Abstract
Background
Intracranial aneurysm (IA) rupture in pediatric patients is a rare but fatal condition. Although risk factors for aneurysm rupture in adults have been well documented, they remain unknown in pediatric patients.
Methods
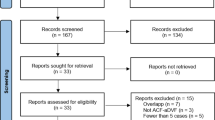
Data for 94 pediatric patients with IAs were retrospectively analyzed. The patients were divided into ruptured and unruptured groups. Risk factors for aneurysm rupture were analyzed through univariable and multiple logistic regression analyses. Typical patients with risk factors were described.
Results
Univariable analyses showed that the unruptured group had significantly higher percentages of giant aneurysms (43.2% vs 12.3%, P = 0.002), wide-neck aneurysms (67.6% vs 29.8%, P = 0.001), and aneurysms located in the internal carotid artery (40.5% vs 3.5%, P < 0.001), while the ruptured group had significantly higher percentages of patients younger than 5 years old (28.1% vs 5.4%, P = 0.013) and aneurysms located in the anterior cerebral artery (24.6% vs 5.4%, P = 0.032), posterior cerebral artery (14.0% vs 0%, P = 0.045), and distal arterial region (DAR) (46.8% vs 27.0%, P < 0.001). Multiple logistic regression analysis confirmed that age 0–5 years (OR = 6.844, P = 0.042) and IAs located in the DAR (OR = 4.162, P = 0.029) were independently related to an increased risk of rupture. Wide-necked aneurysms (OR = 0.235, P = 0.047) were independently associated with a lower risk of rupture.
Conclusions
Among pediatric patients, age younger than 5 years and lesions located in the DAR are independent risk factors for IA rupture, while an IA with a wide neck acts as a protective factor.

Similar content being viewed by others
Abbreviations
- IA:
-
Intracranial aneurysm
- DAR:
-
Arterial region
- SAH:
-
Subarachnoid hemorrhage
- ICH:
-
Intracerebral hemorrhage
- IRB:
-
Institutional review board
- GCS:
-
Glasgow Coma Scale
- CT:
-
Computed tomography
- CTA:
-
Computed tomographic angiography
- DSA:
-
Digital subtraction angiography
- MCA:
-
Middle cerebral artery
- ACA:
-
Anterior cerebral artery
- PCA:
-
Posterior cerebral artery
- SD:
-
Standard deviation
- CI:
-
Confidence interval
- ICA:
-
Internal carotid artery
- AVM:
-
Arteriovenous malformations
- ICP:
-
Intracranial pressure
- AR:
-
Aspect ratio
References
Backeljauw B, Holland SK, Altaye M, Loepke AW (2015) Cognition and brain structure following early childhood surgery with anesthesia. Pediatrics 136:e1-12. https://doi.org/10.1542/peds.2014-3526
Bauman KE, Ennett ST, Foshee VA, Pemberton M, King TS, Koch GG (2002) Influence of a family program on adolescent smoking and drinking prevalence. Prev Sci 3:35–42. https://doi.org/10.1023/a:1014619325968
Beez T, Steiger HJ, Hanggi D (2016) Evolution of management of intracranial aneurysms in children: a systematic review of the modern literature. J Child Neurol 31:773–783. https://doi.org/10.1177/0883073815609153
Can A, Castro VM, Ozdemir YH, Dagen S, Dligach D, Finan S, Yu S, Gainer V, Shadick NA, Savova G, Murphy S, Cai T, Weiss ST, Du R (2018) Alcohol consumption and aneurysmal subarachnoid hemorrhage. Transl Stroke Res 9:13–19. https://doi.org/10.1007/s12975-017-0557-z
Chen R, Zhang S, Guo R, Ma L, You C (2018) Pediatric intracranial distal arterial aneurysms: report of 35 cases. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-018-3574-0
Chen R, Zhang S, You C, Guo R, Ma L (2018) Pediatric intracranial aneurysms: changes from previous studies. Childs Nerv Syst. https://doi.org/10.1007/s00381-018-3818-6
Chen R, Zhang S, You C, Guo R, Ma L (2018) Pediatric intracranial aneurysms: changes from previous studies. Childs Nerv Syst 34:1697–1704. https://doi.org/10.1007/s00381-018-3818-6
Chowdhury T, Cappellani RB, Sandu N, Schaller B, Daya J (2013) Perioperative variables contributing to the rupture of intracranial aneurysm: an update. ScientificWorldJournal 2013:396404. https://doi.org/10.1155/2013/396404
Clarke M (2008) Systematic review of reviews of risk factors for intracranial aneurysms. Neuroradiology 50:653–664. https://doi.org/10.1007/s00234-008-0411-9
