
orbicularis oris muscle
- PP:
-
postoperative pneumocephalus
- PPV:
-
positive predictive value
- TES:
-
transcranial electrical stimulation
- TNR:
-
true negative rate
- TPR:
-
true positive rate
- VS:
-
vestibular schwannoma
References
Acioly MA, Liebsch M, Carvalho CH, Gharabaghi A, Tatagiba M (2010) Transcranial electrocortical stimulation to monitor the facial nerve motor function during cerebellopontine angle surgery. Neurosurgery. https://doi.org/10.1227/01.neu.0000369654.41677.b7
Acioly MA, Ebner FH, Hauser TK, Liebsch M, Carvalho CH, Gharabaghi A, Tatagiba M (2011) The impact of subdural air collection on intraoperative motor and somatosensory evoked potentials: Fact or myth? Acta Neurochir 153(5):1077–1085
Acioly MA, Gharabaghi A, Liebsch M, Carvalho CH, Aguiar PH, Tatagiba M (2011) Quantitative parameters of facial motor evoked potential during vestibular schwannoma surgery predict postoperative facial nerve function. Acta Neurochir 153(6):1169–1179
Acioly MA, Liebsch M, De Aguiar PHP, Tatagiba M (2013) Facial nerve monitoring during cerebellopontine angle and skull base tumor surgery: a systematic review from description to current success on function prediction. World Neurosurg. https://doi.org/10.1016/j.wneu.2011.09.026
Akagami R, Dong CCJ, Westerberg BD (2005) Localized transcranial electrical motor evoked potentials for monitoring cranial nerves in cranial base surgery. Neurosurgery. https://doi.org/10.1227/01.NEU.0000163486.93702.95
Amano M, Kohno M, Nagata O, Taniguchi M, Sora S, Sato H (2011) Intraoperative continuous monitoring of evoked facial nerve electromyograms in acoustic neuroma surgery. Acta Neurochir 153(5):1059–1067
Bhimrao SK, Le TN, Dong CC, Makarenko S, Wongprasartsuk S, Westerberg BD, Akagami R (2016) Role of facial nerve motor-evoked potential ratio in predicting facial nerve function in vestibular Schwannoma surgery both immediate and at 1 year. Otol Neurotol 37(8):1162–1167
Bovo N, Momjian S, Gondar R, Bijlenga P, Schaller K, Boëx C (2021) Sensitivity and negative predictive value of motor evoked potentials of the facial nerve. J Neurol Surg A Cent Eur Neurosurg 82(4):317–324
Butler AJ, Kahn S, Wolf SL, Weiss P (2005) Finger extensor variability in TMS parameters among chronic stroke patients. J Neuroeng Rehabil. https://doi.org/10.1186/1743-0003-2-10
Gharabaghi A, Samii A, Koerbel A, Rosahl SK, Tatagiba M, Samii M (2007) Preservation of function in vestibular schwannoma surgery. Neurosurgery 60(2 SUPPL.1):124–128
Grayeli AB, Guindi S, Kalamarides M, El Garem H, Smail M, Rey A, Sterkers O (2005) Four-channel electromyography of the facial nerve in vestibular schwannoma surgery: Sensitivity and prognostic value for short-term facial function outcome. Otol Neurotol 26(1):114–120
Greve T, Wang L, Katzendobler S, Geyer LL, Schichor C, Tonn JC, Szelényi A (2021) Bilateral and optimistic warning paradigms improve the predictive power of intraoperative facial motor evoked potentials during vestibular schwannoma surgery. Cancers (Basel). https://doi.org/10.3390/cancers13246196
Grey PL, Moffat DA, Hardy DG (1996) Surgical results in unusual cerebellopontine angle tumours. Clin Otolaryngol Allied Sci 21(3):237–243
Hiruta R, Sato T, Itakura T, Fujii M, Sakuma J, Bakhit M, Kojima T, Ichikawa M, Iwatate K, Saito K (2021) Intraoperative transcranial facial motor evoked potential monitoring in surgery of cerebellopontine angle tumors predicts early and late postoperative facial nerve function. Clin Neurophysiol 132(4):864–871
Hostettler IC, Jayashankar N, Bikis C et al (2021) Clinical studies and pre-clinical animal models on facial nerve preservation, reconstruction, and regeneration following cerebellopontine angle tumor surgery—a systematic review and future perspectives. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2021.659413
Kappenman ES, Luck SJ (2010) The effects of electrode impedance on data quality and statistical significance in ERP recordings. Psychophysiology 47(5):888–904
Kombos TH, Suess O, Pietilä T, Brock M (2000) Subdural air limits the elicitation of compound muscle action potentials by high-frequency transcranial electrical stimulation. Br J Neurosurg 14(3):240–243
Machetanz K, Leuze F, Mounts K, Trakolis L, Gugel I, Grimm F, Tatagiba M, Naros G (2020) Occurrence and management of postoperative pneumocephalus using the semi-sitting position in vestibular schwannoma surgery. Acta Neurochir 162(11):2629–2636
Machetanz K, Gallotti AL, Leao Tatagiba MT, Liebsch M, Trakolis L, Wang S, Tatagiba M, Gharabaghi A, Naros G (2021) Time-frequency representation of motor evoked potentials in brain tumor patients. Front Neurol. https://doi.org/10.3389/fneur.2020.633224
Machetanz K, Wiesinger L, Leao MT, Liebsch M, Trakolis L, Wang S, Gharabaghi A, Tatagiba M, Naros G (2021) Interhemispheric differences in time-frequency representation of motor evoked potentials in brain tumor patients. Clin Neurophysiol 132(11):2780–2788
Machetanz K, Lee L, Wang SS, Tatagiba M, Naros G (2023) Trading mental and physical health in vestibular schwannoma treatment decision. Front Oncol 13:1152833
