Abstract
Background
We showed that ventriculoperitoneal (VP) shunt and lumboperitoneal (LP) shunt surgeries are beneficial for patients with idiopathic normal pressure hydrocephalus (iNPH) in the Study of Idiopathic Normal Pressure Hydrocephalus on Neurological Improvement (SINPHONI; a multicenter prospective cohort study) and in SINPHONI-2 (a multicenter randomized trial). Although therapeutic efficacy is important, cost-effectiveness analysis is equally valuable.
Methods
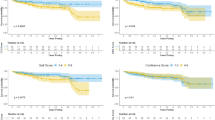
Using both a set of assumptions and using the data from SINPHONI and SINPHONI-2, we estimated the total cost of treatment for iNPH, which consists of medical expenses (e.g., operation fees) and costs to the long-term care insurance system (LCIS) in Japan. Regarding the natural course of iNPH patients, 10% or 20% of patients on each modified Rankin Scale (mRS) show aggravation (aggravation rate: 10% or 20%) every 3 months if the patients do not undergo shunt surgery, as described in a previous report. We performed cost-effectiveness analyses for the various scenarios, calculating the quality-adjusted life year (QALY) and the incremental cost-effective ratio (ICER). Then, based on the definition provided by a previous report, we assessed the cost-effectiveness of shunt surgery for iNPH.
Results
In the first year after shunt surgery, the ICER of VP shunt varies from 29,934 to 40,742 USD (aggravation rate 10% and 20%, respectively) and the ICER of LP shunt varies from 58,346 to 80,392 USD (aggravation rate 10% and 20%, respectively), which indicates that the shunt surgery for iNPH is a cost-effective treatment.
In the 2nd postoperative year, the cost to the LCIS will continue to decrease because of the lasting improvement of the symptoms due to the surgery. The total cost for iNPH patients will show a positive return on investment in as soon as 18 months (VP) and 21 months (LP), indicating that shunt surgery for iNPH is a cost-effective treatment.
Conclusions
Because the total cost for iNPH patients will show a positive return on investment within 2 years, shunt surgery for iNPH is a cost-effective treatment and therefore recommended.
The SINPHONI-2 study was registered with the University Hospital Medical Information Network Clinical Trials registry: UMIN000002730)
SINPHONI was registered with ClinicalTrials.gov, no. NCT00221091.



Similar content being viewed by others
References
Al-Tamimi YZ, Sinha P, Chumas PD, Crimmins D, Drake J, Kestle J, British Pediatric Neurosurgery Group Audit C, Hayward R, Solanki GA, Thomson S, Thorne J (2014) Ventriculoperitoneal shunt 30-day failure rate: a retrospective international cohort study. Neurosurgery 74:29–34
Andren K, Wikkelso C, Tisell M, Hellstrom P (2014) Natural course of idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 85:806–810
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA, Avezaat CJ, de Jong DA, Gooskens RH, Hermans J (1997) Dutch normal-pressure hydrocephalus study: prediction of outcome after shunting by resistance to outflow of cerebrospinal fluid. J Neurosurg 87:687–693
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA, Avezaat CJ, de Jong DA, Gooskens RH, Hermans J (1998) Dutch Normal-Pressure Hydrocephalus Study: randomized comparison of low- and medium-pressure shunts. J Neurosurg 88:490–495
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer JA, Avezaat CJ, de Jong DA, Gooskens RH, Hermans J (1998) Does CSF outflow resistance predict the response to shunting in patients with normal pressure hydrocephalus? Acta neurochirurgica. Supplement 71:331–333
Christensen MC, Morris S (2008) Association between disability measures and short-term health care costs following intracerebral hemorrhage. Neurocrit Care 9:313–318
