Abstract
Purpose
Large (> 3 cm) vestibular schwannomas pose complexity in surgical management because of narrow working corridors and proximity to the cranial nerves, brainstem, and inner ear structures. With current vestibular schwannoma classifications limited in information regarding cerebellopontine edema, our retrospective series examined this radiographic feature relative to clinical outcomes and its possible role in preoperative scoring.
Methods
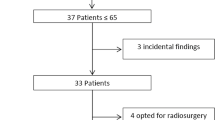
Of 230 patients who underwent surgical resection of vestibular schwannoma (2014–2020), we identified 107 patients with Koos grades 3 or 4 tumors for radiographic assessment of edema in the middle cerebellar peduncle (MCP), brainstem, or both. Radiographic images were graded and patients grouped into Koos grades 3 or 4 or our proposed grade 5 with edema. Tumor volumes, radiographic features, clinical presentations, and clinical outcomes were evaluated.
Results
The 107 patients included 22 patients with grade 3 tumors, 39 with grade 4, and 46 with grade 5. No statistical differences were noted among groups for demographic data or complication rates. Unlike grades 3 and 4 patients, grade 5 patients presented with worse hearing (p < 0.001), larger tumors (p < 0.001), lower rates of gross total resection (GTR), longer hospital stays, and higher rates of balance dysfunction.
Conclusion
With edema detected in 43% of this cohort, special considerations are warranted for grade 5 vestibular schwannomas given the preoperative findings of worse hearing, lower GTR rates, longer hospital stays, and 96% who pursued postoperative balance therapy. We propose that grade 5 with edema offers a more nuanced interpretation of a radiographic feature that holds relevance to treatment selection and patient outcomes.



Similar content being viewed by others
Data Availability
Data available on request.
Change history
30 June 2023
The ORCID of A. Samy Youssef is corrected.
Abbreviations
- AAO-HNS:
-
American Academy of Otolaryngology—Head and Neck Surgery
- ADC:
-
Apparent diffusion coefficient
- MCP:
-
Middle cerebellar peduncle
- HB:
-
House-Brackmann
- LOS:
-
Length of stay
- MRI:
-
Magnetic resonance imaging
- ROI:
-
Region of interest
- 3D:
-
Three-dimensional
References
Atchley TJ, Erickson N, Chagoya G, Fort M, Walters BC, McGrew B, Fisher WS 3rd (2022) Hannover classification of vestibular schwannomas: a reliability study. World Neurosurg 158:e179–e183
Chen X, Gao XL, Chai Y, Shi MM, Zhang JN, Yue SY (2020) Use of a compact high-definition two-dimensional exoscope in surgical treatment of large vestibular schwannoma. Chin Med J (Engl) 133(11):1292–1297
Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). American Academy of Otolaryngology-Head and Neck Surgery Foundation (1995) Otolaryngol Head Neck Surg 113(3):179–180
Daming C, Yiwen S, Bin Z, Yajun X, Jia Y, Rui S et al (2014) Large vestibular schwannoma resection through the suboccipital retrosigmoid keyhole approach. J Craniofac Surg 25(2):463–468
d’Avella D, Mazzoni A, Zanoletti E, Martini A (2013) Microsurgical endoscopy-assisted presigmoid retrolabyrinthine approach as a minimally invasive surgical option for the treatment of medium to large vestibular schwannoma. Acta Neurochir (Wien) 155:671–673
Erickson NJ, Schmalz PGR, Agee BS, Fort M, Walters BC, McGrew BM, Fisher WS (2019) Koos classification of vestibular schwannomas: a reliability study. Neurosurgery 85(3):409–414
Friedmann DR, Grobelny B, Golfinos JG, Roland JT Jr (2015) Nonschwannoma tumors of the cerebellopontine angle. Otolaryngol Clin North Am 48(3):461–475
Goldbrunner R, Weller M, Regis J, Lund-Johansen M, Stavrinou P, Reuss D et al (2020) EANO guideline on the diagnosis and treatment of vestibular schwannoma. Neuro Oncol 22(1):31–45
Giordano M, Gerganov V, Metwali H, Gallieni M, Samii M, Samii A (2020) Imaging features and classification of peritumoral edema in vestibular schwannoma. Neuroradiol J 33(2):169–173
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93(2):146–1477
