Abstract
Purpose
This study was performed to investigate the predictive value of the perioperative D-dimer concentration for the development of postoperative deep vein thrombosis (DVT) after hepatobiliary-pancreatic (HBP) surgery.
Methods
The subjects of this retrospective study were 178 patients who underwent HBP surgery in our hospital between January, 2017 and December, 2021. The D-dimer concentration was measured preoperatively and on postoperative days (POD) 1, 3, and 5. Postoperative DVT was diagnosed based on compression ultrasonography in both lower limbs on POD 6 or 7.
Results
Postoperative DVT developed in 21 (11.8%) of the 178 patients. The D-dimer concentration was significantly higher in the patients with than in those without postoperative DVT before surgery and on PODs 1, 3, and 5. The highest area under the curve of the D-dimer concentration for predicting DVT was 0.762 on POD 3. Multivariate analysis revealed that the D-dimer concentration on POD 3 was an independent predictive risk factor for postoperative DVT, along with the preoperative estimated glomerular filtration rate. Preoperative albumin and D-dimer concentrations were also identified as independent predictive factors of an increase in D-dimer concentration on POD 3.
Conclusions
The D-dimer concentration on POD 3 is a useful predictor of DVT after HBP surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a postoperative complication with multifactorial causes following gastroenterological surgery. In a recent survey on VTE following major gastroenterological surgeries in Japan, the frequency of postoperative DVT and PE was 0.3% (range, 0.1–0.7%) and 0.2% (range, 0.1–0.3%), respectively, and the incidence rate of VTE was similar to that in Western countries [1]. Hepatobiliary-pancreatic (HBP) surgeries, mainly represented by major hepatectomy or pancreaticoduodenectomy, are often highly invasive procedures with a long operative duration; thus, the incidence of VTE following these procedures is higher than that following other gastroenterological surgeries, with the exception of esophagectomy [1, 2]. Although postoperative VTE occurs at a lower rate than other major complications of HBP surgeries, such as pancreatic fistula and bile leakage, it can be life-threatening. PE is potentially fatal and manifests as sudden symptoms, such as dyspnea, chest pain, hypoxemia, and low blood pressure. However, PE is frequently difficult to diagnose early and is often caused by DVT. Therefore, identification of the predictive risk factors for the development of DVT during the perioperative period is critically important to prevent a life-threatening event after HBP surgery.
D-dimer is a marker of endogenous fibrinolysis and is detectable in patients with DVT [3]. Measurement of the D-dimer concentration during the perioperative period can be useful for the diagnosis of DVT in clinical practice and is reportedly a predictive factor for the development of DVT after gastrointestinal and HBP surgery [4, 5]. However, the predictive value of D-dimer measurement during the perioperative period for the early diagnosis of DVT after HBP surgery remains unclear. Moreover, no comparative studies have been performed to identify which HBP surgical procedures are associated with a high risk of DVT.
We conducted the present study to investigate the predictive value of the D-dimer concentration during the perioperative period for the development of early postoperative DVT after HBP surgery and to clarify which HBP surgeries have a high risk of postoperative DVT.
Methods
Patients
We reviewed the medical records of 202 patients who underwent HBP surgery, excluding simple cholecystectomy, at our institution between January, 2017 and December, 2021. After the exclusion of 24 patients for whom data was unavailable, 178 patients were enrolled in this study. The institutional review board of Tottori University approved the study (Approval No. 21A125) and the requirement for informed consent was waived because of the retrospective nature of the study.
Intra- and postoperative prophylaxis for DVT
The patients wore intermittent pneumatic compression devices or elastic compression stockings from the induction of general anesthesia to the morning of POD 1 for prophylaxis of postoperative DVT. Postoperative ambulation was initiated on POD 1. None of the patients received routine prophylactic anticoagulation for DVT.
Evaluation of DVT
The patients underwent compression ultrasonography in both lower limbs to screen for postoperative DVT by two experienced sonographers on postoperative day (POD) 6 or 7. Postoperative DVT was diagnosed according to the presence of fresh thrombosis with a constant intraluminal filling defect or lack of vein compression (Fig. 1).
