Abstract
Background
The postoperative metabolic states of subarachnoid hemorrhage (SAH) patients were investigated using indirect calorimetry (IDC) and various nutritional evaluations to establish any difference in perioperative metabolic and nutritional states between microsurgical and endovascular treatment.
Methods
This study included 30 acute aneurysmal SAH patients with ruptured intracranial aneurysms treated by surgical clipping (n = 16) or coil embolization (n = 14) at a single institute. The resting energy expenditure (REE) and respiratory quotient were measured using IDC on days 1, 4, 7, 10, 14, and 17–21 after the operation. Various blood tests, including C-reactive protein (CRP) and prealbumin, were evaluated on the same days.
Results
The clipping group showed a significant increase in REE/basal energy expenditure (BEE) compared with the coiling group on days 1 and 4 (p = 0.04 and 0.03, respectively). No significant differences were found on days 7, 10, 14, and 17–21. The mean REE/BEE on days 1–14 and 1–21 showed no significant differences between the groups with repeated measures analysis of variance. The clipping group showed a significant decrease of prealbumin on day 4 and significant increase in CRP on days 1, 4, and 7.
Conclusions
The clipping group was in the hypermetabolic state compared with the coiling group during the very early postoperative period. However, the difference associated with the treatment modality was relatively small compared to the effects of the SAH and of the sequelae.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients in the acute phase of subarachnoid hemorrhage (SAH) may develop systemic inflammatory response syndrome as well as deterioration in physical or neurological condition, despite multidisciplinary therapy [27]. In addition, invasive surgical procedures such as microsurgical clipping or endovascular coiling may be necessary to treat the ruptured aneurysm. Patients may enter the hypercatabolic state caused by elevation of catecholamine secretion in the perioperative period [1, 10, 25]. Postoperative malnutrition caused by the hypercatabolic state can result in various problems following surgery such as the occurrence of cerebrovascular spasm. Therefore, assessment of the metabolic and nutritional states is important in the perioperative period of SAH [1, 10, 14, 25].
Coil embolization has been widely adopted for the treatment of cerebral aneurysm since the 1990s and has revolutionized the treatment of aneurysmal SAH [7]. Microsurgical clipping has been carefully compared with endovascular coiling regarding the safety and efficacy to determine whether endovascular coiling can replace microsurgical clipping [11, 13]. However, no study has compared microsurgical clipping with endovascular coiling regarding the metabolic and nutritional states during the perioperative period.
The present study investigated the postoperative metabolic state of patients with aneurysmal SAH using indirect calorimetry (IDC) and various nutritional evaluations at short intervals to establish any difference in perioperative metabolic and nutritional states between microsurgical and endovascular treatment.
Patients and methods
A total of 51 patients with acute SAH underwent microsurgical clipping or endovascular coiling for the treatment of ruptured aneurysm at Takasaki General Medical Center between June 2014 and December 2015. Patients were excluded who could not undergo IDC (coma, use of a ventilator or high-concentration oxygen, difficulty keeping still in bed, and so on) and had hypoalbuminemia due to liver dysfunction before admission. Finally, 30 patients, 8 males and 22 females, with median age of 65.5 years (interquartile range, 59.8–71.5), were included in this study (Table 1). Microsurgical clipping or coil embolization was selected for treatment of the aneurysm according to the location and shape of the aneurysm or the physical condition. Clipping was preferred for middle cerebral artery aneurysms. Coiling was preferred for posterior circulation aneurysms (Table 1) [22]. Selection of microsurgical clipping or endovascular coiling for internal carotid artery and anterior cerebral artery aneurysms was decided after discussion based on preoperative imaging findings involving the neurosurgical team. Clipping was preferred for thrombotic aneurysms, very small aneurysms, and distal anterior cerebral artery aneurysms [16]. Coiling was preferred as less invasive and safer in the presence of complicated surrounding anatomy and multiple aneurysms. Coiling was preferred in only two cases because of poor general condition associated with chronic heart failure and after glioblastoma resection.
All operations including both clipping and coiling were performed under general anesthesia, using concurrent inhalation anesthetic (sevoflurane or desflurane), propofol, rocuronium, and remifentanil. Fentanyl was also used in many cases. Only one patient treated by coiling did not undergo intubation, but was sedated mainly with continuous administration of propofol. Several surgeons performed the operations. All clipping surgeries were performed through conventional fronto-temporal or bifrontal craniotomy without minicraniotomy, anastomoses or through invasive skull base drilling [12].
