Abstract
Background
Aneurysmal rebleed is the most dreaded complication following subarachnoid hemorrhage. Being a cause of devastating outcome, the stratification of risk factors can be used to prioritize patients, especially at high volume centers.
Method
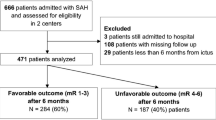
A total of 99 patients with aneurysmal rebleed were analyzed in this study both prospectively and retrospectively from August 2010 to July 2014. In the control group, 100 patients were selected randomly from the patient registry. A total of 25 variables from the demographic, historical, clinical and radiological data were compared and analyzed by univariate and multivariate logistic regression analysis.
Results
Significant independent predictors of aneurysm rebleed were the presence of known hypertension (p = 0.023), diastolic blood pressure of >90 mmHg on admission (p = 0.008); presence of loss of consciousness (p = 0.013) or seizures (p = 0.002) at first ictus; history of warning headaches (p = 0.005); higher Fisher grade (p < 0.001); presence of multiple aneurysms (p = 0.021); irregular aneurysm surface (0.002).
Conclusions
Identification of high risk factors can help in stratifying patients in the high risk group. The risk stratification strategy with early intervention can prevent rebleeds. This in turn may translate into better outcomes of patients with intracranial aneurysms.

Similar content being viewed by others
References
McCormick WF, Nofzinger JD (1965) Saccular intracranial aneurysms: an autopsy study. J Neurosurg 22:155–159
Broderick JP, Brott T, Tomsick T, Miller R, Huster G (1993) Intracerebral hemorrhage more than twice as common as subarachnoid hemorrhage. J Neurosurg 78:188–191
Ingall T, Asplund K, Mahonen M, Bonita R (2000) A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke; J Cereb Circ 31:1054–1061
Linn FH, Rinkel GJ, Algra A, van Gijn J (1996) Incidence of subarachnoid hemorrhage: role of region, year, and rate of computed tomography: a meta-analysis. Stroke; J Cereb Circ 27:625–629
Greenberg M (2006) Handbook of neurosurgery. Thieme, New York
Graf CJ (1971) Prognosis for patients with nonsurgically-treated aneurysms. Analysis of the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. J Neurosurg 35:438–443
Hijdra A, Vermeulen M, van Gijn J, van Crevel H (1987) Rerupture of intracranial aneurysms: a clinicoanatomic study. J Neurosurg 67:29–33
Locksley HB, Sahs AL, Sandler R (1966) Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. 3. Subarachnoid hemorrhage unrelated to intracranial aneurysm and A-V malformation. A study of associated diseases and prognosis. J Neurosurg 24:1034–1056
Steiger HJ, Fritschi J, Seiler RW (1994) Current pattern of in-hospital aneurysmal rebleeds. Analysis of a series treated with individually timed surgery and intravenous nimodipine. Acta Neurochir 127:21–26
Fujii Y, Takeuchi S, Sasaki O, Minakawa T, Koike T, Tanaka R (1996) Ultra-early rebleeding in spontaneous subarachnoid hemorrhage. J Neurosurg 84:35–42
Herrick IA, Gelb AW (1992) Anesthesia for intracranial aneurysm surgery. J Clin Anesth 4:73–85
Sakaki T, Morimoto T, Hoshida T, Kawaguchi S, Nakase H, Fukuzumi A (1999) Rebleeding during transport of patients with a ruptured intracranial aneurysm. J Stroke Cerebrovasc Dis: Off J Nat Stroke Assoc 8:38–41
Beck J, Raabe A, Szelenyi A, Berkefeld J, Gerlach R, Setzer M, Seifert V (2006) Sentinel headache and the risk of rebleeding after aneurysmal subarachnoid hemorrhage. Stroke; J Cereb Circ 37:2733–2737
Naidech AM, Janjua N, Kreiter KT, Ostapkovich ND, Fitzsimmons BF, Parra A, Commichau C, Connolly ES, Mayer SA (2005) Predictors and impact of aneurysm rebleeding after subarachnoid hemorrhage. Arch Neurol 62:410–416
Tanno Y, Homma M, Oinuma M, Kodama N, Ymamoto T (2007) Rebleeding from ruptured intracranial aneurysms in North Eastern Province of Japan. A cooperative study. J Neurolog Sci 258:11–16
Taha AG, Byrne RM, Avgerinos ED, Marone LK, Makaroun MS, Chaer RA (2014) Comparative effectiveness of endovascular versus surgical revascularization for acute lower extremity ischemia. J Vasc Surg
Biller J, Godersky JC, Adams HP Jr (1988) Management of aneurysmal subarachnoid hemorrhage. Stroke; J Cereb Circ 19:1300–1305
Jane JA, Kassell NF, Torner JC, Winn HR (1985) The natural history of aneurysms and arteriovenous malformations. J Neurosurg 62:321–323
Juvela S (1989) Rebleeding from ruptured intracranial aneurysms. Surg Neurol 32:323–326
Kassell NF, Torner JC (1983) Aneurysmal rebleeding: a preliminary report from the Cooperative Aneurysm Study. Neurosurgery 13:479–481
Locksley HB (1966) Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. J Neurosurg 25:321–368
Pakarinen S (1967) Incidence, aetiology, and prognosis of primary subarachnoid haemorrhage. A study based on 589 cases diagnosed in a defined urban population during a defined period. Acta Neurol Scand 43(29):21–28
Rosenorn J, Eskesen V, Schmidt K, Ronde F (1987) The risk of rebleeding from ruptured intracranial aneurysms. J Neurosurg 67:329–332
Vermeulen M, van Gijn J, Hijdra A, van Crevel H (1984) Causes of acute deterioration in patients with a ruptured intracranial aneurysm. A prospective study with serial CT scanning. J Neurosurg 60:935–939
