Abstract
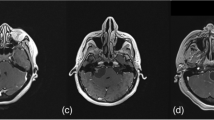
Gamma knife radiosurgery (GKRS) has been accepted as a safe and effective treatment for vestibular schwannoma (VS). However, during follow-up, tumor expansion induced by irradiation can occur, and diagnosis of failure in radiosurgery for VS is still controversial. Tumor expansion with cystic enlargement causes some confusion regarding whether further treatment should be performed. We analyzed more than 10 years of clinical findings and imaging of patients with VS with cystic enlargement after GKRS. A 49-year-old male with hearing impairment was treated with GKRS (12 Gy; isodose, 50%) for a left VS with a preoperative tumor volume of 0.8 cc. The tumor size increased with cystic changes from the third year after GKRS, reaching a volume of 10.8 cc at 5 years after GKRS. At the 6th year of follow-up, the tumor volume started to decrease, up to 0.3 cc by the 14th year of follow-up. A 52-year-old female with hearing impairment and left facial numbness was treated with GKRS for a left VS (13 Gy; isodose, 50%). The preoperative tumor volume was 6.3 cc, which started to increase with cystic enlargement from the first year after GKRS, and reaching 18.2 cc by 5 years after GKRS. The tumor maintained a cystic pattern with slight changes in size, but no other neurologic symptoms developed during the follow-up period. After 6 years of GKRS, tumor regression was observed, eventually reaching a volume of 3.2 cc by the 13th year of follow-up. In both cases, persistent cystic enlargement in VS was observed at 5 years after GKRS, after which the tumors began to stabilize. After more than 10 years of GKRS, the tumor volume was less than that before GKRS. Enlargement with large cystic formation in the first 3–5 years after GKRS has been considered as treatment failure. However, our cases show that further treatment for cystic enlargement should be deferred for at least 10 years, especially in patients without neurological deterioration, as inadequate surgery can be prevented within that period.


Similar content being viewed by others

Abbreviations
- GKRS:
-
Gamma Knife radiosurgery
- VS:
-
Vestibular schwannoma
- CPA:
-
Cerebellopontine angle
- SRS:
-
Stereotactic radiosurgery
- MRI:
-
Magnetic resonance imaging
- IAC:
-
Internal acoustic canal
- PTA:
-
Pure-tone audiometry
- SDT:
-
Speech discrimination test
References
Apicella G, Paolini M, Deantonio L, Masini L, Krengli M (2016) Radiotherapy for vestibular schwannoma: review of recent literature results. Rep Pract Oncol Radiother 21:399–406. https://doi.org/10.1016/j.rpor.2016.02.002
Breshears JD, Chang J, Molinaro AM, Sneed PK, McDermott MW, Tward A, Theodosopoulos PV (2019) Temporal dynamics of pseudoprogression after gamma knife radiosurgery for vestibular schwannomas-a retrospective volumetric study. Neurosurgery 84:123–131. https://doi.org/10.1093/neuros/nyy019
Carlson ML, Habermann EB, Wagie AE, Driscoll CL, Van Gompel JJ, Jacob JT, Link MJ (2015) The changing landscape of vestibular schwannoma management in the united states–a shift toward conservatism. Otolaryngol Head Neck Surg 153:440–446. https://doi.org/10.1177/0194599815590105
De Sanctis P, Green S, Germano I (2019) Communicating hydrocephalus after radiosurgery for vestibular schwannomas: does technique matter? A systematic review and meta-analysis. J Neurooncol 145:365–373. https://doi.org/10.1007/s11060-019-03305-w
Delsanti C, Roche PH, Thomassin JM, Regis J (2008) Morphological changes of vestibular schwannomas after radiosurgical treatment: pitfalls and diagnosis of failure. Prog Neurol Surg 21:93–97. https://doi.org/10.1159/000156712
Goldbrunner R, Weller M, Regis J, Lund-Johansen M, Stavrinou P, Reuss D, Evans DG, Lefranc F, Sallabanda K, Falini A, Axon P, Sterkers O, Fariselli L, Wick W, Tonn JC (2020) EANO guideline on the diagnosis and treatment of vestibular schwannoma. Neuro Oncol 22:31–45. https://doi.org/10.1093/neuonc/noz153
Hayhurst C, Zadeh G (2012) Tumor pseudoprogression following radiosurgery for vestibular schwannoma. Neuro Oncol 14:87–92. https://doi.org/10.1093/neuonc/nor171
Kim JH, Jung HH, Chang JH, Chang JW, Park YG, Chang WS (2017) Predictive factors of unfavorable events after gamma knife radiosurgery for vestibular schwannoma. World Neurosurg 107:175–184. https://doi.org/10.1016/j.wneu.2017.07.139
Kshettry VR, Hsieh JK, Ostrom QT, Kruchko C, Barnholtz-Sloan JS (2015) Incidence of vestibular schwannomas in the United States. J Neurooncol 124:223–228. https://doi.org/10.1007/s11060-015-1827-9
