Abstract
Purpose
Acute liver failure is a life-threatening condition for which ABO-incompatible living donor liver transplantation (ABOi-LDLT) is sometimes the only life-saving treatment option. We reviewed a single-center experience of adult ABOi-LDLT treatment for acute liver failure (ALF).
Methods
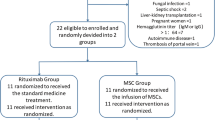
Preoperative treatment, immune indices (B cell marker, anti-donor blood-type antibody), and postoperative outcomes were compared between ALF and non-ALF groups.
Results
There were 5 and 33 patients in the ALF and non-ALF groups, respectively. The ALF group received higher doses of steroids, underwent more rounds of plasma exchange (PE), and underwent transplantation for ALF with a shorter interval following preoperative rituximab (RTx) administration (median: 2 vs 13 days; P < 0.05) than the non-ALF group. Preoperatively, CD19-positive lymphocytes in the peripheral blood were sufficiently depleted in all of the non-ALF group patients, whereas they were poorly depleted in the ALF group. Postoperatively, neither group suffered anti-donor blood-type antibody titer rebound or antibody-mediated rejection. The ALF group had a comparable 5-year survival rate to the non-ALF group (80.0% vs 77.9%).
Conclusions
Despite the delayed preoperative administration of RTx, the ALF group showed an uneventful immunological response and acceptable long-term survival rate. Thus, ABOi-LDLT seems a viable treatment option for ALF.



Similar content being viewed by others
Data Availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
Tanabe M, Shimazu M, Wakabayashi G, Hoshino K, Kawachi S, Kadomura T, et al. Intraportal infusion therapy as a novel approach to adult ABO-incompatible liver transplantation. Transplantation. 2002;73(12):1959–61.
Kawagishi N, Satoh K, Enomoto Y, Akamatsu Y, Sekiguchi S, Fukumori T, et al. New strategy for ABO-incompatible living donor liver transplantation with anti-CD20 antibody (rituximab) and plasma exchange. Transplant Proc. 2005;37(2):1205–6.
Usui M, Isaji S, Mizuno S, Sakurai H, Uemoto S. Experiences and problems pre-operative anti-CD20 monoclonal antibody infusion therapy with splenectomy and plasma exchange for ABO-incompatible living-donor liver transplantation. Clin Transplant. 2007;21(1):24–31.
Egawa H, Teramukai S, Haga H, Tanabe M, Fukushima M, Shimazu M. Present status of ABO-incompatible living donor liver transplantation in Japan. Hepatology. 2008;47(1):143–52.
Uchiyama H, Mano Y, Taketomi A, Soejima Y, Yoshizumi T, Ikegami T, et al. Kinetics of anti-blood type isoagglutinin titers and B lymphocytes in ABO-incompatible living donor liver transplantation with rituximab and plasma exchange. Transplantation. 2011;92(10):1134–9.
Tanabe M, Kawachi S, Obara H, Shinoda M, Hibi T, Kitagawa Y, et al. Current progress in ABO-incompatible liver transplantation. Eur J Clin Invest. 2010;40(10):943–9.
Umeshita K, Eguchi S, Egawa H, Haga H, Kasahara M, Kokudo N, et al. Liver transplantation in Japan: Registry by the Japanese Liver Transplantation Society. Hepatol Res. 2019;49(9):964–80.
Sharma P, Schaubel DE, Gong Q, Guidinger M, Merion RM. End-stage liver disease candidates at the highest model for end-stage liver disease scores have higher wait-list mortality than status-1A candidates. Hepatology. 2012;55(1):192–8.
Kishida N, Shinoda M, Itano O, Obara H, Kitago M, Hibi T, et al. Increased incidence of thrombotic microangiopathy after ABO-incompatible living donor liver transplantation. Ann Transplant. 2016;21:755–64.
Wakabayashi T, Shinoda M, Obara H, Kitago M, Yagi H, Abe Y, et al. Decreased incidence of acute cellular rejection in low-muscle-mass recipients after living-donor liver transplantation. Transplant Proc. 2018;50(10):3626–34.