Jacob JT, Carlson ML, Driscoll CL, Link MJ (2016) Volumetric analysis of tumor control following subtotal and near-total resection of vestibular schwannoma. Laryngoscope 126(8):1877–1882
Jung S, Kim S, Kim H et al (1998) Prediction of facial nerve displacement in extralarge vestibular schwannoma. Acta Neurochir (Wien) 140:1143–1145
Kiyofuji S, Neff BA, Carlson ML, Driscoll CLW, Link MJ (2021) Large and small vestibular schwannomas: same, yet different tumors. Acta Neurochir (Wien) 163:2199–2207
Klironomos G, Dehdashti AR (2019) Surgical strategy in large vestibular schwannoma. J Neurol Surg Part B Skull Base 80:S272–S273
Koos WT, Day JD, Matula C, Levy DI (1998) Neurotopographic considerations in the microsurgical treatment of small acoustic neurinomas. J Neurosurg 88:506–512
Kunigelis KE, Hosokawa P, Arnone G, Raban D, Starr A, Gurau A et al (2020) The predictive value of preoperative apparent diffusion coefficient (ADC) for facial nerve outcomes after vestibular schwannoma resection: clinical study. Acta Neurochir (Wien) 162(8):1995–2005
Landry AP, Yang K, Wang JZ, Gao AF, Zadeh G (2022) Outcomes in vestibular schwannoma treated with primary microsurgery: Clinical landscape. J Clin Neurosci 96:138–146
Li D, Tsimpas A, Germanwala AV (2015) Analysis of vestibular schwannoma size: A literature review on consistency with measurement techniques. Clin Neurol Neurosurg 138:72–77
Macielak RJ, Driscoll CLW, Link MJ, Haynes DS, Lohse CM, Carlson ML (2020) Vestibular schwannoma practice patterns: an international cross-specialty survey. Otol Neurotol 41(10):e1304–e1313
Matthies C, Samii M (1997) Management of 1000 Vestibular schwannomas (acoustic neuromas): clinical presentation. Neurosurgery 40:1–10
Samii M, Giordano M, Metwali H, Almarzooq O, Samii A, Gerganov VM (2015) Prognostic significance of peritumoral edema in patients with vestibular schwannomas. Neurosurgery 77(1):81–86
Satyarthee GD (2017) Predicting shape, location, and course of facial nerve in relation to large vestibular schwannoma on diffusion tensor imaging with intraoperative correlation: important surgical adjunct. World Neurosurg 105:1002
Song G, Liu D, Wu X, Wang X, Zhou Y, Li M et al (2021) Outcomes after semisitting and lateral positioning in large vestibular schwannoma surgery: A single-center comparison. Clin Neurol Neurosurg 207:106768
Troude L, Boucekine M, Montava M, Lavieille JP, Régis JM, Roche PH (2019) Predictive factors of early postoperative and long-term facial nerve function after large vestibular schwannoma surgery. World Neurosurg 127:e599–e608
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31(3):1116–1128
Zumofen DW, Guffi T, Epple C, Westermann B, Krähenbühl AK, Zabka S et al (2018) Intended near-total removal of Koos Grade IV vestibular schwannomas: reconsidering the treatment paradigm. Neurosurgery 82(2):202–210
Acknowledgements
Mary Kemper provided medical editing of this paper.
Author information
Authors and Affiliations
Contributions
Study supervision: A. Samy Youssef.
Concept and design: Timothy Ung, A. Samy Youssef
Acquisition of data: Timothy Ung, Lindsey Freeman, Lisa Hirt, Michael Kortz, Katherine Belanger, Eliza Baird Daniel, Ashesh Thaker, John Thompson, A. Samy Youssef.
Analysis and interpretation of data: Timothy Ung, Lindsey Freeman, Lisa Hirt, Michael Kortz, Katherine Belanger, Eliza Baird Daniel, Patrick Hosokawa, Ashesh Thaker, John Thompson, A. Samy Youssef.
Drafting the paper: all authors.
Review of submitted version: Timothy Ung, Lindsey Freeman, Lisa Hirt, Michael Kortz, Katherine Belanger, Eliza Baird Daniel, Patrick Hosokawa, Ashesh Thaker, John Thompson, A. Samy Youssef.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the (place name of institution and/or national research committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ung, T.H., Freeman, L., Hirt, L. et al. Surgical outcomes in large vestibular schwannomas: should cerebellopontine edema be considered in the grading systems?. Acta Neurochir 165, 1749–1755 (2023). https://doi.org/10.1007/s00701-023-05627-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05627-1