Abstract
Background
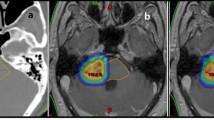
Gamma Knife radiosurgery (GKRS) inverse dose planning is currently far from competing effectively with the quality of dose planning developed by experienced experts. A new inverse planning (IP) method based on « efficient convex optimization algorithms » is proposed, providing high-quality dose plans in real time.
Materials and methods
Eighty-six patients treated by GKRS for vestibular schwannomas (VS) were recruited. The treatment plans created by the first author, who has 27 years of experience and has developed and delivered more than 15,000 dose plans, served as reference. A first set of basic constraints determined by default led the IP for an initial real-time dose plan. Additional constraints were interactively proposed by the planner to take other parameters into account. A second optimized plan was then calculated by the IP. The primary endpoint was the Paddick Conformity Index (PCI). The statistical analysis was planned on a non-inferiority trial design. Coverage, selectivity, and gradient indexes, dose at the organ(s) at risk, and 12 Gy isodose line volume were compared.
Results
After a single run of the IP, the PCI was shown to be non-inferior to that of the “expert.” For the expert and the IP, respectively, the median coverage index was 0.99 and 0.98, the median selectivity index 0.92 and 0.90, the median gradient index 2.95 and 2.84, the median dose at the modiolus of the cochlea 2.83 Gy and 2.86 Gy, the median number of shots 14.31 and 24.13, and the median beam-on time 46.20 min and 26.77 min. In a few specific cases, advanced tools of the IP were used to generate a second run by adding new constraints either globally (for higher selectivity) or locally, in order to increase or decrease these constraints focally.
Conclusion
These preliminary results showed that this new IP method based on « efficient convex optimization algorithms », called IntuitivePlan®, provided high-quality dose plans in real time with excellent coverage, selectivity, and gradient indexes with optimized beam-on time. If the new IP evaluated here is able to compete in real time with the quality of the treatment plans of an expert with extensive radiosurgical experience, this could allow new planners/radiosurgeons with limited or no experience to immediately provide patients with high-quality GKRS for benign and malignant lesions.






Similar content being viewed by others
References
Leksell L (1951) The stereotaxic method and radiosurgery of the brain. Acta Chirurgica Scandinavia 102:316–319
Leksell L (1968) Cerebral radiosurgery. I. Gammathalanotomy in two cases of intractable pain. Acta Chir Scand 134:585–595
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. Journal of neurosurgery 93:219–222
Regis J (2010) Conformity index for radiosurgery. Neurosurgery 67:E521
Wagner TH, Bova FJ, Friedman WA, Buatti JM, Bouchet LG, Meeks SL (2003) A simple and reliable index for scoring rival stereotactic radiosurgery plans. Int J Radiat Oncol Biol Phys 57:1141–1149
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. Journal of neurosurgery 105(Suppl):194–201. https://doi.org/10.3171/sup.2006.105.7.194
Regis J, Tamura M, Guillot C, Yomo S, Muraciolle X, Nagaje M, Arka Y, Porcheron D (2009) Radiosurgery with the world’s first fully robotized Leksell Gamma Knife PerfeXion in clinical use: a 200-patient prospective, randomized, controlled comparison with the Gamma Knife 4C. Neurosurgery 64:346–355 discussion 355-346
Levivier M, Carrillo RE, Charrier R, Martin A, Thiran JP (2018) A real-time optimal inverse planning for Gamma Knife radiosurgery by convex optimization: description of the system and first dosimetry data. J Neurosurg 129:111–117. https://doi.org/10.3171/2018.7.Gks181572
Regis J, Carron R, Delsanti C, Porcheron D, Thomassin JM, Murracciole X, Roche PH (2013) Radiosurgery for vestibular schwannomas. Neurosurg Clin N Am 24:521–530. https://doi.org/10.1016/j.nec.2013.06.002
Regis J, Delsanti C, Roche PH, Thomassin JM, Pellet W (2004) Functional outcomes of radiosurgical treatment of vestibular schwannomas: 1000 successive cases and review of the literature. Neurochirurgie 50:301–311
Regis J, Roche PH, Delsanti C, Thomassin JM, Ouaknine M, Gabert K, Pellet W (2007) Modern management of vestibular schwannomas. Prog Neurol Surg 20:129–141
Regis J, Roche PH, Delsenti C, Soumare O, Thomassin JM, Pellet W (2002) Stereotactic radiosurgery for vestibular schwannoma. In: Pollock BE (ed) Contemporary stereotactic radiosurgery: thechnique and evaluation, vol Chap.9. Futura Publishing Company, Armonk, New York, pp 181-212
Regis J, Tamura M, Wikler D, Porcheron D, Levrier O (2008) Radiosurgery: operative technique, pitfalls and tips. Prog Neurol Surg 21:54–64
Hayashi M, Chernov M, Tamura N, Izawa M, Muragaki Y, Iseki H, Okada Y, Takakura K (2011) Gamma knife robotic microradiosurgery for benign skull base meningiomas: tumor shrinkage may depend on the amount of radiation energy delivered per lesion volume (unit energy). Stereotact Funct Neurosurg 89:6–16. https://doi.org/10.1159/000321184
Hayashi M, Chernov MF, Tamura N, Izawa M, Muragaki Y, Iseki H, Okada Y, Ivanov P, Regis J, Takakura K (2013) Concept of robotic gamma knife microradiosurgery and results of its clinical application in benign skull base tumors. Acta Neurochir Suppl 116:5–15. https://doi.org/10.1007/978-3-7091-1376-9_2
Massager N, Nissim O, Delbrouck C, Devriendt D, David P, Desmedt F, Wikler D, Hassid S, Brotchi J, Levivier M (2006) Role of intracanalicular volumetric and dosimetric parameters on hearing preservation after vestibular schwannoma radiosurgery. Int J Radiat Oncol Biol Phys 64:1331-1340. doi: 1310.1016/j.ijrobp.2005.1310.1030.
Wowra B, Muacevic A, Jess-Hempen A, Hempel JM, Muller-Schunk S, Tonn JC (2005) Outpatient gamma knife surgery for vestibular schwannoma: definition of the therapeutic profile based on a 10-year experience. J Neurosurg 102(Suppl):114–118
Funding
APHM (Assistance Public Hopitaux de Marseille) provided financial support by paying the insurances. This work was supported by Intuitive Therapeutics through a research grant. The sponsor had no role in the design of this research, nor in how it was conducted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript with the exception of Jean Régis who is a consultant for and has received a research grant from Elekta, AB & Medtronic.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (CPPRB: Comité de Protection des Personnes pour la recherche en Biologie) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The ethics committee authorized this study on the November 11, 2017, under the name « Original title in French: Protocole d’évaluation d’un algorithme de planification pour la radiochirurgie par Gamma Knife (SPEED) » under the registration number 2017-A02753-50 (NTC03520829). This was a non-interventional, single center, and prospective observational study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Tumors
Rights and permissions
About this article
Cite this article
Régis, J., Hamdi, H., Loundou, A. et al. Clinical evaluation of a real-time inverse planning for Gamma Knife radiosurgery by convex optimization: a prospective comparative trial in a series of vestibular schwannoma patients. Acta Neurochir 163, 981–989 (2021). https://doi.org/10.1007/s00701-020-04695-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04695-x