Clinical characteristics
The following clinical characteristics were collected from the patients’ records: age, sex, body mass index, surgical procedures, histological diagnosis (malignancy or not), American Society of Anesthesiologists classification, VTE risk classification, comorbidities, antithrombotic medication before surgery, preoperative albumin concentration, preoperative platelet count, preoperative C-reactive protein concentration, preoperative prothrombin time, preoperative estimated glomerular filtration rate (eGFR), operative time, and intraoperative blood loss volume. In this study, with respect to the risk classification of DVT, we defined high or highest risk as “high” and intermediate or low risk as “low” in accordance with the Japanese Circulation Society guidelines for VTE [6]. The D-dimer concentration was measured within 7 days prior to surgery and on PODs 1, 3, and 5.
Statistical analysis
Continuous variables are expressed as means and the standard deviation. To assess between-group differences in the clinical variables, the chi-square test or Fisher’s exact probability test was used for categorical variables and the Mann–Whitney U test was used for continuous variables. Receiver operating characteristic (ROC) analysis was performed to evaluate the area under the curve (AUC) of the D-dimer concentration for the prediction of postoperative DVT and the optimal cutoff value of the D-dimer concentration was determined using Youden’s index in the ROC analysis. Univariate and multivariate logistic regression analyses were performed to clarify predictive risk factors for postoperative DVT following HBP surgery. A P value of < 0.05 was considered significant. All statistical analyses were performed using SPSS Version 24 (IBM Corp., Armonk, NY, USA).
Results
Table 1 summarizes the patients’ clinical characteristics. Postoperative DVT developed in 21 (11.8%) of the 178 patients. All patients with postoperative DVT were asymptomatic. Chest enhanced computed tomography, which was performed to screen for pneumonia 1 week after surgery, revealed concomitant asymptomatic PE in one patient. We administered unfractionated heparin intravenously and then changed the anticoagulant therapy to oral edoxaban. No patients with postoperative DVT suffered serious complications during their postoperative clinical course. The incidence of DVT among all hepatobiliary surgeries was higher than that among all pancreatectomies (29.6% vs. 8.4%, respectively). Of the 21 patients with postoperative DVT, 12 (57.1%) had undergone hepatectomy. The incidence of postoperative DVT was highest after hepatopancreatoduodenectomy (2/4, 50.0%) and hepatectomy (S4a + S5 resection or hemihepatectomy + caudate lobectomy) with extrahepatic bile duct resection (4/13, 30.8%). In contrast, postoperative DVT did not develop in any of the patients who underwent extrahepatic bile duct resection with cholecystectomy, which is regarded as a minimally invasive surgery. With respect to the type of surgery, only hepatectomy with extrahepatic bile duct resection, including hepatopancreatoduodenectomy, was significantly associated with postoperative DVT (odds ratio [OR], 7.350; 95% confidence interval [CI], 2.421–22.316; P < 0.001, Table 2).
Table 3 compares the clinical characteristics between the patients with and those without postoperative DVT. There were significant correlations between the two groups with respect to age; VTE risk classification; preoperative serum albumin concentration; preoperative eGFR; D-dimer concentration before surgery and on PODs 1, 3, and 5; operative time; and hepatectomy with extrahepatic bile duct resection, including hepatopancreatoduodenectomy. The mean age and rate of high risk by VTE risk classification for postoperative DVT were significantly higher for the patients with DVT than for those without DVT. The D-dimer concentration was significantly higher for the patients with postoperative DVT than for those without postoperative DVT at all time points: before surgery and on PODs 1, 3, and 5. The D-dimer concentration increased gradually from the preoperative period to POD 5 in the patients with and those without postoperative DVT. The D-dimer concentration was highest on POD 5 in the patients with and those without postoperative DVT. However, the disparity of the D-dimer concentration between the patients with and those without postoperative DVT on POD 3 was greatest among all the time points. The incidence of hepatectomy (S4a + S5 resection or hemihepatectomy + caudate lobectomy) with extrahepatic bile duct resection, including hepatopancreatoduodenectomy, was significantly higher in the patients with than in those without DVT. In contrast, both the preoperative albumin concentration and preoperative eGFR were significantly lower in the patients with than in those without postoperative DVT.
