Abstract
Purpose
The dynamic nature of intraneural ganglion cysts, including spontaneous expansion and regression, has been described. However, whether these cysts can regress completely in the absence of surgical management has important therapeutic implications. Therefore, we aim to review the literature for cyst regression without surgical intervention.
Methods
We reviewed our database of 970 intraneural ganglion cysts in the literature to search for evidence of complete regression based on strict radiologic confirmation, either spontaneously, or after percutaneous cyst aspiration or steroid injection.
Results
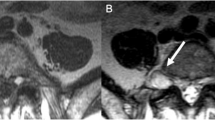
We did not find any examples of complete regression without surgical treatment that met inclusion criteria. Spontaneous regression was reported in four cases; however, only two cases had follow-up imaging, both of which demonstrated residual cysts. Nineteen cases of percutaneous intervention were found in the literature, 13 of which reported clinical improvement following aspiration/steroid injection; however, only seven cases had available imaging. Only two cases reported complete resolution of cyst on MR imaging at follow-up, but reinterpretation found residual intraneural cyst in both cases.
Conclusion
We believe that pathology (structural abnormalities and/or increased joint fluid) always exists at the joint origin of intraneural ganglion cysts which persist even with regression of the cyst. The persistence of a capsular abnormality or defect can lead to recurrence of the cyst in the future, and while imaging may show dramatic decreases in cyst size, truly focused assessment of images will show a tiny focus of persistent intraneural cyst at the joint origin. Thus, expectant management or percutaneous intervention may lead to regression, but not complete resolution, of intraneural ganglion cysts.





Similar content being viewed by others
References
Blitz NM, Amrami KK, Spinner RJ (2009) Magnetic resonance imaging of a deep peroneal intraneural ganglion cyst originating from the second metatarsophalangeal joint: a pattern of propagation supporting the unified articular (synovial) theory for the formation of intraneural ganglia. J Foot Ankle Surg 48:80–84
Boody BS, Savage JW (2016) Evaluation and treatment of lumbar facet cysts. J Am Acad Orthop Surg 24:829–842. https://doi.org/10.5435/JAAOS-D-14-00461
Botchu R, Esler CN, Lloyd DM, Rennie WJ (2013) Ganglia arising from the transverse acetabular ligament: a report of two cases. J Orthop Surg (Hong Kong) 21:380–382. https://doi.org/10.1177/230949901302100324
de Bruijn K, Franssen G, van Ginhoven T (2013) A stepwise approach to ‘groin pain’: a common symptom, an uncommon cause. BMJ Case Rep 2013:bcr2013010466. https://doi.org/10.1136/bcr-2013-010466
Desy NM, Wang H, Elshiekh MA, Tanaka S, Choi TW, Howe BM, Spinner RJ (2016) Intraneural ganglion cysts: a systematic review and reinterpretation of the world’s literature. J Neurosurg 125:615–630. https://doi.org/10.3171/2015.9.JNS141368
Eguchi K, Shirai S, Iwata I, Matsushima M, Yabe I (2020) A case of tibial nerve palsy due to intraneural ganglion cysts. Rinsho Shinkeigaku 60:549–553. https://doi.org/10.5692/clinicalneurol.60.cn-001422
Hartman P, LeGay D (2007) Disappearing foot drop: a peroneal nerve ganglion. Dalhous Med J34(3):14–16
Head L, Gencarelli JR, Allen M, Boyd KU (2015) Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg Am 40(546–553):e548. https://doi.org/10.1016/j.jhsa.2014.12.014
Hersekli MA, Akpinar S, Demirors H, Ozkoc G, Ozalay M, Cesur N, Uysal M, Tandogan RN (2004) Synovial cysts of proximal tibiofibular joint causing peroneal nerve palsy: report of three cases and review of the literature. Arch Orthop Trauma Surg 124:711–714. https://doi.org/10.1007/s00402-004-0717-y
