Abstract
Purpose
Pancreatoduodenectomy (PD) is a highly invasive procedure. Intra-abdominal infections and pancreatic fistulas are strongly correlated complications. In the present study, we identified the risk factors for postoperative early drain colonization (POEDC) and established a perioperative management strategy.
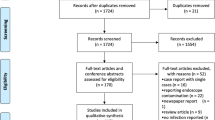
Methods
A total of 205 patients who underwent pancreatoduodenectomy were included in the study. POEDC was defined as a positive drain fluid culture before postoperative day (POD) 4. We retrospectively investigated the correlation between POEDC, postoperative outcomes, and clinical factors.
Results
POEDC was observed in 26 patients (12.6%) with poor postoperative outcomes, including pancreatic fistulas (P < 0.001). A multivariate analysis demonstrated a correlation between these postoperative outcomes and the age (P = 0.002), body mass index (BMI) (P = 0.002), procalcitonin (PCT) level (P < 0.001), and drain amylase level on POD 1 (P = 0.032). Enterococcus was detected most frequently, being found in 15 patients.
Conclusion
We observed a strong correlation between POEDC and poor postoperative outcomes. The BMI, age, and PCT and drain amylase level on POD 1 should be considered POEDC risk factors, with the need to propose an antibiotic perioperative strategy. POEDC control may represent the key to improving postoperative outcomes after PD.


Similar content being viewed by others
References
Adam U, Makowiec F, Riediger H, Schareck WD, Benz S, Hopt UT. Risk factors for complications after pancreatic head resection. Am J Surg. 2004;187:201–8. https://doi.org/10.1016/j.amjsurg.2003.11.004.
Grikyte I, Ignatavicius P. Postoperative hypophosphatemia as a prognostic factor for postoperative pancreatic fistula: a systematic review. Medicina (Kaunas). 2023;59:274. https://doi.org/10.3390/medicina59020274.
Mintziras I, Maurer E, Kanngiesser V, Bartsch DK. C-reactive protein and drain amylase accurately predict clinically relevant pancreatic fistula after partial pancreaticoduodenectomy. Int J Surg. 2020;76:53–8. https://doi.org/10.1016/j.ijsu.2020.02.025.
He C, Zhang Y, Li L, Zhao M, Wang C, Tang Y. Risk factor analysis and prediction of postoperative clinically relevant pancreatic fistula after distal pancreatectomy. BMC Surg. 2023;23:5. https://doi.org/10.1186/s12893-023-01907-w.
Fukami Y, Saito T, Osawa T, Komatsu S, Sano T. Blumgart anastomosis with polyglycolic acid felt reduces the incidence of pancreatic fistula after pancreaticoduodenectomy: a propensity score analysis. Ann Gastroenterol Surg. 2022;6:880–6. https://doi.org/10.1002/ags3.12598.
Fujii T, Sugimoto H, Yamada S, Kanda M, Suenaga M, Takami H, et al. Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg. 2014;18:1108–15. https://doi.org/10.1007/s11605-014-2523-3.
Nagakawa Y, Matsudo T, Hijikata Y, Kikuchi S, Bunso K, Suzuki Y, et al. Bacterial contamination in ascitic fluid is associated with the development of clinically relevant pancreatic fistula after pancreatoduodenectomy. Pancreas. 2013;42:701–6. https://doi.org/10.1097/MPA.0b013e31826d3a41.
Kawai M, Okada KI, Miyazawa M, Kitahata Y, Motobayashi H, Ueno M, et al. Positive drain fluid culture on postoperative day 1 predicts clinically relevant pancreatic fistula in early drain removal with higher drain fluid amylase after pancreaticoduodenectomy. Surgery. 2023;173:511–20. https://doi.org/10.1016/j.surg.2022.10.008.
Kent TS, Sachs TE, Callery MP, Vollmer CM Jr. The burden of infection for elective pancreatic resections. Surgery. 2013;153:86–94. https://doi.org/10.1016/j.surg.2012.03.026.
Kondo K, Chijiiwa K, Ohuchida J, Kai M, Fujii Y, Otani K, et al. Selection of prophylactic antibiotics according to the microorganisms isolated from surgical site infections (SSIs) in a previous series of surgeries reduces SSI incidence after pancreaticoduodenectomy. J Hepato-Bil Pancreat Sci. 2013;20:286–93. https://doi.org/10.1007/s00534-012-0515-9.
Pretzsch E, Heim A, Heiliger C, Pretzsch CM, Ilmer M, Weniger M, et al. Specific intraoperative antibiotic therapy abrogates the negative effect of biliary contamination on the Comprehensive Complication Index after pancreatic head resection. Surgery. 2022;171:1642–51. https://doi.org/10.1016/j.surg.2021.10.022.
Kone LB, Torres C, Banulescu M, Maker VK, Maker AV. Perioperative broad-spectrum antibiotics are associated with decreased surgical site infections compared to 1st–3rd generation cephalosporins after open pancreaticoduodenectomy in patients with jaundice or a biliary stent. Ann Surg. 2022;275:1175–83. https://doi.org/10.1097/SLA.0000000000004216.
Friedman ND, Temkin E, Carmeli Y. The negative impact of antibiotic resistance. Clin Microbiol Infect. 2016;22:416–22. https://doi.org/10.1016/j.cmi.2015.12.002.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152:784–91. https://doi.org/10.1001/jamasurg.2017.0904.
Ban KA, Minei JP, Laronga C, Harbrecht BG, Jensen EH, Fry DE, et al. American College of Surgeons and Surgical Infection Society: Surgical site infection guidelines, 2016 update. J Am Coll Surg. 2017;224:59–74. https://doi.org/10.1016/j.jamcollsurg.2016.10.029.
