Abstract
Background
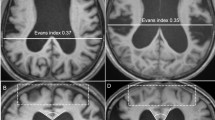
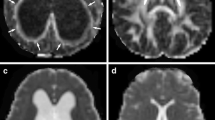
Disproportionately enlarged subarachnoid space hydrocephalus (DESH) findings on MRI were described as a prognostic factor for responsiveness to the treatment of idiopathic normal pressure hydrocephalus (iNPH). Our premise is that DESH could be associated with compression of the cerebral white matter. Microstructural changes can be identified using diffusion tensor imaging (DTI), specifically fractional anisotropy (FA). The aim of this study is to compare FA in iNPH patients with and without DESH and healthy controls.
Methods
We analysed 1.5-T MRI scans of patients fulfilling the criteria of probable or possible iNPH and positive supplementary tests before and after surgery (ventriculo-peritoneal shunt). FA was measured in the anterior and posterior limb of the internal capsule (PLIC) and in the corpus callosum. Patients were divided into the DESH and non-DESH group. These data were also compared to FA values in the control group.
Results
Twenty-seven patients and 24 healthy controls were enrolled. DESH was present in 15 patients and lacking in 12. Twenty-three iNPH patients were shunt responders (85.2 %), and 4 were non-responders (14.8 %). All patients in the DESH group were shunt responders. In the non-DESH group, eight patients were responders (66.7 %). A significant difference between the DESH and non-DESH group was found in the FA of the PLIC. The mean value of FA in the PLIC was 0.72 in the DESH group and 0.66 in the non-DESH group. After the surgery FA decreased in both groups. In the DESH iNPH group FA PLIC decreased to 0.65 and in the non-DESH iNPH group to 0.60. In the healthy controls, the mean FA in the PLIC was 0.58.
Conclusion
DESH on MRI scans is related to a higher FA in the PLIC with a decrease after the surgery. It reflects a more severe compression of the white matter than in non-DESH patients or healthy volunteers. DESH patients had better outcome than non-DESH patients. This study confirmed the importance of DESH as a supportive sign for iNPH.



Similar content being viewed by others
References
Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH (1965) Symptomatic occult hydrocephalus with “normal” cerebrospinal-fluid pressure. A treatable syndrome. N Engl J Med 273:117–126
Hakim S, Adams RD (1965) The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci 2(4):307–327
Bergsneider M, Black PM, Klinge P, Marmarou A, Relkin N (2005) Surgical management of idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3 Suppl):S29–39, discussion ii–v
Klinge P, Marmarou A, Bergsneider M, Relkin N, Black PM (2005) Outcome of shunting in idiopathic normal-pressure hydrocephalus and the value of outcome assessment in shunted patients. Neurosurgery 57(3 Suppl):S40–52, discussion ii–v
Klinge PM, Berding G, Brinker T, Knapp WH, Samii M (1999) A positron emission tomography study of cerebrovascular reserve before and after shunt surgery in patients with idiopathic chronic hydrocephalus. J Neurosurg 91(4):605–609
Momjian S, Owler BK, Czosnyka Z, Czosnyka M, Pena A, Pickard JD (2004) Pattern of white matter regional cerebral blood flow and autoregulation in normal pressure hydrocephalus. Brain J Neurol 127(Pt 5):965–972
Agren-Wilsson A, Eklund A, Koskinen L-OD, Bergenheim AT, Malm J (2005) Brain energy metabolism and intracranial pressure in idiopathic adult hydrocephalus syndrome. J Neurol Neurosurg Psychiatry 76(8):1088–1093
Ishikawa M, Kikuchi H, Taki W, Kobayashi A, Nishizawa S, Yonekura Y, Konishi J (1989) Regional cerebral blood flow and oxygen metabolism in normal pressure hydrocephalus after subarachnoid hemorrhage. Neurol Med Chir (Tokyo) 29(5):382–388
Wikkelsø C, Hellström P, Klinge PM, Tans JTJ, European iNPH Multicentre Study Group (2013) The European iNPH Multicentre Study on the predictive values of resistance to CSF outflow and the CSF Tap Test in patients with idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 84(5):562–568
Kitagaki H, Mori E, Ishii K, Yamaji S, Hirono N, Imamura T (1998) CSF spaces in idiopathic normal pressure hydrocephalus: morphology and volumetry. AJNR Am J Neuroradiol 19(7):1277–1284
Hashimoto M, Ishikawa M, Mori E, Kuwana N, Study of INPH on neurological improvement (SINPHONI) (2010) Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7:18
Le Bihan D, Turner R, Douek P, Patronas N (1992) Diffusion MR imaging: clinical applications. AJR Am J Roentgenol 159(3):591–599
Masutani Y, Aoki S, Abe O, Hayashi N, Otomo K (2003) MR diffusion tensor imaging: recent advance and new techniques for diffusion tensor visualization. Eur J Radiol 46(1):53–66
Assaf Y, Ben-Sira L, Constantini S, Chang LC, Beni-Adani L (2006) Diffusion tensor imaging in hydrocephalus: initial experience. AJNR Am J Neuroradiol 27(8):1717–1724
Uluğ AM, Truong TN, Filippi CG, Chun T, Lee JK, Yang C, Souweidane MM, Zimmerman RD (2003) Diffusion imaging in obstructive hydrocephalus. AJNR Am J Neuroradiol 24(6):1171–1176
