Abstract
Purpose
Chronic lung allograft dysfunction (CLAD) is a known long-term fatal disorder after lung transplantation. In this study, we evaluated the CLAD classification of the International Society for Heart and Lung Transplantation (ISHLT) for living-donor lobar lung transplantation (LDLLT).
Methods
We conducted a single-center retrospective review of data from 73 patients who underwent bilateral LDLLT between 1998 and 2019. Factors related to opacity on computed tomography (CT) and restriction on pulmonary function tests (PFTs) were also analyzed.
Results
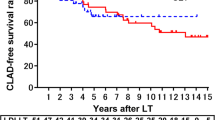
Overall, 26 (36%) patients were diagnosed with CLAD, including restrictive allograft syndrome (RAS), n = 10 (38.5%); bronchiolitis obliterans syndrome (BOS), n = 8 (30.8%); mixed, n = 1 (3.8%); undefined, n = 2 (7.7%); and unclassified, n = 5 (19.2%). The 5-year survival rate after the CLAD onset was 60.7%. The survival of patients with BOS was significantly better than that of patients with RAS (p = 0.012). In particular, patients with restriction on PFT had a significantly worse survival than those without restriction (p = 0.001).
Conclusions
CLAD after bilateral LDLLT does not have a major impact on the recipient survival, especially in patients with BOS. Restriction on PFT may predict a particularly poor prognosis in patients with CLAD after bilateral LDLLT.






Similar content being viewed by others
References
Verleden GM, Glanville AR, Lease ED, Fisher AJ, Calabrese F, Corris PA, et al. Chronic lung allograft dysfunction: definition, diagnostic criteria, and approaches to treatment-a consensus report from the pulmonary council of the ISHLT. J Heart Lung Transpl. 2019;38:493–503.
Cooper JD, Billingham M, Egan T, Hertz MI, Higenbottam T, Lynch J, et al. A working formulation for the standardization of nomenclature and for clinical staging of chronic dysfunction in lung allografts international society for heart and lung transplantation. J Heart Lung Transpl. 1993;12:713–6.
Sato M, Waddell TK, Wagnetz U, Roberts HC, Hwang DM, Haroon A, et al. Restrictive allograft syndrome (RAS): a novel form of chronic lung allograft dysfunction. J Heart Lung Transpl. 2011;30:735–42.
Levy L, Huszti E, Renaud-Picard B, Berra G, Kawashima M, Takahagi A, et al. Risk assessment of chronic lung allograft dysfunction phenotypes: Validation and proposed refinement of the 2019 international society for heart and lung transplantation classification system. J Heart Lung Transpl. 2020;39:761–70.
Sugimoto S, Yamamoto H, Kurosaki T, Otani S, Okazaki M, Yamane M, et al. Impact of chronic lung allograft dysfunction, especially restrictive allograft syndrome, on the survival after living-donor lobar lung transplantation compared with cadaveric lung transplantation in adults: a single-center experience. Surg Today. 2019;49:686–93.
Eba J, Nakamura K. Overview of the ethical guidelines for medical and biological research involving human subjects in Japan. Jpn J Clin Oncol. 2022;52:539–44.
Glanville AR, Verleden GM, Todd JL, Benden C, Calabrese F, Gottlieb J, et al. Chronic lung allograft dysfunction: Definition and update of restrictive allograft syndrome-a consensus report from the pulmonary council of the ISHLT. J Heart Lung Transpl. 2019;38:483–92.
Yamamoto H, Sugimoto S, Soh J, Shiotani T, Miyoshi K, Otani S, et al. The prognostic nutritional index is correlated negatively with the lung allocation score and predicts survival after both cadaveric and living-donor lobar lung transplantation. Surg Today. 2021;51:1610–8.
Date H. Living-related lung transplantation. J Thorac Dis. 2017;9:3362–71.
Daud SA, Yusen RD, Meyers BF, Chakinala MM, Walter MJ, Aloush AA, et al. Impact of immediate primary lung allograft dysfunction on bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2007;175:507–13.
Miyamoto E, Chen F, Aoyama A, Sato M, Yamada T, Date H. Unilateral chronic lung allograft dysfunction is a characteristic of bilateral living-donor lobar lung transplantation. Eur J Cardiothorac Surg. 2015;48:463–9.
Yamada Y, Langner T, Inci I, Benden C, Schuurmans M, Weder W, et al. Impact of human leukocyte antigen mismatch on lung transplant outcome. Interact Cardiovasc Thorac Surg. 2018;26:859–64.
Yamamoto H, Sugimoto S, Kurosaki T, Miyoshi K, Otani S, Okazaki M, et al. Lung perfusion scintigraphy to detect chronic lung allograft dysfunction after living-donor lobar lung transplantation. Sci Rep. 2020;10:10595.
Yamane M, Date H, Okazaki M, Toyooka S, Aoe M, Sano Y. Long-term improvement in pulmonary function after living donor lobar lung transplantation. J Heart Lung Transpl. 2007;26:687–92.
Woodrow JP, Shlobin OA, Barnett SD, Burton N, Nathan SD. Comparison of bronchiolitis obliterans syndrome to other forms of chronic lung allograft dysfunction after lung transplantation. J Heart Lung Transpl. 2010;29:1159–64.
Peräkylä LH, Raivio PM, Kesävuori RI, Piilonen AK, Stark CK, Halme MK, et al. Chronic lung allograft dysfunction subtype analysis by computed tomography volumetry. Clin Transpl. 2022;36:e14507.
Saito M, Chen-Yoshikawa TF, Nakamoto Y, Kayawake H, Tokuno J, Ueda S, et al. Unilateral chronic lung allograft dysfunction assessed by biphasic computed tomographic volumetry in bilateral living-donor lobar lung transplantation. Transpl Direct. 2018;4:e398.
Brun AL, Chabi ML, Picard C, Mellot F, Grenier PA. Lung transplantation: ct assessment of chronic lung allograft dysfunction (CLAD). Diag (Basel). 2021;11:817.
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing.
Author information
Authors and Affiliations
Contributions
Participated in research design: KM, SO, SS, Participated in the writing of the paper: KM, SO, KS, KS, KM, HY, MO, ST, Participated in the performance of the research: KM, SO, HY, Participated in the data analysis: KM, SO, KH, ST.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsubara, K., Otani, S., Yamamoto, H. et al. Restrictive allograft dysfunction rather than bronchiolitis obliterans syndrome had a major impact on the overall survival after living-donor lobar lung transplantation. Surg Today 54, 317–324 (2024). https://doi.org/10.1007/s00595-023-02729-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02729-2