Abstract
Background
To compare the prognostic value of pulse amplitude on intracranial pressure (ICP) monitoring and disproportionately enlarged subarachnoid space hydrocephalus (DESH) on magnetic resonance imaging (MRI) for predicting surgical benefit after shunt placement in idiopathic normal pressure hydrocephalus (iNPH).
Method
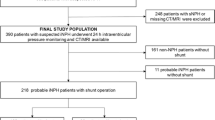
Patients with suspected iNPH were prospectively recruited from a single centre. All patients received preoperative MRI and ICP monitoring. Patients were classified as shunt responders if they had an improvement of one point or more on the NPH score at 1 year post-surgery. The sensitivity, specificity, Youden index, and positive and negative predictive values of the two diagnostic methods were calculated.
Results
Sixty-four of 89 patients clinically improved at 1 year post-surgery and were classed as shunt responders. Positive DESH findings had a sensitivity of 79.4 % and specificity of 80.8 % for predicting shunt responders. Fifty-five of 89 patients had positive DESH findings: 50 of these responded to VP shunt, giving a positive and negative predictive value of 90.9 % and 61.8 %, respectively. Fifty-seven of 89 patients had high ICP pulse amplitude. High ICP pulse amplitude had a sensitivity of 84.4 %, specificity of 88 %, positive predictive value of 94.7 % and negative predictive value of 61.8 % for predicting shunt responders.
Conclusions
Both positive DESH findings and high ICP pulse amplitude support the diagnosis of iNPH and provide additional diagnostic value for predicting shunt-responsive patients; however, high ICP amplitude was more accurate than positive DESH findings, although it is an invasive test.
Similar content being viewed by others
References
Alperin N, Vikingstad EM, Gomez-Anson B, Levin DN (1996) Hemodynamically independent analysis of cerebrospinal fluid and brain motion observed with dynamic phase contrast MRI. Magn Reson Med 35:741–754
Bech-Azeddine R, Waldemar G, Knudsen GM, Høgh P, Bruhn P, Wildschiødtz G, Gjerris F, Paulson OB, Juhler M (2001) Idiopathic normal-pressure hydrocephalus: evaluation and findings in a multidisciplinary memory clinic. Eur J Neurol 8:601–611
Black PM (1980) Idiopathic normal-pressure hydrocephalus. Results of shunting in 62 patients. J Neurosurg 52:371–377
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA, Hermans J (1999) Dutch normal-pressure hydrocephalus study: the role of cerebrovascular disease. J Neurosurg 90:221–226
Czosnyka M, Czosnyka Z, Keong N, Lavinio A, Smielewski P, Momjian S, Schmidt EA, Petrella G, Owler B, Pickard JD (2007) Pulse pressure waveform in hydrocephalus: what it is and what it isn’t. Neurosurg Focus 22:E2
Di Rocco C, Maira G, Rossi GF, Vignati A (1976) Cerebrospinal fluid pressure studies in normal pressure hydrocephalus and cerebral atrophy. Eur Neurol 14:119–128
Eide PK (2006) Intracranial pressure parameters in idiopathic normal pressure hydrocephalus patients treated with ventriculo-peritoneal shunts. Acta Neurochir (Wein) 148:21–29, discussion 29
Eide PK, Brean A (2010) Cerebrospinal fluid pulse pressure amplitude during lumbar infusion in idiopathic normal pressure hydrocephalus can predict response to shunting. Cerebrospinal Fluid Res 7:5
Eide PK, Sorteberg W (2010) Diagnostic intracranial pressure monitoring and surgical management in idiopathic normal pressure hydrocephalus: a 6-year review of 214 patients. Neurosurgery 66:80–91
Enzmann DR, Pelc NJ (1993) Cerebrospinal fluid flow measured by phase-contrast cine MR. AJNR Am J Neuroradiol 14:1301–1307, discussion 1309–10
Golomb J, Wisoff J, Miller DC, Boksay I, Kluger A, Weiner H, Salton J, Graves W (2000) Alzheimer’s disease comorbidity in normal pressure hydrocephalus: prevalence and shunt response. J Neurol Neurosurg Psychiatry 68:778–781
Hashimoto M, Ishikawa M, Mori E, Kuwana N (2010) Study of INPH on neurological improvement (SINPHONI) Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7:18
Holodny AI, George AE, de Leon MJ, Golomb J, Kalnin AJ, Cooper PR (1998) Focal dilation and paradoxical collapse of cortical fissures and sulci in patients with normal-pressure hydrocephalus. J Neurosurg 89:742–747
Höglund M, Tisell M, Wikkelsø C (2001) Incidence of surgery for hydrocephalus in adults surveyed: same number afflicted by hydrocephalus as by multiple sclerosis]. Lakartidningen 98:1681–1685
Kiefer M, Unterberg A (2012) The differential diagnosis and treatment of normal-pressure hydrocephalus. Dtsch Arztebl Int 109:15–25, quiz 26
Kim MJ, Seo SW, Lee KM, Kim ST, Lee JI, Nam DH, Na DL (2011) Differential diagnosis of idiopathic normal pressure hydrocephalus from other dementias using diffusion tensor imaging. AJNR Am J Neuroradiol 32:1496–1503