This study was approved by the Institutional Review Board of Takasaki General Medical Center. Informed consent was obtained from the patients or family.
Medical treatment after clipping or coiling
The absence of problematic bleeding was confirmed on the day after the operation, and then fasudil hydrochloride and ozagrel sodium were administered to prevent cerebral vasospasm [20, 24]. Fluid to maintain adequate intravascular water volume was also given to patients in relatively favorable general condition including cardiac function. A vasopressor was sometimes administered to maintain blood pressure for prevention of cerebral vasospasm [8]. Early enteral feeding or oral nutrition was attempted after the operation [3]. Various methods and quantities of nutritional administration were used, such as oral intake, enteral feeding, peripheral parenteral nutrition, and/or central venous parenteral nutrition, but we tried to administer adequate energy and protein. Priority was given to oral intake. A sufficient amount of energy was administered to many patients. However, the amount of protein was occasionally less than the target value (1.0–1.5 g/kg/day) (data not shown).
Measurement of systemic metabolism and energy consumption
The resting energy expenditure (REE) and respiratory quotient (RQ) were measured using a portable IDC device (AE-100i®, Minato Medical Science Co., Ltd., Osaka, Japan) on days 1, 4, 7, 10, 14, and 17–21 after the operation. All measurements were conducted at the bedside before feeding with room air. The gas analyzer was automatically calibrated before each measurement. After the patient had rested for over 30 min, the mask was placed on the patient’s face and then the oxygen and carbon dioxide amounts passing through the sampling tube were detected with the gas analyzer [17]. All measurements were conducted for 15 min, and the first 5 min of data were discarded [14]. The REE was calculated with the modified Weir formula as follows: REE (kcal/day) = (3.9 × VO2 [ml/min] + 1.1 × VCO2 [ml/min]) × 1.44, where VO2 is volumetric oxygen consumption and VCO2 is volumetric carbon dioxide elimination [26].
In addition, basal energy expenditure (BEE) was calculated by the Harris-Benedict formula [9]. The values of the BEE (kcal/day) were calculated as follows: males, 66.47 + 13.75 × weight (kg) + 5 × height (cm) – 6.76 × age (years); females, 655.1 + 9.56 × weight (kg) + 1.85 × height (cm) – 4.86 × age (years). REE/BEE was calculated to correct for sex, age, and build.
Nutritional and inflammation assessments
Nutritional state was assessed with blood tests, caloric intake, and nitrogen intake. The blood tests, including the white blood cell count, C-reactive protein (CRP), and prealbumin, were evaluated on days 1, 4, 7, 10, 14, and 17–21. Nutritional intake including oral intake, enteral feeding, peripheral parenteral nutrition, and/or central venous parenteral nutrition was calculated, and then the caloric and nitrogen intakes were calculated. The collaborating nutritional support team added supplementary nutrition according to the patient. Records of nutritional intake were maintained by nurses of the intensive care unit (ICU) and neurosurgical ward.
Statistical analysis
The data were analyzed with freely available EZR statistical software. Differences in the characteristics between the groups were evaluated by Fisher’s exact test or Mann-Whitney U test. Comparisons between the groups regarding REE/BEE, RQ, and prealbumin were evaluated by the Student’s t-test because these data were normally distributed in most measurements. Comparison between the groups regarding CRP was evaluated by the Mann-Whitney U test because these data were not normally distributed at all measurement dates in the coiling group. Additionally, comparison of REE/BEE between the groups used repeated measures analysis of variance (ANOVA). We set statistical significance at p < 0.05. No corrections were made for multiple comparisons.