Sano S, Sugiura T, Kawamura I, Okamura Y, Ito T, Yamamoto Y, et al. Third-generation cephalosporin for antimicrobial prophylaxis in pancreatoduodenectomy in patients with internal preoperative biliary drainage. Surgery. 2019;165:559–64. https://doi.org/10.1016/j.surg.2018.09.011.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
McMillan MT, Malleo G, Bassi C, Allegrini V, Casetti L, Drebin JA, et al. Multicenter, prospective trial of selective drain management for pancreatoduodenectomy using risk stratification. Ann Surg. 2017;265:1209–18. https://doi.org/10.1097/SLA.0000000000001832.
Belmouhand M, Krohn PS, Svendsen LB, Henriksen A, Hansen CP, Achiam MP. The occurrence of Enterococcus faecium and faecalis Is significantly associated with anastomotic leakage after pancreaticoduodenectomy. Scand J Surg. 2018;107:107–13. https://doi.org/10.1177/1457496917731188.
Sato N, Kimura T, Kenjo A, Kofunato Y, Okada R, Ishigame T, et al. Early intra-abdominal infection following pancreaticoduodenectomy: associated factors and clinical impact on surgical outcome. Fukushima J Med Sci. 2020;66:124–32. https://doi.org/10.5387/fms.2020-11.
Ciprani D, Capretti G, Sorrentino M, Gramellini M, Famularo S, Casari E, et al. Clinical usefulness of routinely performed drain fluid cultures after pancreaticoduodenectomy. A new ally to predict patients’ outcomes? Pancreatology. 2023. https://doi.org/10.1016/j.pan.2023.12.013.
Sourrouille I, Gaujoux S, Lacave G, Bert F, Dokmak S, Belghiti J, et al. Five days of postoperative antimicrobial therapy decreases infectious complications following pancreaticoduodenectomy in patients at risk for bile contamination. HPB (Oxford). 2013;15:473–80. https://doi.org/10.1111/hpb.12012.
Okamura K, Tanaka K, Miura T, Nakanishi Y, Noji T, Nakamura T, et al. Randomized controlled trial of perioperative antimicrobial therapy based on the results of preoperative bile cultures in patients undergoing biliary reconstruction. J Hepato-Bil Pancreat Sci. 2017;24:382–93. https://doi.org/10.1002/jhbp.453.
Pham H, Chen A, Nahm CB, Lam V, Pang T, Richardson AJ. The role of targeted versus standard antibiotic prophylaxis in pancreatoduodenectomy in reducing postoperative infectious complications: a systematic review and meta-analysis. Ann Surg. 2022;275:315–23. https://doi.org/10.1097/SLA.0000000000004816.
Maatman TK, Weber DJ, Qureshi B, Ceppa EP, Nakeeb A, Schmidt CM, et al. Does the microbiology of Bactibilia drive postoperative complications after pancreatoduodenectomy? J Gastrointest Surg. 2020;24:2544–50. https://doi.org/10.1007/s11605-019-04432-5.
Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, et al. The surgical infection society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017;18:1–76. https://doi.org/10.1089/sur.2016.261.
Kaneko K, Okamoto R, Nakano R, Kawakami S, Inoue M. Gene mutations responsible for overexpression of AmpC beta-lactamase in some clinical isolates of Enterobacter cloacae. J Clin Microbiol. 2005;43:2955–8. https://doi.org/10.1128/JCM.43.6.2955-2958.2005.
Becker KL, Nylén ES, White JC, Müller B, Snider RH Jr. Clinical review 167: Procalcitonin and the calcitonin gene family of peptides in inflammation, infection, and sepsis: a journey from calcitonin back to its precursors. J Clin Endocrinol Metab. 2004;89:1512–25. https://doi.org/10.1210/jc.2002-021444.
Hata T, Mizuma M, Motoi F, Hayashi H, Ishida M, Ohtsuka H, et al. Serum procalcitonin as an early diagnostic marker of severe postoperative complications after elective pancreaticoduodenectomy. J Hepato-Bil Pancreat Sci. 2020;27:767–75. https://doi.org/10.1002/jhbp.809.
Veillette G, Dominguez I, Ferrone C, Thayer SP, McGrath D, Warshaw AL, et al. Implications and management of pancreatic fistulas following pancreaticoduodenectomy: the Massachusetts General Hospital experience. Arch Surg. 2008;143:476–81. https://doi.org/10.1001/archsurg.143.5.476.
You Y, Han IW, Choi DW, Heo JS, Ryu Y, Park DJ, et al. Nomogram for predicting postoperative pancreatic fistula. HPB (Oxford). 2019;21:1436–45. https://doi.org/10.1016/j.hpb.2019.03.351.
Bassi C, Molinari E, Malleo G, Crippa S, Butturini G, Salvia R, et al. Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Ann Surg. 2010;252:207–14. https://doi.org/10.1097/SLA.0b013e3181e61e88.
McMillan MT, Malleo G, Bassi C, Butturini G, Salvia R, Roses RE, et al. Drain management after pancreatoduodenectomy: Reappraisal of a prospective randomized trial using risk stratification. J Am Coll Surg. 2015;221:798–809. https://doi.org/10.1016/j.jamcollsurg.2015.07.005.
Funding
This study did not receive grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Watanabe, A., Harimoto, N., Araki, K. et al. Perioperative pancreaticoduodenectomy management strategy focusing on postoperative early drain colonization. Surg Today (2024). https://doi.org/10.1007/s00595-024-02810-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02810-4