Abstract
Background
Enhanced recovery after surgery (ERAS) is a constant motivation. There is growing evidence that an endoscopic (rather than microscopic) transsphenoidal approach to pituitary tumours can play a role, facilitating faster recovery and a commensurate reduction in length of stay (LOS). Reducing LOS is beneficial to both patients and healthcare systems. We sought to assess the safety, patient feedback, and resource implications of adopting an enhanced recovery and accelerated discharge policy for elective pituitary surgery.
Methods
We retrospectively assessed two consecutive cohorts of patients undergoing elective surgery for pituitary adenoma in a single UK centre between July 2016 and November 2019. The pre-ERAS cohort included 52 sequential patients operated prior to protocol change. The ERAS cohort included 55 sequential patients operated after a protocol change. Patient demographic data, tumour characteristics, intra- and post-operative CSF leak, the rate and cause of readmission (within 30 days), and the mean and median LOS were recorded. Patient feedback was collected from a subset of patients (n = 23) in the ERAS group.
Results
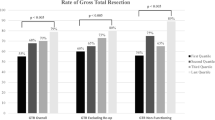
The two cohorts were well-matched with respect to their demographic, pathological, and operative characteristics. The rates of readmission within 30 days of discharge were similar between the two groups (8% pre-ERAS cohort, 9% ERAS cohort, p = 0.75). In the pre-ERAS cohort, the mean LOS was 4.5 days and median LOS was 3 days. This compares with significant reduction in LOS for the ERAS group: mean of 1.7 days and median of 1 day (p < 0.05). Thirty-nine of 55 patients in the ERAS group were discharged on post-operative day 1. Patient feedback was very positive in the ERAS group (mean patient satisfaction score of 9.7/10 using a Likert scale).
Conclusions
An enhanced recovery protocol after elective endoscopic pituitary surgery is safe, reduces length of stay, and is associated with high patient satisfaction.

Similar content being viewed by others
References
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617
Koupparis A, Dunn J, Gillatt D et al (2010) Improvement of an enhanced recovery protocol for radical cystecomy. British Journal of Medical and Surgical Urology 3:237–240
Lassen K, Soop M, Nygren J et al (2009) Consensus review of optimal perioperative care in colorectal surgery: enhanced recovery after surgery (ERAS) group recommendations. Arch Surg 144:961–969
Podore PC, Throop EB (1999) Infrarenal aortic surgery with a 3-day hospital stay: a report on success with a clinical pathway. J Vasc Surg 29:787–792
Tovar EA, Roethe RA, Weissig MD et al (1998) One-day admission for lung lobectomy: an incidental result of a clinical pathway. Ann Thorac Surg 65:803–806
Higgins TS, Courtemanche C, Karakla D et al (2008) Analysis of transnasal endoscopic versus transseptal microscopic approach for excision of pituitary tumors. Am J Rhinol 22(6):649–652
Barker FG II, Klibanski A, Swearingen B (2003) Transsphenoidal surgery for pituitary tumors in the United States, 1996–2000: mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab 88(10):4709–4719
Cappabianca P, Alfieri A, Colao A et al (1999) Endoscopic endonasal transsphenoidal approach: an additional reason in support of surgery in the management of pituitary lesions. Skull Base Surg 9(2):109–117
Casler JD (2005) Doolittle AM, Mair EA. Endoscopic surgery of the anterior skull base. Laryngoscope 115(1):16–24
Neal JG, Patel SJ, Kulbersh JS et al (2007) Comparison of techniques for transsphenoidal pituitary surgery. Am J Rhinol 21(2):203–206
Rotenberg B, Tam S, Ryu WH et al (2010) Microscopic versus endoscopic pituitary surgery: a systematic review. Laryngoscope 120(7):1292–1297
Sarkiss CA, Lee J, Papin JA et al (2015) Pilot study on early postoperative discharge in pituitary adenoma patients: effect of socioeconomic factors and benefit of specialized pituitary centers. J Neurol Surg B Skull Base 76(4):323–330
Thomas JG, Gadgil N, Samson SL et al (2014) Prospective trial of a short hospital stay protocol after endoscopic endonasal pituitary adenoma surgery. World Neurosurg 81(3–4):576–583
Recommendations for low volume pituitary surgery. Society of British Neurological Surgery Policies and Publications. https://www.sbns.org.uk/index.php/download_file/view/1448/87/ Accessed 15 Jan 2020
The Leeds Pituitary Centre Handbook, available on the Leeds Teaching Hospitals website. https://www.leedsth.nhs.uk/patients-visitors/patient-and-visitor-information/patient-information-leaflets/ Accessed 15 Jan 2020
Smith I, Krankes P, Murat I et al (2011) Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 28(8):556–569
Schraag S, Pradelli L, Alsaleh AJO et al (2018) Propofol vs. inhalational agents to maintain general anaesthesia in ambulatory and in-patient surgery: a systematic review and meta-analysis. BMC Anesthiol 18(1):162
Kranke P, Jokinen J, Pace NL, et al. (2015) Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 16;(7)
Cornesse D, Senard M, Hans GA et al (2010) Comparison between two intraoperative intravenous loading doses of paracetamol on pain after minor hand surgery: two grams versus one gram. Acta Chir Belg 110(5):529–532
Milton Raff M, Belbachir A, El-Tallawy S et al (2018) Intravenous oxycodone versus other intravenous strong opioids for acute postoperative pain control: a systematic review of randomized controlled trials. Pain and Therapy 1:19–39
Gan TJ, Diemunsch P, Habib AS et al (2014) Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 118(1):85–113
Spitzer M, Wildenhain J, Rappsilber J et al (2014) BoxPlotR: a web tool for generation of box plots. Nat Methods 11:121–122
Alzhrani G, Sivakumar W, Park MS, Taussky P, Couldwell WT (2018) Delayed complications after transsphenoidal surgery for pituitary adenomas. World Neurosurg 109:233–241
Zimmer LA, Andaluz N (2018) Incidence of epistaxis after endoscopic pituitary surgery: proposed treatment algorithm. Ear Nose Throat J 97(3):E44–E48
Zwagerman NT, Wang EW, Shin SS et al (2019) Does lumbar drainage reduce postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery? A prospective, randomized controlled trial. Neurosurg 131:1172–1178
Nix P, Tyagi A, Phillips N (2015) Evolution of a UK endoscopic anterior skull base pituitary service-the first 123 patients. Clin Otolaryngol. https://doi.org/10.1111/coa.12514
Strickland BA, Lucas J, Harris B et al (2018) Identification and repair of intraoperative cerebrospinal fluid leaks in endonasal transsphenoidal pituitary surgery: surgical experience in a series of 1002 patients. J Neurosurg 129(2):425–429
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict interest.
Ethical approval
For this type of study, formal consent is not required. This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pituitaries
Rights and permissions
About this article
Cite this article
Hughes, M.A., Culpin, E., Darley, R. et al. Enhanced recovery and accelerated discharge after endoscopic transsphenoidal pituitary surgery: safety, patient feedback, and cost implications. Acta Neurochir 162, 1281–1286 (2020). https://doi.org/10.1007/s00701-020-04282-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04282-0