Results
Patient characteristics
Microsurgical clipping was performed for 16 patients and endovascular coiling for 14 patients among the total of 30 patients. Decompressive craniectomy was combined with clipping in four patients to control the intracranial pressure. All patients underwent procedures including microsurgical clipping or endovascular coiling for aneurysm only once during the hospitalization. Ventricular drainage was placed for three patients (clipping:coiling = 2:1, 1–21 days, average 9 days), cisternal drainage for 4 patients (clipping = 4, 2–16 days, average 11 days), and spinal drainage for 6 patients (clipping:coiling = 2:4, 5–14 days, average 9 days). A shunt procedure was performed in ten patients (clipping:coiling = 5:5) to treat hydrocephalus. Eleven patients suffered symptomatic vasospasm (clipping:coiling = 6:5), and five suffered cerebral infarction due to delayed cerebral ischemia (clipping:coiling = 2:3). Intra-arterial infusion of papaverine hydrochloride was performed for only one patient after coiling to treat cerebral vasospasm. All major adverse events within 21 days after the operation were assessed. Nine patients suffered infections, including mild meningitis, respiratory infection, urinary infection, and unknown sepsis within 21 days after the operation (clipping:coiling = 4:5). These infections were treated with antibiotics. Some patients suffered cardiac dysfunction (clipping:coiling = 2:2), convulsion (clipping:coiling = 1:1), deep venous thrombosis (clipping:coiling = 1:0), and drug eruption (clipping:coiling = 1:0). Blood tests showed liver dysfunction [aspartate transaminase > 90 U/l or/and alanine aminotransferase > 126 U/l (male), > 69 U/l (female)] (clipping:coiling = 5:2), kidney dysfunction [creatinine > 1.605 mg/dl (male), >1.185 mg/dl (female)] (clipping:coiling = 0:1), electrolyte abnormality (K > 5.5 mmol/l, K < 3.0 mmol/l, Na > 150 mmol/l, or/and Na < 130 mmol/l) (clipping:coiling = 6:5), and anemia (hemoglobin < 10.0 g/dl) (clipping:coiling = 6:2). No significant intergroup differences were found with any of the major adverse events. The blood tests were assessed by reference to the Common Terminology Criteria for Adverse Events version 4.0, of the US National Cancer Institute.
The profiles of the groups including age, sex, body mass index (BMI), World Federation of Neurosurgical Societies (WFNS) grade, modified Rankin Scale (mRS) at the time of discharge, incidence of symptomatic cerebral vasospasm or infarction, and number of shunt procedures are shown in Table 1 [23]. The median WFNS grade was 2 and mRS was 1 in both groups. No significant intergroup differences were found in any of the profiles. Both microsurgical clipping and endovascular coiling were performed for anterior communicating artery and internal carotid artery aneurysms. Only microsurgical clipping was performed for middle cerebral artery aneurysms and only endovascular coiling for posterior circulation aneurysms (Table 1).
Measurements of indirect calorimetry
The mean REE/BEE of each group is shown in Fig. 1 and Table 2. The mean REE/BEE was higher than 1 in both groups. The mean REE/BEE approached 1 at almost 3 weeks after the operation. The clipping group showed a significant increase in REE/BEE on days 1 and 4 compared with the coiling group (p = 0.04 and 0.03, respectively). The mean REE/BEE on days 1–14 and 1–21 showed no significant differences between the groups with repeated measures ANOVA. The mean REE/BEE of the clipping group increased from the early postoperative period without any obvious peak. The mean REE/BEE of the coiling group peaked on day 10 (Fig. 1).
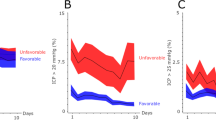
Supplementary comparison of all 30 patients evaluated the mean REE/BEE in various clinical statuses, including mild (WFNS grade I or II) or severe (WFNS grade III, IV, or V) SAH grades, with or without symptomatic vasospasm, need or no need for shunts for hydrocephalus, and lower (0, 1, or 2) or higher (3, 4, 5, or 6) mRS at the time of discharge on representative days 1 and 10 after treatment. The patients with higher mRS and patients with hydrocephalus treated by shunt showed a significant increase in REE/BEE on day 10 (p = 0.02 and < 0.05, respectively) (Fig. 2).