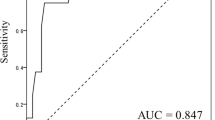
Based on the highest Youden indices of the ROC analysis, the optimal cutoff values of the D-dimer concentration were as follows: 0.45 before surgery, 5.35 on POD 1, 6.25 on POD 3, and 12.10 on POD 5. ROC analysis revealed that the AUC of the D-dimer concentration for the discrimination ability to predict postoperative DVT was 0.762 (P < 0.001) on POD 3, which was the highest value among all AUCs of the D-dimer concentrations measured in this study (0.738 before surgery, P < 0.001; 0.672 on POD 1, P = 0.001; and 0.655 on POD 5, P = 0.021) (Fig. 2).
Multivariate analysis of the predictive risk factors for DVT in early postoperative period revealed that the D-dimer concentration on POD 3 was an independent risk factor for postoperative DVT (OR, 4.149; 95% CI 1.104–15.593; P = 0.035), along with the preoperative eGFR (OR, 4.858; 95% CI 1.571–15.026; P = 0.006) in patients who underwent HBP surgery (Table 4). We also performed logistic regression analysis to investigate the preoperative factors for predicting high D-dimer concentrations on POD 3. The results of this analysis are shown in Table 5. Preoperative albumin and D-dimer concentrations were identified as independent predictive factors of an increase in the D-dimer concentration on POD 3. Based on this finding, we evaluated the AUC of the combination of the preoperative D-dimer concentration or the preoperative albumin concentration and the D-dimer concentration on POD 3. The AUCs of the combination of preoperative D-dimer concentration or preoperative albumin concentration and D-dimer concentration on POD 3 were 0.787 (P < 0.001) and 0.732 (P = 0.001), respectively. The AUC of the combination of the D-dimer concentration before surgery and on POD 3 was slightly superior to that of the D-dimer concentration on POD 3 alone (Fig. 3).
Discussion
HBP surgeries are associated with serious and potentially fatal complications because they are among the most highly invasive of all gastroenterological surgeries. DVT is often asymptomatic in the early period and it usually occurs postoperatively, during the first 12 (median) days after surgery [2]. Untreated asymptomatic DVT can result in PE, which may progress to a life-threatening condition. Therefore, predicting the development of DVT during the perioperative period is important for avoiding this situation after HBP surgery. Several studies have demonstrated that D-dimer assays have a high negative predictive value, and that D-dimer is a sensitive but nonspecific marker of DVT [3, 7]. In fact, a perioperative elevated D-dimer concentration is reportedly a reliable predictive risk factor for postoperative DVT [8,9,10]. However, few reports have addressed the usefulness and optimal timing of D-dimer assay for predicting DVT during the perioperative period following HBP surgery. Moreover, which HBP surgical procedures are most strongly associated with the development of postoperative DVT remain unclear. We conducted the present study to address these issues.
