Abstract
Background
This study aimed to evaluate prevalence and severity of professional burnout in a sample of Lithuanian neurosurgeons and to analyze its personal, interpersonal, and organizational correlates.
Method
Thirty-one out of 79 (response rate 39 %) Lithuanian neurosurgeons participated in the study. Professional burnout was evaluated using the Maslach Burnout Inventory – General Survey. Participants also answered questions about professional stressors, sources of professional dissatisfaction, life–style factors, sickness absenteeism/presenteeism, and professional practice.
Results
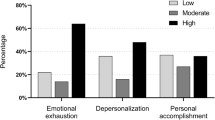
The majority of neurosurgeons were between 41 and 60 years of age (48 %), were married (97 %), had children (84 %). Most neurosurgeons had 20 or more years of professional experience (54.9 %), worked from 41 to 60 h per week (58 %), and performed up to 150 surgeries per year (77.4 %). Eight (26 %) neurosurgeons reported a high level of emotional exhaustion, five (16 %) reported high level of cynicism, and eight (26 %) reported low professional efficacy. Correlation analyses revealed that higher number of surgeries per year, more hours devoted to clinical work, opportunities for professional development, intellectual challenges at work, appreciation by the patients and prestige of the profession were related to lower level of burnout. Greater general workload, unpredictability of the work schedule, lack of necessary technical equipment, dissatisfaction with colleagues, and uncertainty about the future were related to a higher level of burnout.
Conclusions
Burnout was reported by one-quarter of neurosurgeons who chose to participate in the study. Personal, interpersonal, and organizational factors arising while fulfilling professional duties were important correlates of neurosurgeons’ burnout. Due to the moderate response rate, our results should be interpreted with caution. Larger studies evaluating burnout among European neurosurgeons are needed.
Similar content being viewed by others
References
Ahola K, Kivimäki M, Honkonen T, Virtanen M, Koskinen S, Vahtera J, Lönnqvist J (2008) Occupational burnout and medically certified sickness absence: a population-based study of Finnish employees. J Psychosom Res 64(2):185–193
Ahola K, Väänänen A, Koskinen A, Kouvonen A, Shirom A (2010) Burnout as a predictor of all-cause mortality among industrial employees: a 10-year prospective register-linkage study. J Psychosom Res 69(1):51–57
Anagnostopoulos F, Liolios E, Persefonis G, Slater J, Kafetsios K, Niakas D (2012) Physician burnout and patient satisfaction with consultation in primary health care settings: evidence of relationships from a one-with-many design. J Clin Psychol Med Settings 19(4):401–410
Balch CM, Shanafelt T (2010) Combating stress and burnout in surgical practice: a review. Adv Surg 44(1):29–47
Bertges Yost W, Eshelman A, Raoufi M, Abouljoud MS (2005) A national study of burnout among American transplant surgeons. Transplant Proc 37(2):1399–1401
Bria M, Spânu F, Băban A, Dumitraşcu DL (2014) Maslach Burnout Inventory – General Survey: factorial validity and invariance among Romanian healthcare professionals. Burn Res 1(3):103–111
Bunevicius A, Bilskiene D, Macas A, Tamasauskas A (2016) Hemodynamic response during aneurysm clipping surgery among experienced neurosurgeons. Acta Neurochir (Wien) 158(2):221–227
Campbell DA, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ (2001) Burnout among American surgeons. Surgery 130(4):696–702, discussion 702–705
Cappabianca P (2006) Advice for a young neurosurgeon. Surg Neurol 65(1):35–37
Chyi P, Tan M, Robinson G, Jayathissa S, Weatherall M (2014) Coming to work sick: s survey of hospital doctors in New Zealand. N Z Med J 127(1399):23–35
Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P (2014) How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res 14:325. doi:10.1186/1472-6963-14-325
Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL (2015) Burnout among psychiatrists in the Veterans Health Administration. Burn Res 2(4):108–114
Genevičiūtė-Janonienė G, Skučaitė R, Endriulatienė A (2015) Įsipareigijomas organizacijai - darbuotojų profesinio perdegimo rizikos ar saugos veiksnys? [Employees’ organizational commitment - risk or preventive factor in professional burnout at work]. Psichologija (Vilnius Univ) 52:77–90
Gustafsson Sendén M, Løvseth LT, Schenck-Gustafsson K, Fridner A (2013) What makes physicians go to work while sick: a comparative study of sickness presenteeism in four European countries (HOUPE). Swiss Med Wkly 143:w13840. doi:10.4414/smw.2013.13840
Hakanen JJ, Schaufeli WB (2012) Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord 141(2–3):415–424
Halbesleben JRB, Whitman MV, Crawford WS (2014) A dialectical theory of the decision to go to work: bringing together absenteeism and presenteeism. Hum Resour Manag Rev 24(2):177–192
Hansen CD, Andersen JH (2008) Going ill to work: what personal circumstances, attitudes and work-related factors are associated with sickness presenteeism? Soc Sci Med 67(6):956–964
Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, Nykyri E, Aromaa A, Lönnqvist J (2006) The association between burnout and physical illness in the general population: results from the Finnish health 2000 study. J Psychosom Res 61(1):59–66
Kat A, Mallory B, Gilbert JC, Bethel C, Hayes-Jordan AA, Saito JM, Tomita SS, Walsh DS, Shin CE, Wesley JR, Farmer D (2010) State of the practice for pediatric surgery: career satisfaction and concerns. A report from the American Pediatric Surgical Association Task Force on family issues. J Pediatr Surg 45(10):1975–1982
Klein J (2013) Präsentismus, Absentismus und psychosoziale Arbeitsbelastungen bei chirurgisch tätigen Krankenhausärzten [Presenteeism, absenteeism and psychosocial stress at work among German clinicians in surgery]. Das Gesundheitswes 75(10):e139–e148
Klimo P, DeCuypere M, Ragel BT, McCartney S, Couldwell WT, Boop FA (2013) Career satisfaction and burnout among U.S. neurosurgeons: a feasibility and pilot study. World Neurosurg 80(5):e59–e68
Knox ADC, Reddy S, Mema B, DeMoya M, Cilli-Turner E, Harris I (2014) “Back in the day”… what are surgeon bloggers saying about their careers? J Surg Educ 71(1):21–31
Langballe EM, Innstrand ST, Aasland OG, Falkum E (2011) The predictive value of individual factors, work-related factors, and work-home interaction on burnout in female and male physicians: a longitudinal study. Stress Heal 27(1):73–87
Lee RT, Seo B, Hladkyj S, Lovell BL, Schwartzmann L (2013) Correlates of physician burnout across regions and specialties: a meta-analysis. Hum Resour Health 11:48. doi:10.1186/1478-4491-11-48
Mache S, Vitzthum K, Klapp BF, Danzer G (2014) Surgeons’ work engagement: influencing factors and relations to job and life satisfaction. Surgeon 12(4):181–190
Maslach C, Jackson SE (1981) The measurement of experienced burnout. J Organ Behav 2(2):99–113
Maslach C, Leiter MP, Schaufeli WB (2009) Measuring burnout. In: Cartwright C, Cooper CL (eds) The Oxford handbook of organizational well-being. Oxford University Press, Oxford, pp 86–108
McAbee JH, Ragel BT, McCartney S, Jones GM, Michael LM 2nd, DeCuyper M, Cheng JS, Boop FA, Klimo P Jr (2015) Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg 123:161–173
Mikalauskas A, Macas A, Benetis R (2012) Burnout among Lithuanian cardiac surgeons and cardiac anesthesiologists. Medicina (Kaunas) 48(9):478–484
Montgomery A (2014) The inevitability of physician burnout: implications for interventions. Burn Res 1(1):50–56
Pinto A, Faiz O, Bicknell C, Vincent C (2014) Acute traumatic stress among surgeons after major surgical complications. Am J Surg 208(4):642–647
Pit SW, Hansen V (2014) Factors influencing early retirement intentions in Australian rural general practitioners. Occup Med (Lond) 64(4):297–304
Rantanen I, Tuominen R (2011) Relative magnitude of presenteeism and absenteeism and work-related factors affecting them among health care professionals. Int Arch Occup Environ Health 84:225–230
Reulen H-J, Hide RAB, Bettag M, Bodosi M, Cunha E Sa M (2009) A report on neurosurgical workforce in the countries of the EU and associated states. Acta Neurochir 151:715–721
Rhodes SM, Collins SK (2015) The organizational impact of presenteeism. Radiol Manag 37(5):27–32
Schaufeli W, Bakker A, Hoogduin K, Schaap C, Kladler A (2001) On the clinical validity of the Maslach Burnout Inventory and the Burnout Measure. Psychol Health 16:565–582
Schaufeli WB, Greenglass ER (2001) Introduction to special issue on burnout and health. Psychol Health 16(5):501–510
Schauffeli WB, Leiter MP, Maslach C, Jackson SE (1996) MBI-general survey. In: Maslach C, Jackson SE, Leiter MP (eds) Maslach Burnout Inventory manual. Consulting Psychologists Press, Palo Alto, pp 19–26
Schutte N, Toppinen S, Kalimo R, Schaufeli WB (2000) The factorial validity of the Maslach Burnout Inventory-General Survey (MBI-GS) across occupational groups and nations. J Occup Organ Psychol 73:53–66
Stelter K, Theodoraki MN, Becker S, Tsekmistrenko V, Olzowy B, Ledderose G (2015) Specific stressors in endonasal skull base surgery with and without navigation. Eur Arch Otorhinolaryngol 272(3):631–638
Upton D, Mason V, Doran B, Solowiej K, Shiralkar U, Shiralkar S (2012) The experience of burnout across different surgical specialties in the United Kingdom: a cross-sectional survey. Surgery 151(4):493–501
Vijendren A, Yung M, Sanchez J (2014) The ill surgeon: a review of common work-related health problems amongst UK surgeons. Langenbecks Arch Surg 399(8):967–979
Wall M, Schenck-Gustafsson K, Minucci D, Sendén MG, Løvseth LT, Fridner A (2014) Suicidal ideation among surgeons in Italy and Sweden - a cross-sectional study. BMC Psychol 2(1):53. doi:10.1186/s40359-014-0053-0
Acknowledgments
The authors are grateful to Indre Sulskyte for her assistance with data gathering process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pranckeviciene, A., Tamasauskas, A., Deltuva, V.P. et al. Professional burnout and its correlates in Lithuanian neurosurgeons. Acta Neurochir 158, 1437–1445 (2016). https://doi.org/10.1007/s00701-016-2869-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2869-2