REE/BEE (mean ± standard deviation) in various clinical statuses on days 1 and 10. Higher modified Rankin Scale (mRS) group and patients with hydrocephalus treated by shunt show a significant increase in REE/BEE on day 10 (*p < 0.05). a REE/BEE of the patients in mild World Federation of Neurosurgical Societies (WFNS) grades and severe WFNS grades. b REE/BEE of the patients with and without symptomatic vasospasm. c REE/BEE of the patients with and without shunt procedure. d REE/BEE of the patients with lower mRS and higher mRS
Nutritional and inflammation assessments
Prealbumin was measured at short intervals after the operation (Fig. 3). Prealbumin showed a significant decrease on day 4 in the clipping group compared with the coiling group. This significant difference occurred only on day 4, and no differences were found after day 7. CRP, indicating the inflammatory response, was significantly increased on days 1, 4, and 7 in the clipping group compared with the coiling group (Fig. 4). The mean RQ in both the clipping and coiling groups was not lower than 0.85 on all evaluated days, suggesting sufficient nutritional feeding during the postoperative period.
Discussion
The present investigation of the postoperative metabolic state of patients with aneurysmal SAH using IDC and various nutritional evaluations at short intervals in 16 patients treated by microsurgical clipping and 14 patients treated by endovascular coiling found that the mean REE/BEE was higher than 1 in both groups. The clipping group showed a significant increase in REE/BEE on days 1 and 4 compared with the coiling group (p = 0.04 and 0.03, respectively). No significant differences were found at the other measurement points. The mean REE/BEE on days 1–14 and 1–21 showed no significant differences between the groups. Supplementary comparison of all 30 cases found that the patients with higher mRS at discharge and with hydrocephalus treated by shunt showed a significant increase in REE/BEE on day 10 (p = 0.02 and <0.05, respectively). The clipping group showed a significant decrease of prealbumin on day 4 and significant increase in CRP on days 1, 4, and 7.
IDC is the most common method for measuring the energy consumption of patients. Compared with the conventional devices, smaller simple-to-use portable devices are now available for critically ill patients in the ICU. Measurement of energy consumption using IDC is recommended for critically ill patients [21]. Malnutrition is likely to occur in patients with SAH because of hypercatabolism with catecholamine surge [19]. In addition, low plasma osmotic pressure associated with malnutrition combined with cerebral vasospasm can cause severe cerebral infarction. However, the metabolic and nutritional states of SAH patients are little understood. Increased energy expenditure measured using IDC was found in Japanese patients with ruptured aneurysm [25]. In addition, REE/BEE reached the maximum level on day 10 after microsurgical clipping in 36 aneurysmal SAH patients [10]. The mean REE/BEE was 1.46 ± 0.24 and 1.98 ± 0.78 in patients with Hunt and Hess grades 1–2 and 3–5, respectively, which indicated that energy expenditure increased greatly [10]. On the other hand, median value of energy expenditure on days 1 and 7 after endovascular coiling for the first time was 1.12 (interquartile range, 1.05–1.23) [14]. A recent extensive survey of the nutritional state of SAH patients did not adequately compare aneurysm treatments or changes with time [1].
Energy expenditure after microsurgical clipping has generally been considered to greatly increase [10, 25]. On the other hand, energy expenditure after coil embolization was lower than reported after microsurgical clipping [14]. The present study first performed direct comparison of the postoperative energy expenditure using the same measurement method between the clipping and coiling groups under the control of a single facility during the same period. Endovascular coiling is increasingly performed worldwide instead of microsurgical clipping, but the choice of treatment method tends to depend on the location of the aneurysm or the difficulty of treatment in Japan at present [13]. For this reason, the endovascular coiling group included a few cases of posterior circulation aneurysm. In contrast, no significant differences were found in the patient profiles including age, sex, BMI, incidence of symptomatic cerebral vasospasm, WFNS grade, adverse events, and mRS at the time of discharge.
The clipping group showed significant increases in REE/BEE on days 1 and 4 compared with the coiling group. CRP of the clipping group greatly increased on days 1 and 4 compared with the coiling group, which reflected the invasiveness of craniotomy during the early postoperative period. However, the mean REE/BEE on days 1–14 and 1–21 showed no significant differences between the groups. The present findings may indicate that the clipping group was in the hypermetabolic state compared with the coiling group during the very early postoperative period (< day 7). Consequently, the effects of surgical invasiveness may be partially masked by the systemic reactions caused by the SAH and complications. Supplementary comparisons of all 30 patients found that patients with higher mRS at discharge and patients with hydrocephalus treated by shunt showed significant increases in REE/BEE on day 10 (Fig. 2), suggesting that complications and the associated stress may cause changes in the postoperative metabolic balance. The REE/BEE of the coiling group in our study was close to Nagano’s measurement value [14], but the values of the clipping group in our study were far below Kasuya’s measurement values [10]. Clearly, coil embolization is less invasive than microsurgical clipping with craniotomy. However, the difference in overall metabolic state and energy consumption associated with the treatment modality was relatively small compared to the effect of the SAH and of the sequelae during the perioperative period after aneurysmal SAH.