Kitagaki H, Mori E, Ishii K, Yamaji S, Hirono N, Imamura T (1998) CSF spaces in idiopathic normal pressure hydrocephalus: morphology and volumetry. AJNR Am J Neuroradiol 19:1277–1284
Klassen BT, Ahlskog JE (2011) Normal pressure hydrocephalus: how often does the diagnosis hold water? Neurology 77:1119–1125
Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM (2005) The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery 57:S17–S28, discussion ii–v
Marmarou A, Bergsneider M, Relkin N, Klinge P, Black PM (2005) Development of guidelines for idiopathic normal-pressure hydrocephalus: introduction. Neurosurgery 57:S1–S3, discussion ii–v
Marmarou A, Young HF, Aygok GA, Sawauchi S, Tsuji O, Yamamoto T, Dunbar J (2005) Diagnosis and management of idiopathic normal-pressure hydrocephalus: a prospective study in 151 patients. J Neurosurg 102:987–997
Moore DW, Kovanlikaya I, Heier LA, Raj A, Huang C, Chu K-W, Relkin NR (2012) A pilot study of quantitative MRI measurements of ventricular volume and cortical atrophy for the differential diagnosis of normal pressure hydrocephalus. Neurol Res Int 2012:718150–718156
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M, Nakajima M, Hashimoto M, Kuriyama N, Tokuda T, Ishii K, Kaijima M (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52:775–809
Park E-H, Eide PK, Zurakowski D, Madsen JR (2012) Impaired pulsation absorber mechanism in idiopathic normal pressure hydrocephalus: laboratory investigation. J Neurosurg 117:1189–1196
Sahuquillo J, Rubio E, Codina A, Molins A, Guitart JM, Poca MA, Chasampi A (1991) Reappraisal of the intracranial pressure and cerebrospinal fluid dynamics in patients with the so-called “normal pressure hydrocephalus” syndrome. Acta Neurochir (Wein) 112:50–61
Sasaki M, Honda S, Yuasa T, Iwamura A, Shibata E, Ohba H (2008) Narrow CSF space at high convexity and high midline areas in idiopathic normal pressure hydrocephalus detected by axial and coronal MRI. Neuroradiology 50:117–122
Sæhle T, Eide PK (2015) Association between ventricular volume measures and pulsatile and static intracranial pressure scores in non-communicating hydrocephalus. J Neurol Sci 350:33–39
Thomsen AM, Børgesen SE, Bruhn P, Gjerris F (1986) Prognosis of dementia in normal-pressure hydrocephalus after a shunt operation. Ann Neurol 20:304–310
Vanneste J, Augustijn P, Tan WF, Dirven C (1993) Shunting normal pressure hydrocephalus: the predictive value of combined clinical and CT data. J Neurol Neurosurg Psychiatry 56:251–256
Walchenbach R, Geiger E, Thomeer RTWM, Vanneste JAL (2002) The value of temporary external lumbar CSF drainage in predicting the outcome of shunting on normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 72:503–506
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comment
Despite technical and knowledge improving, the surgical outcomes and the clinical indication to shunting for iNPH have not improved in the last decades. After the well-known multi-center prospective study SHINPHONI of 2010, the neurosurgical community is aware that disproportionately expanded Sylvian fissures alongside with tight high convexity and medial subarachnoid spaces in MRI - also known as disproportionately enlarged subarachnoid space hydrocephalus (DESH) -is very useful for the diagnosis of iNPH, and therefore could predict the efficacy of treatment.
In this manuscript, the Authors report a prospective study involving long-term follow-up of 89 patients with iNPH over a mean period of 46 months in order to compare the prognostic value of DESH and pulse amplitude ICP. One year after shunting 71,9 % of patients had a clinical improvement and could be classified as shunt responders. 62,9 were DESH positive. DESH had a sensitivity and specifity of around 80 %, with a positive predict value of 91 % and negative predictive value of 60 % for discriminating shunt responders. If associated with ICP amplitude the accuracy of predicting shunt responses reaches globally the > 90 %.
A very intriguing issue is the theory, that positive DESH findings may be caused by defective CSF absorption as a result of suprasylvian subarachnoidal block. This question is worthy to be clarified by appropriate research.
The topic is of neurosurgical relevance, and the study well conducted. Overall, the data are convincing that DESH may be useful as a first test for identifying iNPH patients who will respond to a shunt.
Alex Alfieri
Francesco Ferri
Neuruppin, Germany
Rights and permissions
About this article
Cite this article
Garcia-Armengol, R., Domenech, S., Botella-Campos, C. et al. Comparison of elevated intracranial pressure pulse amplitude and disproportionately enlarged subarachnoid space (DESH) for prediction of surgical results in suspected idiopathic normal pressure hydrocephalus. Acta Neurochir 158, 2207–2213 (2016). https://doi.org/10.1007/s00701-016-2858-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2858-5