Arima H, Anderson C, Omae T, Woodward M, Hata J, Murakami Y, Macmahon S, Neal B, Chalmers J, Group PC (2011) Effects of blood pressure lowering on major vascular events among patients with isolated diastolic hypertension: the perindopril protection against recurrent stroke study (PROGRESS) trial. Stroke; J Cereb Circ 42:2339–2341
Arima H, Chalmers J (2011) PROGRESS: prevention of recurrent stroke. J Clin Hypertens 13:693–702
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ, Joint National Committee on Prevention DE, Treatment of High Blood Pressure. National Heart L, Blood I, National High Blood Pressure Education Program Coordinating C (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42:1206–1252
Fang XH, Zhang XH, Yang QD, Dai XY, Su FZ, Rao ML, Wu SP, Du XL, Wang WZ, Li SC (2006) Subtype hypertension and risk of stroke in middle-aged and older Chinese: a 10-year follow-up study. Stroke; J Cereb Circ 37:38–43
Kelly TN, Gu D, Chen J, Huang JF, Chen JC, Duan X, Wu X, Yau CL, Whelton PK, He J (2008) Hypertension subtype and risk of cardiovascular disease in Chinese adults. Circulation 118:1558–1566
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B, Management of Arterial Hypertension of the European Society of H, European Society of C (2007) 2007 guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the european society of hypertension (ESH) and of the european society of cardiology (ESC). J Hypertens 25:1105–1187
Starke RM, Connolly ES Jr, Participants in the International Multi-Disciplinary Consensus Conference on the Critical Care Management of Subarachnoid H (2011) Rebleeding after aneurysmal subarachnoid hemorrhage. Neurocritical Care 15:241–246
Cong W, Zhongxin Z, Tiangui L, Zhang Y, Min H, Chao Y (2012) Risk factors for rebleeding of aneurysmal subarachnoid hemorrhage based on the analysis of on-admission information. Turkish Neurosurg 22:675–681
Ohkuma H, Tsurutani H, Suzuki S (2001) Incidence and significance of early aneurysmal rebleeding before neurosurgical or neurological management. Stroke; J Cereb Circ 32:1176–1180
Reynolds ASC (1980) Bleeding Patterns from ruptured intracranial aneurysms: an autopsy series of 205 patients. Surg Neurol 15:4
Nibbelink DW, Torner JC, Henderson WG (1975) Intracranial aneurysms and subarachnoid hemorrhage. A cooperative study Antifibrinolytic therapy in recent onset subarachnoid hemorrhage. Stroke; J Cereb Circ 6:622–629
Beck J, Rohde S, Berkefeld J, Seifert V, Raabe A (2006) Size and location of ruptured and unruptured intracranial aneurysms measured by 3-dimensional rotational angiography. Surg Neurol 65:18–25, discussion 25-17
Guo LM, Zhou HY, Xu JW, Wang Y, Qiu YM, Jiang JY (2011) Risk factors related to aneurysmal rebleeding. World Neurosurg 76:292–298, discussion 253-294
Cha KC, Kim JH, Kang HI, Moon BG, Lee SJ, Kim JS (2010) Aneurysmal rebleeding : factors associated with clinical outcome in the rebleeding patients. J Korean Neurosurg Soc 47:119–123
Mehta V, Holness RO, Connolly K, Walling S, Hall R (1996) Acute hydrocephalus following aneurysmal subarachnoid hemorrhage. The Canadian journal of neurological sciences. J Can Sci Neurol 23:40–45
Rajshekhar V, Harbaugh RE (1992) Results of routine ventriculostomy with external ventricular drainage for acute hydrocephalus following subarachnoid haemorrhage. Acta Neurochir 115:8–14
Pare L, Delfino R, Leblanc R (1992) The relationship of ventricular drainage to aneurysmal rebleeding. J Neurosurg 76:422–427
Locksley HB (1966) Natural history of subarachnoid hemorrhage, intracranial aneurysms and arteriovenous malformations. Based on 6368 cases in the cooperative study. J Neurosurg 25:219–239
Lanzino G, Kassell NF, Germanson TP, Kongable GL, Truskowski LL, Torner JC, Jane JA (1996) Age and outcome after aneurysmal subarachnoid hemorrhage: why do older patients fare worse? J Neurosurg 85:410–418
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patient-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of NIMHANS (National Institute of Mental health and Neuro Sciences, Bengaluru, Karnataka, India) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
Comment
Spontaneous subarachnoid hemorrhage (SAH), which is most frequently due to aneurysmal rupture, is a significant source of morbidity and mortality. However, the continued evolution of both open and endovascular treatment modalities are actively improving the expected outcome of this disease process. As the authors point out, though, aneurysmal rebleed prior to treatment is both largely unpredictable and clinically devastating to the patient. On both retrospective and prospective review of their own patient series, the authors attempt to identify the risk factors that portend a higher likelihood of rebleed before a patient can receive treatment. By examining a variety of demographic, comorbid and radiographic characteristics, the authors are able to identify clinical variables that reliably identify those patients at a higher risk of early rebleed. They further posit that following these clinical variables in practice may allow for more urgent treatment of high-risk cases and therefore further improve patient outcomes.