Jitpun E, Hidalgo J, Link MJ, Amrami KK, Spinner RJ (2019) Letter to the Editor regarding “Spontaneous regression of a hypoglossal neurinoma: case report and review of the literature”. World Neurosurg 130:578–579. https://doi.org/10.1016/j.wneu.2019.06.033
Jitpun E, Howe BMM, Amrami KK, Trousdale RT, Spinner RJ (2019) Obturator intraneural ganglion cysts: joint connected and underdiagnosed. World Neurosurg 126:e259–e269. https://doi.org/10.1016/j.wneu.2019.02.029
Jose J, Fourzali R, Lesniak B, Kaplan L (2011) Ultrasound-guided aspiration of symptomatic intraneural ganglion cyst within the tibial nerve. Skeletal Radiol 40:1473–1478. https://doi.org/10.1007/s00256-011-1209-0
Kim SW, Yoon YC, Sung DH (2022) Intraneural ganglion cysts originating from the hip joint: a single center experience. Muscle Nerve. https://doi.org/10.1002/mus.27535
Laumonerie P, Lapegue F, Reina N, Tibbo M, Rongieres M, Faruch M, Mansat P (2018) Degenerative subtalar joints complicated by medial plantar intraneural cysts: cutting the cystic articular branch prevents recurrence. Bone Joint J 100-B:183–189. https://doi.org/10.1302/0301-620X.100B2.BJJ-2017-0990.R1
Leafblad ND, Wilson TJ, Amrami KK, Turner NS, Spinner RJ (2019) Cystic adventitial disease of the tibial vein arising from the subtalar joint: a case report. J Foot Ankle Surg 58:377–380. https://doi.org/10.1053/j.jfas.2018.08.044
Li P, Lou D, Lu H (2018) The cubital tunnel syndrome caused by intraneural ganglion cyst of the ulnar nerve at the elbow: a case report. BMC Neurol 18:1–4
Liang T, Panu A, Crowther S, Low G, Lambert R (2013) Ultrasound-guided aspiration and injection of an intraneural ganglion cyst of the common peroneal nerve. HSS J 9:270–274. https://doi.org/10.1007/s11420-013-9345-9
Miomo H, Shibata K, Kina M, Tomari S, Tomoshige M (1992) Peroneal nerve paralysis due to intraneural ganglion: a case report. Orthop Traumatol 41:180–183
Mirzatolooei F, Tabrizi A, Kazemi-Shishavan SAM (2019) A case of intraneural ganglion cyst of the peroneal nerve: a rapid recovery after incision of cyst. J Res Clin Med 7:129–132
Nagano MUMSN, Kurihara A (1995) A case of tarsal tunnel syndrome caused by intraneural ganglion. J Jpn Soc Surg Foot 16:64–65
Park SH, Do HK, Jo GY (2019) Compressive peroneal neuropathy by an intraneural ganglion cyst combined with L5 radiculopathy: a case report. Med (Baltimore) 98:e17865. https://doi.org/10.1097/MD.0000000000017865
Santander XA, Cotua CE, Saldana C (2017) Spontaneous regression of a hypoglossal neurinoma: case report and review of the literature. World Neurosurg 105:1033 e1037-1033 e1039. https://doi.org/10.1016/j.wneu.2017.06.004
Santander XA, Cotua CE, Saldana C, Brea AB (2019) In reply to the letter to the editor regarding “Spontaneous regression of a hypoglossal neurinoma: case report and review of the literature”. World Neurosurg 130:580–581. https://doi.org/10.1016/j.wneu.2019.07.081
Shahid KR, Hebert-Blouin MN, Amrami KK, Spinner RJ (2011) Extraneural rupture of intraneural ganglion cysts. J Surg Orthop Adv 20:136–141
Spinner RJ, Amrami KK, Wolanskyj AP, Desy NM, Wang H, Benarroch EE, Skinner JA, Rock MG, Scheithauer BW (2007) Dynamic phases of peroneal and tibial intraneural ganglia formation: a new dimension added to the unifying articular theory. J Neurosurg 107:296–307. https://doi.org/10.3171/JNS-07/08/0296
Spinner RJ, Atkinson JL, Tiel RL (2003) Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory J Neurosurg 99:330–343. https://doi.org/10.3171/jns.2003.99.2.0330
Spinner RJ, Desy NM, Amrami KK (2016) The unifying articular (synovial) origin for intraneural ganglion cysts: moving beyond a theory. J Hand Surg Am 41:e223-224. https://doi.org/10.1016/j.jhsa.2016.04.004