Katzman R, Hussey F (1970) A simple constant-infusion manometric test for measurement of CSF absorption. I. Rationale and method. Neurology 20(6):534–544
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3 Suppl):S4–16, discussion ii–v
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke J Cereb Circ 19(5):604–607
Kiefer M, Eymann R, Komenda Y, Steudel WI (2003) A grading system for chronic hydrocephalus. Zentralblatt Für Neurochir 64(3):109–115
Meier U (2002) The grading of normal pressure hydrocephalus. Biomed Tech (Berl) 47(3):54–58
Hattingen E, Jurcoane A, Melber J, Blasel S, Zanella FE, Neumann-Haefelin T, Singer OC (2010) Diffusion tensor imaging in patients with adult chronic idiopathic hydrocephalus. Neurosurgery 66(5):917–924
Jurcoane A, Keil F, Szelenyi A, Pfeilschifter W, Singer OC, Hattingen E (2014) Directional diffusion of corticospinal tract supports therapy decisions in idiopathic normal-pressure hydrocephalus. Neuroradiology 56(1):5–13
Koyama T, Marumoto K, Domen K, Miyake H (2013) White matter characteristics of idiopathic normal pressure hydrocephalus: a diffusion tensor tract-based spatial statistic study. Neurol Med Chir (Tokyo) 53(9):601–608
Kojoukhova M, Koivisto AM, Korhonen R, Remes AM, Vanninen R, Soininen H, Jääskeläinen JE, Sutela A, Leinonen V (2015) Feasibility of radiological markers in idiopathic normal pressure hydrocephalus. Acta Neurochir (Wien) 157(10):1709–1718, discussion 1719
Virhammar J, Laurell K, Cesarini KG, Larsson E-M (2014) Preoperative prognostic value of MRI findings in 108 patients with idiopathic normal pressure hydrocephalus. AJNR Am J Neuroradiol 35(12):2311–2318
Kim MJ, Seo SW, Lee KM, Kim ST, Lee JI, Nam DH, Na DL (2011) Differential diagnosis of idiopathic normal pressure hydrocephalus from other dementias using diffusion tensor imaging. AJNR Am J Neuroradiol 32(8):1496–1503
Hattori T, Yuasa T, Aoki S, Sato R, Sawaura H, Mori T, Mizusawa H (2011) Altered microstructure in corticospinal tract in idiopathic normal pressure hydrocephalus: comparison with Alzheimer disease and Parkinson disease with dementia. AJNR Am J Neuroradiol 32(9):1681–1687
Hattori T, Ito K, Aoki S, Yuasa T, Sato R, Ishikawa M, Sawaura H, Hori M, Mizusawa H (2012) White matter alteration in idiopathic normal pressure hydrocephalus: tract-based spatial statistics study. AJNR Am J Neuroradiol 33(1):97–103
Koyama T, Marumoto K, Domen K, Ohmura T, Miyake H (2012) Diffusion tensor imaging of idiopathic normal pressure hydrocephalus: a voxel-based fractional anisotropy study. Neurol Med Chir (Tokyo) 52(2):68–74
Acknowledgments
This study was supported by grant IGA MZ NT14448-3/2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Ministry of Health of the Czech Republic provided financial support in the form of grant IGA MZ NT14448-3/2013.
The sponsor had no role in the design or conduct of this research.
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
Disproportionately enlarged subarchnoid space hydrocephalus (DESH) was described by the Japanese Society of Normal Pressure Hydrocephalus around 2010. Its guidelines define DESH as iNPH with the specific MRI features of tight high-convexity, the presence of medial subarachnoid spaces and ventriculomegaly. Not all patients presenting with iNPH show the classical picture of DESH. It is reported that the improvement rate after shunting in iNPH patients with DESH is 60 % to 70 %. This raises eyebrows, as a similar figure can be found in many studies in iNPH patients without considering whether they were DESH or non-DESH. On top of this, the fast MRI sequences designed to show pulsatile movement of the CSF (Time-SLIP CSF flow imaging) demonstrate that the CSF moves freely in the subarachnoid spaces below and in the Sylvian fissures; however it does not move in the convexity subarachnoid spaces in patients with DESH. This indicates the presence of flow obstacles in the convexity subarachnoid spaces.
There is no study associating DESH with values of parameters derived from CSF dynamics assessment using the infusion test and/or overnight ICP monitoring. The present finding of an increased fractional anisotropy index in DESH patients versus non-DESH NPH is an original one. However, there is an overlap in FA values in both groups; therefore it is not known how FA may be useful for patient classification. The improvement rate of 100 % versus 66 % should be confirmed in a much larger study than 15:12 patients.
Nevertheless the reported finding may contribute to better understanding of the nature of iNPH.
Marek Czosnyka
Cambridge, UK
Rights and permissions
About this article
Cite this article
Radovnický, T., Adámek, D., Derner, M. et al. Fractional anisotropy in patients with disproportionately enlarged subarachnoid space hydrocephalus. Acta Neurochir 158, 1495–1500 (2016). https://doi.org/10.1007/s00701-016-2861-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2861-x