Recent remarkable developments in interventional radiology (IVR) have lead to changes in the field of cardiovascular diseases. Many comparative trials have been reported in this field [2, 5]. Coil embolization has similar or greater safety and efficacy compared with microsurgical clipping [13]. Coil embolization is thought to be minimally invasive, partly because craniotomy is not required. However, our findings suggest that the invasiveness of craniotomy may not be such a big disadvantage compared with IVR for patients with acute SAH regarding the overall metabolic state and energy consumption.
Nutritional management of patients with severe acute conditions is controversial, but trophic feeding is considered helpful and overfeeding is harmful [4, 6, 15, 18]. The present study found lower increases in REE after both clipping and coiling compared with previously reported findings after microsurgical clipping. Therefore, the measurement of individual energy consumption using IDC is helpful for prevention of overfeeding after surgery in patients with SAH.
The present study only included a small number of cases, so further experience is necessary. Selection of microsurgical clipping or endovascular coiling was decided by the neurosurgical team comprehensively, so the selection bias may have affected the results. In addition, although the nutrition administration policy was basically unified for all patients, differences in administration method, nutritional components, and amount of nutrition may have affected the results.
Conclusions
The present study found that patients who underwent clipping were in the hypermetabolic state compared with patients who underwent coiling during the very early postoperative period, but this difference was relatively small during the overall perioperative period after SAH compared to the effects of the SAH and of the sequelae.
References
Badjatia N, Monahan A, Carpenter A, Zimmerman J, Schmidt JM, Claassen J, Connolly ES, Mayer SA, Karmally W, Seres D (2015) Inflammation, negative nitrogen balance, and outcome after aneurysmal subarachnoid hemorrhage. Neurology 84:680–687
Bangalore S, Guo Y, Samadashvili Z, Blecker S, Hannan EL (2016) Revascularization in patients with multivessel coronary artery disease and severe left ventricular systolic dysfunction: everolimus-eluting stents versus coronary artery bypass graft surgery. Circulation 133:2132–2140
Dennis MS, Lewis SC, Warlow C (2005) FOOD trial collaboration: effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomized controlled trial. Lancet 365:764–772
Dissanaike S, Shelton M, Warner K, O'Keefe GE (2007) The risk for bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition. Crit Care 11:R114
González-Saldivar H, Rodriguez-Pascual C, de la Morena G, Fernández-Golfín C, Amorós C, Alonso MB, Dolz LM, Solé AA, Guzmán-Martínez G, Gómez-Doblas JJ, Jiménez AA, Fuentes ME, Gay LG, Ortiz MR, Avanzas P, Abu-Assi E, Ripoll-Vera T, Díaz-Castro O, Osinalde EP, Martínez-Sellés M, Influencia del Diagnóstico de Estenosis Aórtica Severa—Influence of the Severe Aortic Stenosis Diagnosis (IDEAS) Investigators (2016) Comparison of 1-year outcome in patients with severe aorta stenosis treated conservatively or by aortic valve replacement or by percutaneous transcatheter aortic valve implantation (data from a multicenter Spanish registry). Am J Cardiol 118:244–250
Grau T, Bonet A, Rubio M, Mateo D, Farré M, Acosta JA, Blesa A, Montejo JC, de Lorenzo AG, Mesejo A (2007) Working group on nutrition and metabolism of the Spanish Society of Critical Care: liver dysfunction associated with artificial nutrition in critically ill patients. Crit Care 11:R10
Guglielmi G, Viñuela F, Sepetka I, Macellari V (1991) Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: electrochemical basis, technique, and experimental results. J Neurosurg 75:1–7
Hadeishi H, Mizuno M, Suzuki A, Yasui N (1990) Hyperdynamic therapy for cerebral vasospasm. Neurol Med Chir (Tokyo) 30:317–323
Harris JA, Benedict FG (1918) A biometric study of human basal metabolism. Proc Natl Acad Sci U S A 4:370–373