Lau T, Olivera R, Miller T Jr, Downes K, Danner C, van Loveren HR, Agazzi S (2012) Paradoxical trends in the management of vestibular schwannoma in the United States. J Neurosurg 117:514–519. https://doi.org/10.3171/2012.5.JNS111858
Li LF, Yu CP, Tsang AC, Taw BB, Lui WM (2020) Near-complete regression 19 years after Gamma Knife radiosurgery of vestibular schwannoma with massive pseudoprogression: case report. J Neurosurg 134:1455–1458. https://doi.org/10.3171/2020.3.JNS20389
Linkov F, Valappil B, McAfee J, Goughnour SL, Hildrew DM, McCall AA, Linkov I, Hirsch B, Snyderman C (2017) Development of an evidence-based decision pathway for vestibular schwannoma treatment options. Am J Otolaryngol 38:57–64. https://doi.org/10.1016/j.amjoto.2016.09.019
Mackeith SA, Kerr RS, Milford CA (2013) Trends in acoustic neuroma management: a 20-year review of the oxford skull base clinic. J Neurol Surg B Skull Base 74:194–200. https://doi.org/10.1055/s-0033-1342919
Malone J, Tiberi D, Sinclair J, Gaviolli E, Malone S (2020) Delayed pseudoprogression of a vestibular schwannoma postradiosurgery. Radiol Case Rep 15:749–752. https://doi.org/10.1016/j.radcr.2020.03.001
Marinelli JP, Lohse CM, Carlson ML (2018) Incidence of vestibular schwannoma over the past half-century: a population-based study of Olmsted County, Minnesota. Otolaryngol Head Neck Surg 159:717–723. https://doi.org/10.1177/0194599818770629
Nagano O, Higuchi Y, Serizawa T, Ono J, Matsuda S, Yamakami I, Saeki N (2008) Transient expansion of vestibular schwannoma following stereotactic radiosurgery. J Neurosurg 109:811–816. https://doi.org/10.3171/JNS/2008/109/11/0811
Nasi D, Zunarelli E, Puzzolante A, Moriconi E, Pavesi G (2020) Early life-threating enlargement of a vestibular schwannoma after gamma knife radiosurgery. Acta Neurochir (Wien) 162:1977–1982. https://doi.org/10.1007/s00701-020-04434-2
Patel MA, Marciscano AE, Hu C, Jusue-Torres I, Garg R, Rashid A, Francis HW, Lim M, Redmond KJ, Rigamonti D, Kleinberg LR (2017) Long-term treatment response and patient outcomes for vestibular schwannoma patients treated with hypofractionated stereotactic radiotherapy. Front Oncol 7:200. https://doi.org/10.3389/fonc.2017.00200
Pollock BE (2006) Management of vestibular schwannomas that enlarge after stereotactic radiosurgery: treatment recommendations based on a 15 year experience. Neurosurgery 58:241–248. https://doi.org/10.1227/01.NEU.0000194833.66593.8B. (discussion 241-248)
Regis J, Delsanti C, Roche PH (2017) Editorial: Vestibular schwannoma radiosurgery: progression or pseudoprogression? J Neurosurg 127:374–379. https://doi.org/10.3171/2016.7.JNS161236
Shuto T, Inomori S, Matsunaga S, Fujino H (2008) Microsurgery for vestibular schwannoma after gamma knife radiosurgery. Acta Neurochir (Wien) 150:229–234. https://doi.org/10.1007/s00701-007-1486-5. (discussion 234)
Shuto T, Matsunaga S (2016) Two cases of cystic enlargement of vestibular schwannoma as a late complication following gamma knife surgery. J Clin Neurosci 33:239–241. https://doi.org/10.1016/j.jocn.2016.05.022
Wage J, Mignano J, Wu J (2021) Tufts medical center experience with long-term follow-up of vestibular schwannoma treated with gamma knife stereotactic radiosurgery: novel finding of delayed pseudoprogression. Adv Radiat Oncol 6:100687. https://doi.org/10.1016/j.adro.2021.100687
Yu CP, Cheung JY, Leung S, Ho R (2000) Sequential volume mapping for confirmation of negative growth in vestibular schwannomas treated by gamma knife radiosurgery. J Neurosurg 93(Suppl 3):82–89. https://doi.org/10.3171/jns.2000.93.supplement
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Patient consent
The patients and guardians consented to the submission of the case report for publication in the journal.
Informed consent
The need for informed consent was waived owing to the retrospective nature of this study.
Conflict of interest
The authors declare no commercial or financial relationships that could be construed as potential conflicts of interest regarding the preparation or publication of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, TK., Kim, YJ., Jung, TY. et al. From the perspective of pseudo-progression rather than treatment failure, how long should we wait before considering treatment failure if large cystic enlargement occurs after Gamma Knife radiosurgery for vestibular schwannoma?: insight into pseudoprogression based on two case reports. Acta Neurochir 165, 2105–2109 (2023). https://doi.org/10.1007/s00701-023-05684-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05684-6