Eguchi T, Kurokawa S, Hashimoto H, Hoshida T, Sakaki T (1995) Experimental study on hypertensive crises in epileptic seizures–changes in pial artery diameter, intracranial pressure and regional cerebral blood flow. No To Shinkei 47:1143–1148
Falkner B (2010) Hypertension in children and adolescents: epidemiology and natural history. Pediatr Nephrol 25:1219–1224. https://doi.org/10.1007/s00467-009-1200-3
Flemming KD, Wiebers DO, Brown RD Jr, Link MJ, Nakatomi H, Huston J 3rd, McClelland R, Christianson TJ (2004) Prospective risk of hemorrhage in patients with vertebrobasilar nonsaccular intracranial aneurysm. J Neurosurg 101:82–87. https://doi.org/10.3171/jns.2004.101.1.0082
Hetts SW, Narvid J, Sanai N, Lawton MT, Gupta N, Fullerton HJ, Dowd CF, Higashida RT, Halbach VV (2009) Intracranial aneurysms in childhood: 27-year single-institution experience. AJNR Am J Neuroradiol 30:1315–1324. https://doi.org/10.3174/ajnr.A1587
Kapoor BS, Haddad HL, Saddekni S, Lockhart ME (2009) Diagnosis and management of pseudoaneurysms: an update. Curr Probl Diagn Radiol 38:170–188. https://doi.org/10.1067/j.cpradiol.2008.11.001
Kleinloog R, de Mul N, Verweij BH, Post JA, Rinkel GJE, Ruigrok YM (2018) Risk factors for intracranial aneurysm rupture: a systematic review. Neurosurgery 82:431–440. https://doi.org/10.1093/neuros/nyx238
Korja M, Kivisaari R, Rezai Jahromi B, Lehto H (2017) Natural history of ruptured but untreated intracranial aneurysms. Stroke 48:1081–1084. https://doi.org/10.1161/STROKEAHA.116.015933
Koroknay-Pal P, Laakso A, Lehto H, Seppa K, Kivisaari R, Hernesniemi J, Niemela M (2012) Long-term excess mortality in pediatric patients with cerebral aneurysms. Stroke 43:2091–2096. https://doi.org/10.1161/STROKEAHA.112.650077
Lashkarivand A, Sorteberg W, Rosseland LA, Sorteberg A (2020) Survival and outcome in patients with aneurysmal subarachnoid hemorrhage in Glasgow coma score 3–5. Acta Neurochir (Wien) 162:533–544. https://doi.org/10.1007/s00701-019-04190-y
Lindgren AE, Kurki MI, Riihinen A, Koivisto T, Ronkainen A, Rinne J, Hernesniemi J, Eriksson JG, Jaaskelainen JE, von und zuFraunberg M (2014) Hypertension predisposes to the formation of saccular intracranial aneurysms in 467 unruptured and 1053 ruptured patients in Eastern Finland. Ann Med 46:169–176. https://doi.org/10.3109/07853890.2014.883168
Loepke AW, Soriano SG (2008) An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg 106:1681–1707. https://doi.org/10.1213/ane.0b013e318167ad77
Rinkel GJ, Djibuti M, Algra A, van Gijn J (1998) Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke 29:251–256. https://doi.org/10.1161/01.str.29.1.251
Schmidt-Trucksass A, Grathwohl D, Schmid A, Boragk R, Upmeier C, Keul J, Huonker M (1999) Structural, functional, and hemodynamic changes of the common carotid artery with age in male subjects. Arterioscler Thromb Vasc Biol 19:1091–1097. https://doi.org/10.1161/01.atv.19.4.1091
Sena JC, Reynier Y, Alliez B (2003) Unruptured intracranial aneurysm presenting with epiletic seizure. Arq Neuropsiquiatr 61:663–667. https://doi.org/10.1590/s0004-282x2003000400026
Shin HY, Gerritsen ME, Bizios R (2002) Regulation of endothelial cell proliferation and apoptosis by cyclic pressure. Ann Biomed Eng 30:297–304. https://doi.org/10.1114/1.1458595
Slator N, Talibi SS, Mundil N, Thomas A, Lamin S, Walsh R, Rodrigues D, Solanki GA (2019) Paediatric intracranial aneurysms: a British institutional review. Childs Nerv Syst 35:1197–1205. https://doi.org/10.1007/s00381-019-04159-3
Solheim O, Vik A, Gulati S, Eide PK (2008) Rapid and severe rise in static and pulsatile intracranial pressures during a generalized epileptic seizure. Seizure 17:740–743. https://doi.org/10.1016/j.seizure.2008.05.006
Sorteberg A, Dahlberg D (2013) Intracranial non-traumatic aneurysms in children and adolescents. Curr Pediatr Rev 9:343–352. https://doi.org/10.2174/221155281120100005