Matthies C, Raslan F, Schweitzer T, Hagen R, Roosen K, Reiners K (2011) Facial motor evoked potentials in cerebellopontine angle surgery: technique, pitfalls and predictive value. Clin Neurol Neurosurg 113(10):872–879
Moffat DA, Ballagh RH (1995) Rare tumours of the cerebellopontine angle. Clin Oncol 7(1):28–41
Naros G, Machetanz K, Leao MT, Wang S, Tatagiba M, Gharabaghi A (2022) Impaired phase synchronization of motor-evoked potentials reflects the degree of motor dysfunction in the lesioned human brain. Hum Brain Mapp. https://doi.org/10.1002/hbm.25812
Neff BA, Ting J, Dickinson SL, Welling DB (2005) Facial nerve monitoring parameters as a predictor of postoperative facial nerve outcomes after vestibular schwannoma resection. Otol Neurotol 26(4):728–732
Oro J, Haghighi SS (1992) Effects of altering core body temperature on somatosensory and motor evoked potentials in rats. Spine (Phila Pa 1976) 17(5):498–503
Prass RL, Lüders H (1986) Acoustic (loudspeaker) facial electromyographic monitoring. Neurosurgery 19(3):392–400
Prass RL, Kinney SE, Hardy RW, Hahn JF, Luders H (1987) Acoustic (loudspeaker) facial EMG monitoring: II. Use of evoked EMG activity during acoustic neuroma resection. Otolaryngol Head Neck Surg 97(6):541–551
Prell J, Rampp S, Romstöck J, Fahlbusch R, Strauss C (2007) Train time as a quantitative electromyographic parameter for facial nerve function in patients undergoing surgery for vestibular schwannoma. J Neurosurg 106(5):826–832
Prell J, Rachinger J, Scheller C, Alfieri A, Strauss C, Rampp S (2010) A real-time monitoring system for the facial nerve. Neurosurgery 66(6):1064–1073
Prell J, Strauss C, Plontke SK, Rampp S (2017) Intraoperative Funktionsüberwachung des N. facialis: Operationen an Vestibularisschwannomen. HNO 65(5):404–412
Rauschenbach L, Santos AN, Dinger TF et al (2021) Predictive value of intraoperative neuromonitoring in brainstem cavernous malformation surgery. World Neurosurg 156:e359–e373
Romstöck J, Strauss C, Fahlbusch R (2000) Continuous electromyography monitoring of motor cranial nerves during cerebellopontine angle surgery. J Neurosurg 93(4):586–593
Sarnthein J, Hejrati N, Neidert MC, Huber AM, Krayenbühl N (2013) Facial nerve motor evoked potentials during skull base surgery to monitor facial nerve function using the threshold-level method. Neurosurg Focus. https://doi.org/10.3171/2012.12.FOCUS12386
Schmitt WR, Daube JR, Carlson ML, Mandrekar JN, Beatty CW, Neff BA, Driscoll CL, Link MJ (2013) Use of supramaximal stimulation to predict facial nerve outcomes following vestibular schwannoma microsurgery: results from a decade of experience - Clinical article. J Neurosurg 118(1):206–212
Seidel K, Biner MS, Zubak I, Rychen J, Beck J, Raabe A (2020) Continuous dynamic mapping to avoid accidental injury of the facial nerve during surgery for large vestibular schwannomas. Neurosurg Rev 43(1):241–248
Song H, Ma C, Xu D, Yu M, Feng J, Sun L (2018) Prognostic value of transcranial facial nerve motor-evoked potentials in predicting facial nerve function following cerebellopontine angle tumorectomy. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000012576
Springborg JB, Poulsgaard L, Thomsen J (2008) Nonvestibular schwannoma tumors in the cerebellopontine angle: a structured approach and management guidelines. Skull Base 18(4):217–228
Starnoni D, Giammattei L, Cossu G et al Surgical management for large vestibular schwannomas: a systematic review, meta-analysis, and consensus statement on behalf of the EANS skull base section. https://doi.org/10.1007/s00701-020-04491-7/Published
Tatagiba M, Roser F, Schuhmann MU, Ebner FH (2014) Vestibular schwannoma surgery via the retrosigmoid transmeatal approach. Acta Neurochir 156(2):421–425 discussion 425
Tawfik KO, Walters ZA, Kohlberg GD, Lipschitz N, Breen JT, O’Neal K, Zuccarello M, Samy RN (2019) Impact of motor-evoked potential monitoring on facial nerve outcomes after vestibular schwannoma resection. Ann Otol Rhinol Laryngol. https://doi.org/10.1177/0003489418803969
Torihashi K, Sora S, Sato H, Kohno M (2018) The method for placement of an intraoperative continuous facial nerve stimulating electrode in acoustic neuroma surgery: Technical note. Neurol Med Chir (Tokyo) 58(11):477–480
Code availability
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
KM and GN contributed to the conception and design of the study, the acquisition and analysis of data, and the drafting of the manuscript. MR contributed to the acquisition and analysis of data. ML, LO, EW, MG, and SW contributed analysis of data and critical reviewed the manuscript. MT contributed to the conception and design of the study, the acquisition of data, and critical reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the local ethics committee of the Eberhard Karls University Tuebingen.
Consent to participate and consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Machetanz, K., Roegele, M., Liebsch, M. et al. Predictive value of facial motor–evoked potential and electromyography for facial motor function in vestibular schwannoma surgery. Acta Neurochir 166, 23 (2024). https://doi.org/10.1007/s00701-024-05927-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05927-0