Egeler-Peerdeman SM, Barkhof F, Walchenbach R, Valk J (1998) Cine phase-contrast MR imaging in normal pressure hydrocephalus patients: relation to surgical outcome. Acta Neurochir Suppl 71:340–342
Fletcher JJ, Kotagal V, Mammoser A, Peterson M, Morgenstern LB, Burke JF (2015) Cost-effectiveness of transfers to centers with neurological intensive care units after intracerebral hemorrhage. Stroke: J Cerebral Circ 46:58–64
Hashimoto M, Ishikawa M, Mori E, Kuwana N, Study of Ioni (2010) Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7:18
Kazui H, Miyajima M, Mori E, Ishikawa M, Investigators S (2015) Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): an open-label randomised trial. Lancet Neurol 14:585–594
Laupacis A, Feeny D, Detsky AS, Tugwell PX (1992) How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ : Can Med Assoc J = J l’Assoc Med Can 146:473–481
Menger RP, Connor DE Jr, Thakur JD, Sonig A, Smith E, Guthikonda B, Nanda A (2014) A comparison of lumboperitoneal and ventriculoperitoneal shunting for idiopathic intracranial hypertension: an analysis of economic impact and complications using the Nationwide Inpatient Sample. Neurosurg Focus 37, E4
Miyajima M, Kazui H, Mori E, Ishikawa M, Sinphoni-Investigators obot (2016) One-year outcome in patients with idiopathic normal-pressure hydrocephalus: comparison of lumboperitoneal shunt to ventriculoperitoneal shunt. Journal of neurosurgery:1–10
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M, Nakajima M, Hashimoto M, Kuriyama N, Tokuda T, Ishii K, Kaijima M, Hirata Y, Saito M, Arai H, Japanese Society of Normal Pressure H (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir 52:775–809
Muraki I, Yamagishi K, Ito Y, Fujieda T, Ishikawa Y, Miyagawa Y, Okada K, Sato S, Kitamura A, Shimamoto T, Tanigawa T, Iso H (2008) Caregiver burden for impaired elderly Japanese with prevalent stroke and dementia under long-term care insurance system. Cerebrovasc Dis 25:234–240
Spagnoli D, Innocenti L, Bello L, Pluderi M, Bacigaluppi S, Tomei G, Gaini SM (2006) Impact of cerebrovascular disease on the surgical treatment of idiopathic normal pressure hydrocephalus. Neurosurgery 59:545–552, discussion 545–552
Toma AK, Papadopoulos MC, Stapleton S, Kitchen ND, Watkins LD (2013) Systematic review of the outcome of shunt surgery in idiopathic normal-pressure hydrocephalus. Acta Neurochir 155:1977–1980
Acknowledgements
This study was a project of the Japanese Society of Normal-Pressure Hydrocephalus. We thank the patients for their participation. We would also like to thank both the people who agreed to participate in this trial and the study contributors.
Author contributions
Conception and design: all authors; acquisition of data: all authors; analysis and interpretation of data: all authors; drafting of the article: Kameda; critically reviewing the article: all authors; revising the manuscript: Kameda; reviewing the submitted version of the manuscript: all authors; statistical analysis: Kameda and Yamada; administrative/technical/material support: all authors; study supervision: Atsuchi, Kimura, Kazui, Miyajima, Mori, Ishikawa, and Date.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
Johnson & Johnson and Nihon Medi-Physics provided financial support to the SINPHONI-2 study [10], and Johnson & Johnson, Nihon Medi-Physics, and Daiichi Pharmaceuticals Co. provided financial support to the SINPHONI study [9]. These sponsors had no role in the design or conduct of this research.
Conflict of Interest
Dr. Miyajima receives clinical and research support from Johnson & Johnson K.K., Inc. (Japan), and Nihon Medi-Physics Co., Ltd. (Japan). Dr. Ishikawa receives lecture fees from Codman and Shurtleff (Japan) and Medtronic Corp. (Japan). Dr. Mori receives honoraria from Johnson & Johnson K.K., Inc.
