Abstract
Background
Meningiomas may show a different WHO grade and variable biological and clinical behaviors. The aim of the present study is to assess whether WHO grade, proliferation index, progesterone receptor (PR) expression, histological subtype, neuroradiological features, and the recurrence rate differ depending on the tumor location.
Methods
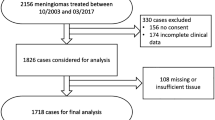
Three hundred meningiomas operated on from 2006 to 2016 were reviewed. The WHO grade (2007 classification), Ki67-MIB1, progesterone receptor expression, and histological subtype were reexamined and correlated to the meningioma location, classified as medial skull base, lateral skull base, non-skull base, and spinal.
Results
Non-skull base and lateral skull base meningiomas showed significantly higher rates of atypical WHO II forms (34% and 25.5% respectively) than medial skull base (12.5%) and spinal ones (7%) (p = 0.0003) and also higher rates of tumors with Ki67-Li > 4% (42% and 38% vs 22% and 14%) (p = 0.0031). The rate of meningiomas with PR expression ≤ 50% was significantly lower in medial skull base (25%) than in non-skull base (48%) (p = 0.009). Meningothelial and transitional meningiomas were more frequent at the skull base (68.5% and 54.5%, respectively), the fibroblastic subtype at the non-skull base (48.5%), and the psammomatous at the spinal canal (50%) (p < 0.00001). Medial skull base and spinal meningiomas showed significantly lower size (p < 0.00001), lower rates of cases with lost arachnoid interface (p = 0.0022), and significantly lower recurrence rates (p = 0.0035) than lateral skull base and non-skull base meningiomas.
Conclusion
Medial skull base meningiomas show lower size, lower rate of atypical forms, lower Ki67-Li values, and significantly higher PR expression than those at the lateral skull base and non-skull base. This corresponds to lesser aggressiveness and lower recurrence rates.

Similar content being viewed by others
References
Albdezahar E, El-Gendi SM, Yehya A, Gowil AG (2011) Recurrence of benign meningiomas: predictive value of proliferative index, BCL2, p53, hormonal receptors and HER2 expression. Br J Neurosurg 25:707–713
Barresi V, Alafaci C, Caffo M, Barresi G, Tuccari G (2012) Clinicopathological characteristics, hormone receptor status and matrix metallo-proteinase-9 (MMP-9) immunohistochemical expression in spinal meningiomas. Pathol Res Pract 208:350–355
Batarfi M, Valasek P, Krejci E, Huang R, Patel K (2017) The development and origins of vertebrate meninges. Bio Comm 62:73–81
Bhat AR, Wani MA, Kirmani AR, Ramzan AU (2014) Histological subtypes and anatomical location correlated in meningeal brain tumors (meningiomas). J Neurosci Rural Pract 5:244–249
Catala M (1998) Embryonic and fetal development of structures associated with the cerebro-spinal fluid in man and other species. Part I: The ventricular system, meninges and choroid plexuses. Arch Anat Cytol Pathol 46:153–169
Claus EB, Park PJ, Carroll R, Chan J, Black PM (2008) Specific genes expressed in association with progesterone receptors in meningioma. Cancer Res 68:314–322
Cornelius JF, Slotty PJ, Steiger HJ, Hänggi D, Polivka M, George B (2013) Malignant potential of skull base meningioma s versus non-skull base meningioma’s: clinical series of 1.663 cases. Acta Neurochir 155:407–413
Giombini S, Solero CL, Lasio G, Morello G (1984) Immediate and late outcome of operations for parasagittal and falx meningiomas: report of 342 cases. Surg Neurol 21:427–435
Hale AT, Wang L, Strother MK, Chambless LB (2018) Differentiating meningioma grade by imaging features on magnetic resonance imaging. J Clin Neurosci 48:71–75
Hashimoto N, Rabo CS, Okita Y, Kinoshita M, Kagawa N, Fujimoto Y et al (2012) Slower growth of skull base meningiomas compared with non-skull base meningiomas based on volumetric and biological studies. J Neurosurg 116:574–580
Hwang WL, Marsicano AB, Niemierko A et al (2016) Imaging and extent of surgical resection predict risk of meningioma recurrence better than WHO histopathological grade. Neuro-Oncology 18:863–872