Abe K, Shinoda M, Uno S, Obara H, Kitago M, Abe Y, et al. Invasive pulmonary aspergillosis after liver transplantation: lessons from successfully treated cases and review of the literature. Surg Today. 2021;51(8):1361–70.
Farges O, Kalil AN, Samuel D, Saliba F, Arulnaden JL, Debat P, et al. The use of ABO-incompatible grafts in liver transplantation: a life-saving procedure in highly selected patients. Transplantation. 1995;59(8):1124–33.
Ikegami T, Taketomi A, Soejima Y, Yoshizumi T, Uchiyama H, Harada N, et al. Rituximab, IVIG, and plasma exchange without graft local infusion treatment: a new protocol in ABO incompatible living donor liver transplantation. Transplantation. 2009;88(3):303–7.
Horikoshi Y, Itoh H, Kikuchi S, Uchida T, Suzuki K, Sugihara K, et al. Successful living donor liver transplantation for fulminant hepatic failure that manifested immediately after cesarean delivery. Asaio J. 2012;58(2):174–6.
Yasuda M, Ikegami T, Imai D, Wang H, Bekki Y, Itoh S, et al. The changes in treatment strategies in ABOi living donor liver transplantation for acute liver failure. J Med Invest. 2015;62(3–4):184–7.
Lee B, Cho JY, Han HS, Yoon YS, Lee HW, Lee JS, et al. Long-term outcomes of emergency ABO-incompatible living donor liver transplantation using a modified desensitization protocol for highly sensitized patients with acute liver failure: a case report. Ann Hepatobiliary Pancreat Surg. 2021;25(4):571–4.
Egawa H, Teramukai S, Haga H, Tanabe M, Mori A, Ikegami T, et al. Impact of rituximab desensitization on blood-type-incompatible adult living donor liver transplantation: a Japanese multicenter study. Am J Transplant. 2014;14(1):102–14.
Lo CM, Shaked A, Busuttil RW. Risk factors for liver transplantation across the ABO barrier. Transplantation. 1994;58(5):543–7.
Bernal W, McPhail MJ. Acute liver failure. J Hepatol. 2021;74(6):1489–90.
Mizota T, Hishiki T, Shinoda M, Naito Y, Hirukawa K, Masugi Y, et al. The hypotaurine-taurine pathway as an antioxidative mechanism in patients with acute liver failure. J Clin Biochem Nutr. 2022;70(1):54–63.
Lill-Elghanian D, Schwartz K, King L, Fraker P. Glucocorticoid-induced apoptosis in early B cells from human bone marrow. Exp Biol Med (Maywood). 2002;227(9):763–70.
Gruver-Yates AL, Quinn MA, Cidlowski JA. Analysis of glucocorticoid receptors and their apoptotic response to dexamethasone in male murine B cells during development. Endocrinology. 2014;155(2):463–74.
Han CZ, Wei Q, Yang MF, Zhuang L, Xu X. The critical role of therapeutic plasma exchange in ABO-incompatible liver transplantation. Hepatobiliary Pancreat Dis Int. 2022;21(6):538–42.
Lee WC, Cheng CH, Lee CF, Hung HC, Lee JC, Wu TH, et al. Quick preparation of ABO-incompatible living donor liver transplantation for acute liver failure. Clin Transplant. 2022;36(3): e14555.
Acknowledgements
We thank Ms. Chie Takaoka, Transplant Coordinator at Keio University Hospital, for data collection of referred patients.
Funding
No external funding was received for this study.
Author information
Authors and Affiliations
Contributions
KH contributed to research design, data analysis, and writing of the manuscript. MS participated in research design, data analysis, and writing of the manuscript. OI, HO, MK, KT, HY, and YA were involved in the research. YK contributed to the research design.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare in relation to this article.
Ethics statement
The protocol for this research project has been approved by the Institutional Review Board of our institute and it conforms to the provisions of the Declaration of Helsinki (approval numbers: 20080136 and 20120443). Informed patient consent was waived due to the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hirukawa, K., Shinoda, M., Hasegawa, Y. et al. Long-term outcomes following ABO-incompatible living donor liver transplantation for acute liver failure: a single-center experience of over 20 years. Surg Today 53, 1160–1172 (2023). https://doi.org/10.1007/s00595-023-02678-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02678-w