Dr. Kazui received donations for the 15th Japan Congress of Normal Pressure Hydrocephalus from Johnson & Johnson K.K., Nihon Medi-Physics Co., Ltd., and Medtronic, Inc. and speaker’s honoraria from Johnson & Johnson K.K., Nihon Medi-Physics Co., Ltd., and Medtronic, Inc.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Appendix
Appendix
SINPHONI-2 investigators and centers
M Ishikawa (Rakuwakai Otowa Hospital, Kyoto, Japan); E Mori (Tohoku University Graduate School of Medicine, Sendai, Japan); H Arai and M Miyajima (Juntendo University Graduate School of Medicine, Tokyo, Japan); M Hashimoto (Noto General Hospital, Nanao, Japan); Y Kajimoto (Osaka Medical Collage, Takatsuki, Japan); H Miyake (Nishinomiya Kyoritsu Neurosurgical Hospital, Nishinomiya, Japan); T Nakayama (Hamamatsu Medical Centre, Hamamatsu, Japan); O Hirai (Shinko Hospital, Kobe, Japan); H Kazui and M Takeda (Osaka University Graduate School of Medicine, Suita, Japan); N Kuwana (Tokyo Kyosai Hospital, Tokyo, Japan); C-C Chang (Yokohama Minami Kyosai Hospital, Yokohama, Japan); I Date (Okayama University Graduate School of Medicine, Okayama, Japan); Y Hirata (Kumamoto Takumadai Rehabilitation Hospital, Kumamoto, Japan); M Atsuchi (Atsuchi Neurosurgical Hospital, Kagoshima, Japan); T Okada (Tama-Hokubu Medical Centre, Higashimurayama, Japan); D Kita (Kanazawa University Graduate School of Medicine, Kanazawa, Japan); M Watanabe (Tama-Nanbu Regional Hospital, Tama, Japan); T Kimura (Dohtoh Neurosurgical Hospital, Kitami, Japan); M Kaijima (Megumino Hospital, Eniwa, Japan); S Sunada (Tsudanuma Central General Hospital, Narashino, Japan).
SINPHONI investigators and centers
M Ishikawa and, H Oowaki (Kitano Hospital, Osaka); C-C Chang (Yokohama Minami Kyosai Hospital, Yokohama); M Hashimoto, T Tukada and O Ueki (Noto General Hospital, Nanao); T Takeuchi (Southern Tohoku General Hospital, Koriyama); K Bando (Fujisawa Municipal Hospital, Fujisawa); Y Okamoto (Saiseikai Yahata General Hospital, Kitakyushu); H Murai (Chiba University Graduate School of Medicine, Chiba); Y Kajimoto (Osaka Medical College, Takatuki); E Mori, T Kondo, and K Hiraoka (Tohoku University Graduate School, Sendai); T Okada (Tama Geriatric Medical Center, Tokyo); S Ono and I Date (Okayama University Graduate School of Medicine, Okayama); T Kawaguchi, S Ohkawa and, K Ishii (Hyogo Brain and Heart Center, Himeji); M Miyajima (Juntendo University School of Medicine, Tokyo); A Wachi (Tama Southern Regional Hospital, Tama); S Nomura (Yamaguchi University Graduate School of Medicine, Ube); H Miyake (Nishinomiya Kyoritsu Neurosurgical Hospital, Nishinomiya); O Hirai (Shinko Hospital, Kobe); T Nakayama (Hamamatsu Medical Center, Hamamatu); S Ito (Yokohama City University Medical Center, Yokohama); Y Washimi, K Sako (Nakamura Memorial Hospital, Sapporo); M Bundo (National Center for Geriatrics and Gerontology, Obu); G Tashiro (Maizuru Municipal Hospital, Maizuru); M Murakami and, Y Hirata (Kumamoto Takumadai Hospital, Kumamoto); D Kita (Kanazawa University Graduate School of Medicine, Kanazawa); K Shirota (Higashi Matsuyama Municipal Hospital, Matuyama); T Kondo and E Koumura (Kobe University Graduate School of Medicine, Kobe); H Kazui, N Miyoshi, A Ogino, and Y Kubo (Osaka University Graduate School of Medicine, Suita); Y Nagai, T Daimon, K Matsuyama, and M Fukushima (Translational Research Center, Kobe).
Rights and permissions
About this article
Cite this article
Kameda, M., Yamada, S., Atsuchi, M. et al. Cost-effectiveness analysis of shunt surgery for idiopathic normal pressure hydrocephalus based on the SINPHONI and SINPHONI-2 trials. Acta Neurochir 159, 995–1003 (2017). https://doi.org/10.1007/s00701-017-3115-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3115-2