The authors make a valiant attempt to more thoroughly delineate the risk factors that predispose patients to this devastating complication of aneurysmal SAH. While the authors attempt to clarify which patients should be targeted to early therapy, the interval at which treatment should be instituted remains ambiguous. It is well documented in the literature that the highest risk of aneurysmal rebleed is in the first 24 h after initial hemorrhage (1–3). The patients in this series vary widely in their times from initial bleeding event to presentation, transfer and eventual treatment (24 to 72 h). Therefore, it would be of more clinical relevance to explore these intervals scrupulously in the context of the risk factors discussed. If patients with risk factors that predispose them to rebleed are also at risk of earlier rebleed, this assists in designing treatment algorithms. Without this analysis, the presence of risk factors is identified and patients are placed in a ‘high risk’ class, but not treated differently from any other aneurysmal rupture. This timing of therapy is the crucial variable that has the most potential impact on patient outcome.
Previous works have attempted to delineate the risk factors for both aneurysmal rupture and rebleed (2, 4, 5). The authors admit as much and compare their sometimes contradictory results with previous work. While this is meaningful to some extent and helps to better define the ‘high-risk’ group, it takes the focus off of the proposed novel factors the authors suggest. The authors do their best, in the discussion, to spend less time focusing on previously documented risks and instead examining if their factors of interest (diastolic hypertension, seizure, LOC, warning headache, etc.) have an additive effect with known risks or impart a higher clinical risk.
The data presented highlight several interesting points regarding the discord between the existing data and the management of SAH. The authors and others cited focus on the highest risk of rebleed being in the first 24 h. The authors then point out that a minority of patients even arrive at their tertiary care center within 24 h of hemorrhage (<20 %), and few of these patients are treated in this time period (35 %). The data presented herein and the current treatment data call for change in the way SAH patients are prioritized, transferred to properly equipped facilities and treated promptly.
The authors are to be commended for their careful, diligent examination of the risk factors that increase the likelihood of aneurysmal rebleed prior to treatment. As we acquire insight into aneurysmal rebleed, its risk factors and the appropriate timing of definitive treatment, this paper holds the potential to serve as a framework to utilize for patient prioritization.
References
1. Pare L, Delfino R, Leblanc R. The relationship of ventricular drainage to aneurysmal rebleeding. Journal of Neurosurgery. 1992;76(3):422–7.
2. Kaptain GJ, Lanzino G, Kassell NF. Subarachnoid haemorrhage: epidemiology, risk factors, and treatment options. Drugs Aging. 2000;17(3):183–99.
3. Robbert M, Hoogmoed J, van Straaten HA, Coert BA, Peter Vandertop W, Verbaan D. Time intervals from aneurysmal subarachnoid hemorrhage to treatment and factors contributing to delay. J Neurol. 2014;261(3):473–9.
4. Hillman J, Fridriksson S, Nilsson O, Yu Z, Saveland H, Jakobsson KE. Immediate administration of tranexamic acid and reduced incidence of early rebleeding after aneurysmal subarachnoid hemorrhage: a prospective randomized study. Journal of Neurosurgery. 2002;97(4):771–8.
5. Juvela S. Rebleeding from ruptured intracranial aneurysms. Surg Neurol. 1989;32(5):323–6.
Drew Spencer, Christopher M. Loftus
Illinois, USA
Rights and permissions
About this article
Cite this article
Solanki, C., Pandey, P. & Rao, K.V.L.N. Predictors of aneurysmal rebleed before definitive surgical or endovascular management. Acta Neurochir 158, 1037–1044 (2016). https://doi.org/10.1007/s00701-016-2784-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2784-6