Ildan F, Erman T, Gocer AI et al (2007) Predicting the probability of meningioma recurrence in the preoperative and early postoperative period; a multivariate analysis in the midterm follow-up. Skull Base 17:157–171
Jiang X, Iseki S, Maxson RE, Sucov HM, Morriss-Kay GM (2002) Tissue origins and interactions in the mammalian skull vault. Dev Biol 241:106–116
Kalamarides M, Stemmer-Rachamimov AO, Niwa-Kawakita M, Chareyre F, Taranchon E, Han ZY et al (2011) Identification of a progenitor cell of origin capable of generating diverse meningioma histological subtypes. Oncogene 30:2333–2344
Kane AJ, Sughrue ME, Rutkowski MJ, Shangari G, Fang S, Mcdermott MW et al (2011) Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer 117:1272–1278
Kasuya H, Kubo O, Tanaka M, Amano K, Kato K, Hori T (2006) Clinical and radiological features related to the growth potential of meningiomas. Neurosurg Rev 29:293–296
Klekamp J, Samii M (1999) Surgical results for spinal meningiomas. Surg Neurol 52:552–562
Koutourousiou M, Fernandez-Miranda JC, Stefko ST, Wang EW, Snyderman CH, Gardner PA (2014) Endoscopic endonasal surgery for suprasellar meningiomas: experience with 75 patients. J Neurosurg 120:1326–1339
Kuroi Y, Matsumoto K, Shibuya M, Kasuya H (2018) Progesterone receptor is responsible for benign biology of skull base meningioma. World Neurosurg 118:e918–e924
Lam Shin Cheung V, Kim A, Sahgal A, Das S (2018) Meningioma recurrence rates following treatment: a systematic analysis. J Neuro-Oncol 136:351–361
Lee JH, Sade B, Choi E, Golubic M, Prayson R (2006) Meningothelioma as the predominant histological subtype of midline skull base and spinal meningioma. J Neurosurg 105:60–64
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Magill ST, Young JS, Chae R, Aghi MK, Theodosopoulos PV, McDermott MW (2018) Relationship between tumor location, size, and WHO grade in meningioma. Neurosurg Focus 44:E4
Maiti TK, Bir SC, Patra DP, Kalakoti P, Guthikonda B, Nanda A (2016) Spinal meningiomas: clinicoradiological factors predicting recurrence and functional outcome. Neurosurg Focus 41(2):E6
Maiuri F, Del Basso De Caro ML, de Divitiis O, Guadagno E, Mariniello G. (2019) Recurrence of spinal meningiomas: analysis of the risk factors. Br J Neurosurg
Maiuri F, Del Basso De Caro ML, Esposito F, Cappabianca P, Strazzullo V, Pettinato G et al (2007) Recurrences of meningioma: predictive value of pathological features and hormonal and growth factors. J Neuro-Oncol 82:63–68
Maiuri F, Iaconetta G, de Divitiis O, Cirillo S, Di Salle F, De Caro ML (1999) Intracranial meningiomas: correlations between MR imaging and histology. Eur J Radiol 31(1):69–75
Mansouri A, Klironomos G, Taslimi S, Kilian A, Gentili F et al (2016) Surgically resected skull base meningiomas demonstrate a divergent postoperative recurrence pattern compared with non-skull base meningiomas. J Neurosurg 125:431–440
Mariniello G, Maiuri F, Strianese D, Donzelli R, Iuliano A, Tranfa F et al (2008) Spheno-orbital meningiomas: surgical approaches and outcome according to the intraorbital extent. Zentralbl Neurochir 69:175–181
Maroon JC, Kennerdell JS, Vidovich DV, Abla A, Sternau L (1994) Recurrent spheno-orbital meningioma. J Neurosurg 80:202–208
McGovern SL, Aldape KD, Munsell MF, Mahajan A, DeMonte F, Woo SY (2010) A comparison of World Health Organization tumor grades at recurrence in patients with non-skull base and skull base meningiomas. J Neurosurg 112:925–933
Meling TR, Da Broi M, Scheie D, Helseth E (2019) Meningiomas: skull base versus non-skull base. Neurosurg Rev 42:163–173
Metellus P, Nanni I, Dussert C, Trinkhaus M, Fuentes S, Chinot O et al (2008) Prognostic implications of biologic markers in intracranial meningiomas: 120 cases. Neurochirurgie 54:750–756
Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL (1985) Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg 62:18–24
Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T et al (2012) Long-term surgical outcomes of spinal meningiomas. Spine (Phila Pa 1976) 37:E617–E623
Nakasu S, Fukami T, Jito J, Nozaki K (2009) Recurrence and regrowth of benign meningiomas. Brain Tumor Pathol 26:69–72
Nakasu S, Nakasu Y, Nakajima M, Matsuda M, Handa J (1999) Preoperative identification of meningiomas that are highly likely to recur. J Neurosurg 90:455–462
Nanda A, Vannemreddy P (2008) Recurrence and outcome in skull base meningiomas: do they differ from other intracranial meningiomas? Skull Base 18:243–252
O’Rahilly R, Müller F (1986) The meninges in human development. J Neuropathol Exp Neurol 45:588–608
Perry A, Gutmann DH, Reifenberger G (2004) Molecular pathogenesis of meningiomas. J Neuro-Oncol 70:183–202
Pravdenkova S, Al-Mefty O, Sawyer J, Husain M (2006) Progesterone and estrogen receptors: opposing prognostic indicators in meningiomas. J Neurosurg 105:163–173
Rohringer M, Sutherland GR, Louw DF, Sima AA (1989) Incidence and clinicopathological features of meningioma. J Neurosurg 71:665–672
Roser F, Nakamura M, Bellinzona M, Ritz R, Ostertag H, Tatagiba MS (2006) Proliferation potential of spinal meningiomas. Eur Spine J 15:211–215
Roser F, Nakamura M, Bellinzona M, Rosahl SK, Ostertag H, Samii M (2004) The prognostic value of progesterone receptor status in meningiomas. J Clin Pathol 57:1033–1037
Roser F, Nakamura M, Ritz R, Bellinzona M, Dietz K, Samii M, Tatagiba MS (2005) Proliferation and progesterone receptor status in benign meningiomas are not age dependent. Cancer 104:598–601
Roser F, Samii M, Ostertag H, Bellinzona M (2004) The Ki-67 proliferation antigen in meningiomas. Experience in 600 cases. Acta Neurochir 146:37–44
Sade B, Chahlavi A, Krishnaney A, Nagel S, Choi E, Lee JH (2007) World Health Organization grades II and III meningiomas are rare in the cranial base and spine. Neurosurgery 61:1194–1198
Sandalcioglu IE, Gasser T, Mohr C, Stolke D, Wiedemayer H (2005) Spheno orbital meningiomas: interdisciplinary surgical approach, respectability and long-term results. J Craniomaxillofac Surg 33:260–266
Savardekar AR, Patra DP, Bir S, Thakur JD, Mohammed N, Bollam P, Georgescu MM, Nanda A (2018) Differential tumor progression patterns in skull base versus non-skull base meningiomas: a critical analysis from a long-term follow-up study and review of literature. World Neurosurg 112:e74–e83
Spektor S, Valarezo J, Fliss DM, Gil Z, Cohen J, Goldman J et al (2005) Olfactory groove meningiomas from neurosurgical and ear, nose, and throat perspectives: approaches, techniques, and outcomes. Neurosurgery 57(4 Suppl):268–280
Spille DC, Sporns PB, Heβ K, Stummer W, Brokinkel B (2019) Predict of high-grade histology and recurrence in meningiomas using routine preoperative magnetic resonance imaging: a systematic review. World Neurosurg 128:174–181
Standring S, Ellis H, Wigley C (2016) Gray’s anatomy: the anatomical basis of clinical practice. Elsevier Churchill Livingstone, New York
Wolfsberger S, Doostkam S, Boecher-Schwarz HG, Roessler K, van Trotsenburg M, Hainfellner JA et al (2004) Progesterone-receptor index in meningiomas: correlation with clinico-pathological parameters and review of the literature. Neurosurg Rev 27:238–245
Zhou P, Ma W, Yin S, Li Y, Jiang S (2013) Three risk factors for WHO grade II and III meningiomas: a study of 1737 cases from a single center. Neurol India 61:40–44
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this retrospective study, no institutional review board approval or patient consent is required per institutional policy.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tumor - Meningioma
Rights and permissions
About this article
Cite this article
Maiuri, F., Mariniello, G., Guadagno, E. et al. WHO grade, proliferation index, and progesterone receptor expression are different according to the location of meningioma. Acta Neurochir 161, 2553–2561 (2019). https://doi.org/10.1007/s00701-019-04084-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04084-z