Strickland BA, Attenello F, Russin JJ (2016) Extracranial to intracranial bypass for the treatment of cerebral aneurysms in the pediatric population. J Clin Neurosci 34:6–10. https://doi.org/10.1016/j.jocn.2016.05.009
Tanaka T, Takei Y, Yamanouchi D (2016) Hyperglycemia suppresses calcium phosphate-induced aneurysm formation through inhibition of macrophage activation. J Am Heart Assoc 5:e003062. https://doi.org/10.1161/JAHA.115.003062
Tsutsumi K, Ueki K, Morita A, Kirino T (2000) Risk of rupture from incidental cerebral aneurysms. J Neurosurg 93:550–553. https://doi.org/10.3171/jns.2000.93.4.0550
van ’t Hof FN, Ruigrok YM, Lee CH, Ripke S, Anderson G, de Andrade M, Baas AF, Blankensteijn JD, Bottinger EP, Bown MJ, Broderick J, Bijlenga P, Carrell DS, Crawford DC, Crosslin DR, Ebeling C, Eriksson JG, Fornage M, Foroud T, von Und Zu Fraunberg M, Friedrich CM, Gaal EI, Gottesman O, Guo DC, Harrison SC, Hernesniemi J, Hofman A, Inoue I, Jaaskelainen JE, Jones GT, Kiemeney LA, Kivisaari R, Ko N, Koskinen S, Kubo M, Kullo IJ, Kuivaniemi H, Kurki MI, Laakso A, Lai D, Leal SM, Lehto H, LeMaire SA, Low SK, Malinowski J, McCarty CA, Milewicz DM, Mosley TH, Nakamura Y, Nakaoka H, Niemela M, Pacheco J, Peissig PL, Pera J, Rasmussen-Torvik L, Ritchie MD, Rivadeneira F, van Rij AM, Santos-Cortez RL, Saratzis A, Slowik A, Takahashi A, Tromp G, Uitterlinden AG, Verma SS, Vermeulen SH, Wang GT, Aneurysm C, Vascular Research Consortium of New Z, Han B, Rinkel GJ, de Bakker PI (2016) Shared genetic risk factors of intracranial, abdominal, and thoracic aneurysms. J Am Heart Assoc 5.https://doi.org/10.1161/JAHA.115.002603
Vlak MH, Rinkel GJ, Greebe P, Algra A (2013) Risk of rupture of an intracranial aneurysm based on patient characteristics: a case-control study. Stroke 44:1256–1259. https://doi.org/10.1161/STROKEAHA.111.000679
Wan A, Jaja BN, Schweizer TA, Macdonald RL, collaboration obotS (2016) Clinical characteristics and outcome of aneurysmal subarachnoid hemorrhage with intracerebral hematoma. J Neurosurg 125:1344–1351. https://doi.org/10.3171/2015.10.JNS151036
Williams LN, Brown RD Jr (2013) Management of unruptured intracranial aneurysms. Neurol Clin Pract 3:99–108. https://doi.org/10.1212/CPJ.0b013e31828d9f6b
Zheng Y, Lu Z, Shen J, Xu F (2020) Intracranial pseudoaneurysms: evaluation and management. Front Neurol 11:582. https://doi.org/10.3389/fneur.2020.00582
Funding
This study was funded by the fellowship of China Postdoctoral Science Foundation (2020M673237), Postdoctoral Science Foundation of West China Hospital (2020HXBH155) Science and Foundation of Department of Science and Technology Sichuan Province (2020YFS0223);
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Informed consent
Informed consent was obtained from the parents or legal guardians of all individual participants included in the study.
Additional information
Comments
Dr Junpeng Ma and colleagues are acknowledged for their study of risk factors for intracranial aneurysm rupture in pediatric patients. They studied 94 aneurysm patients under 18 years of age selected from 5582 patients managed during a 7-year period in West China Hospital. When ruptured aneurysms (n = 57) and unruptured aneurysms (n = 40) were compared, unruptured aneurysms were more often giant in size, wide-necked and located in ICA, while ruptured aneurysms were more often in younger patients, located in ACA, PCA or peripheral arteries. Multiple regression analysis showed that low age and peripheral location were independent predictors of rupture, while wide-neck was independently associated to low risk of rupture. The findings provide valuable information for the management of pediatric subarachnoid hemorrhage patients.
Per Enblad, M.D., Ph.D.
Uppsala Sweden.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Neurosurgery
Rights and permissions
About this article
Cite this article
Chen, R., Zhang, S., Xiao, A. et al. Risk factors for intracranial aneurysm rupture in pediatric patients. Acta Neurochir 164, 1145–1152 (2022). https://doi.org/10.1007/s00701-021-04957-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04957-2