Spinner RJ, Hebert-Blouin MN, Rock MG, Amrami KK (2011) Extreme intraneural ganglion cysts. J Neurosurg 114:217–224. https://doi.org/10.3171/2010.4.JNS091969
Spinner RJ, Mikami Y, Desy NM, Amrami KK, Berger RA (2018) Superficial radial intraneural ganglion cysts at the wrist. Acta Neurochir 160:2479–2484
Spinner RJ, Wang H, Howe BM, Colbert SH, Amrami KK (2012) Deep ulnar intraneural ganglia in the palm. Acta Neurochir (Wien) 154:1755–1763. https://doi.org/10.1007/s00701-012-1422-1
Squires JH, Emery KH, Johnson N, Sorger J (2014) Tibial nerve intraneural ganglion cyst in a 10-year-old boy. Pediatr Radiol 44:488–490. https://doi.org/10.1007/s00247-013-2814-y
Vidoni A, McLoughlin E, James SL, Botchu R (2020) Intra-neural ganglion cyst of the lateral dorsal cutaneous nerve: an uncommon cause of lateral ankle pain. J Ultrasound 23:81–86. https://doi.org/10.1007/s40477-019-00387-0
Visser LH (2006) High-resolution sonography of the common peroneal nerve: detection of intraneural ganglia. Neurol 67:1473–1475. https://doi.org/10.1212/01.wnl.0000240070.98910.bc
Waldschmidt U, Slongo T (2010) An unusual cause of paralysis of the peroneal nerve-a case report. J Pediatr Surg 45:259–261. https://doi.org/10.1016/j.jpedsurg.2009.09.039
Weyns F, Bringmans T, Vandevenne J, Daenekindt T, Van Goethem A, Wuyts J, Vanormelingen L, Vandersteen M (2012) Peripheral neuropathy caused by joint-related cysts: a review of 17 cases. Acta Neurochir (Wien) 154:1741–1753. https://doi.org/10.1007/s00701-012-1444-8
Wilson TJ, Hebert-Blouin MN, Murthy NS, Amrami KK, Spinner RJ (2017) Recognition of peroneal intraneural ganglia in an historical cohort with “negative” MRIs. Acta Neurochir (Wien) 159:925–930. https://doi.org/10.1007/s00701-017-3130-3
Wilson TJ, Hebert-Blouin MN, Murthy NS, Garcia JJ, Amrami KK, Spinner RJ (2017) The nearly invisible intraneural cyst: a new and emerging part of the spectrum. Neurosurg Focus 42:E10. https://doi.org/10.3171/2016.12.FOCUS16439
Wilson TJ, Mauermann ML, Rock MG, Spinner RJ (2018) Outcomes following surgery for peroneal intraneural ganglion cysts. Muscle Nerve 57:989–993. https://doi.org/10.1002/mus.26062
Yukata K, Arai K, Yoshizumi Y, Tamano K, Imada K, Nakaima N (2005) Obturator neuropathy caused by an acetabular labral cyst: MRI findings. Am J Roentgenol 184:S112–S114
Author information
Authors and Affiliations
Contributions
Conceptualization: Nicole M. De La Pena, Thomas J. Wilson, Kimberly K. Amrami, and Robert J. Spinner; Data curation: Karina A. Lenartowicz, Nicholas M. Desy, Alexandre S. Wolf, and Kimberly K. Amrami; Formal analysis: Karina A. Lenartowicz, Nikhil K. Murthy, and Robert J. Spinner; Investigation: Nikhil K. Murthy and Alexandre S. Wolf; Methodology: Karina A. Lenartowicz, and Nicole M. De La Pena; Resources: Nicholas M. Desy; Software: Karina A. Lenartowicz, Nicholas M. Desy, and Alexandre S. Wolf; Supervision: Kimberly K. Amrami and Robert J. Spinner; Writing—original draft: Nikhil K. Murthy and Robert J. Spinner; Writing—review and editing: Karina A. Lenartowicz, Thomas J. Wilson, and Robert J. Spinner.
Corresponding author
Ethics declarations
Ethics approval
The manuscript does not contain clinical studies or patient data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Peripheral Nerves
Rights and permissions
About this article
Cite this article
Lenartowicz, K.A., Murthy, N.K., Desy, N.M. et al. Does complete regression of intraneural ganglion cysts occur without surgery?. Acta Neurochir 164, 2689–2698 (2022). https://doi.org/10.1007/s00701-022-05311-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05311-w