Kasuya H, Kawashima A, Namiki K, Shimizu T, Takakura K (1998) Metabolic profiles of patients with subarachnoid hemorrhage treated by early surgery. Neurosurgery 42:1268–1274
McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, Albuquerque FC (2012) The barrow ruptured aneurysm trial. J Neurosurg 116:135–144
Mitchell P, Vindlacheruvu RR, Mahmood K, Ashpole RD, Grivas A, Mendelow AD (2005) Supraorbital eyebrow minicraniotomy for anterior circulation aneurysms. Surg Neurol 63:47–51
Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366:809–817
Nagano A, Yamada Y, Miyake H, Domen K, Koyama T (2016) Increased resting energy expenditure after endovascular coiling for subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 25:813–818
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, Morris A, Dong N, Rock P (2012) Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA 307:795–803
Nguyen TN, Raymond J, Guilbert F, Roy D, Bérubé MD, Mahmoud M, Weill A (2008) Association of endovascular therapy of very small ruptured aneurysms with higher rates of procedure-related rupture. J Neurosurg 108:1088–1092
Oshima T, Berger MM, De Waele E, Guttormsen AB, Heidegger CP, Hiesmayr M, Singer P, Wernerman J, Pichard C (2017) Indirect calorimetry in nutritional therapy. A position paper by the ICALIC study group. Clin Nutr 36(3):651–662
Reid C (2006) Frequency of under- and overfeeding in mechanically ventilated ICU patients: causes and possible consequences. J Hum Nutr Diet 19:13–22
Salem R, Vallée F, Dépret F, Callebert J, Maurice JP, Marty P, Matéo J, Madadaki C, Houdart E, Bresson D, Froelich S, Stapf C, Payen D, Mebazaa A (2014) Subarachnoid hemorrhage induces an early and reversible cardiac injury associated with catecholamine release: one-week follow-up study. Crit Care 18:558
Shibuya M, Suzuki Y, Sugita K, Saito I, Sasaki T, Takakura K, Nagata I, Kikuchi H, Takemae T, Hidaka H, Nakashima M (1992) Effect of AT877 on cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Result of a prospective placebo-controlled double blind trial. J Neurosurg 76:571–577
Singer P, Berger MM, Van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C, ESPEN (2009) ESPEN guidelines on parenteral nutrition: intensive care. Clin Nutr 28:387–400
Spetzler RF, McDougall CG, Albuquerque FC, Zabramski JM, Hills NK, Partovi S, Nakaji P, Wallace RC (2013) The Barrow ruptured aneurysm trial: 3-year results. J Neurosurg 119:146–157
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, De Villiers JC (1988) A universal subarachnoid hemorrhage scale: report of a committee of the world federation of neurosurgical societies. J Neurol Neurosurg Psychiatry 51:1457
Tokiyoshi K, Ohnishi T, Nii Y (1991) Efficacy and toxicity of thromboxane synthetase inhibitor for cerebral vasospasm after subarachnoid hemorrhage. Surg Neurol 36:112–118
Touho H, Karasawa J, Shishido H, Morisako T, Yamada K, Shibamoto K (1990) Hypermetabolism in the acute stage of hemorrhagic cerebrovascular disease. J Neurosurg 72:710–714
Weir JB (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109:1–9
Yoshimoto Y, Tanaka Y, Hoya K (2001) Acute systemic inflammatory response syndrome in subarachnoid hemorrhage. Stroke 32:1989–1993
Acknowledgements
We are grateful to Dr. Tetsushi Ogawa of Takasaki General Medical Center for critical comments about nutrition science. We also thank Yoshihiro Kawahake, Masamitsu Hatano, and Yusuke Ogawa of Takasaki General Medical Center for technical support in metabolism measuring.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees of the country of each participating member and with the 1964 Helsinki Declaration and its later amendments or comparable standards.
Informed consent
Informed consent was obtained from all participants included in the study.
Rights and permissions
About this article
Cite this article
Shimauchi-Ohtaki, H., Tosaka, M., Ohtani, T. et al. Systemic metabolism and energy consumption after microsurgical clipping and endovascular coiling for aneurysmal subarachnoid hemorrhage. Acta Neurochir 160, 261–268 (2018). https://doi.org/10.1007/s00701-017-3400-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3400-0