This study is the first to demonstrate that the D-dimer concentration on POD 3 is a simple and readily available factor for early prediction of the development of DVT in patients following HBP surgery. D-dimer is a fibrin-related marker that serves as an indicator of coagulation activation and fibrinolysis. A high D-dimer concentration is recognized as a reliable marker for a hypercoagulable state [11]. The elevation of D-dimer continues for several days because its half-life in plasma is longer (range, 3–48 h) than that of other fibrin-related markers [12]. Accordingly, we presumed that the absolute value of D-dimer may not appreciably predict the development of DVT in the early postoperative period. The current study showed that the D-dimer concentration was significantly higher in patients with than in those without postoperative DVT before surgery and on PODs 1, 3, and 5, and that the D-dimer concentration increased gradually from preoperatively to POD 5, when its highest value was reached. However, the optimal timing of D-dimer measurement for the prediction of DVT was identified as POD 3, which showed the greatest disparity in the D-dimer concentration between the patients with and those without DVT, and not POD 5, which showed the highest absolute value of the D-dimer concentration. This suggests that the disparity in the D-dimer concentration between the two groups is more important than the absolute value for predicting DVT during the early postoperative period. Yang et al. [13] reported that a highly significant deviation of the plasma D-dimer concentration between patients with and those without DVT was found on POD 3, with an AUC of 0.924 in the ROC analysis, in younger patients who underwent open reduction and internal fixation of lower limb fractures. Likewise, in another study, the greatest disparity of the D-dimer concentration between patients with and those without postoperative VTE after lung surgery was observed on POD 3, with significance, and the AUC on POD 3 was highest for the prediction of postoperative VTE [14]. Moreover, the concentration of fibrinogen degradation products, which are fibrin-related factors, was significantly higher in patients with than in those without VTE only on POD 3 after lung surgery [14]. These reports support the usefulness of D-dimer measurement on POD 3 for the prediction of DVT after HBP surgery, as found in the current study. Preoperative factors, particularly preoperative D-dimer concentration, are believed to affect the development of postoperative DVT. Similarly, in this study, the preoperative D-dimer concentration was identified as a factor predictive of an increase in the D-dimer concentration on POD 3. Therefore, we evaluated the AUC of the combination of D-dimer concentration before surgery and on POD 3 under the hypothesis that accurate prediction was possible by combining pre- and postoperative D-dimer concentrations. However, the results showed that the AUC of the combination of D-dimer concentration before surgery and on POD 3 was only slightly superior to that of the D-dimer concentration on POD 3 alone. Although the development of postoperative DVT is multifactorial, which might affect the AUC values, our results suggest that the measurement of D-dimer concentration on POD 3 alone is an option for detecting postoperative DVT.
Transient dysfunction of the liver, especially synthetic dysfunction, occurs after hepatectomy, which impairs postoperative coagulability. Patients who have undergone hepatectomy suffer a brief hypercoagulable state despite an elevation in the prothrombin time–international normalized ratio [15]. Thus, these patients are considered more predisposed to postoperative VTE than patients who have undergone other gastroenterological surgeries associated with less impairment of coagulability. Post-hepatectomy VTE is closely associated with the extent of liver resection. Studies have shown that patients who underwent liver resection with obesity or extended liver resection were at higher risk of VTE [16, 17]. Furthermore, with respect to the association between the operative approach and the incidence rate of VTE following hepatectomy, open major hepatectomy is the operative approach with the highest risk for postoperative VTE among all operative approaches to hepatectomy, including combinations of an open or minimally invasive approach and major or minor hepatectomy [18]. Extended hepatectomy with extrahepatic bile duct resection or hepatopancreatoduodenectomy is the most invasive, with both a longer operative duration and greater intraoperative blood loss than simple hepatectomy without extrahepatic bile duct resection. Furthermore, both a prolonged operation time and intraoperative blood transfusion are risk factors for VTE in HBP surgery [19,20,21]. Therefore, we assumed that hepatectomy (S4a + S5 resection or hemihepatectomy + caudate lobectomy) with extrahepatic bile duct resection, including hepatopancreatoduodenectomy, was a major risk factor for the development of DVT after HBP surgery. Our results showed that hepatectomy (S4a + S5 resection or hemihepatectomy + caudate lobectomy) with extrahepatic bile duct resection, including hepatopancreatoduodenectomy, was consistently the highest-risk procedure for the development of postoperative DVT among the many HBP surgical procedures. However, the present study could not confirm whether hepatectomy (S4a + S5 resection or hemihepatectomy + caudate lobectomy) with extrahepatic bile duct resection, including hepatopancreatoduodenectomy, was an independent risk factor for the development of DVT after HBP surgery, although it tended to show significance. The small sample size in the present study might have affected this result.
This study has two main limitations. First, it was a retrospective study involving a small cohort of only Asian individuals, which may have led to bias, prompting the need for a large-scale, prospective study to confirm our results. Second, we performed only ultrasonography to assess the development of postoperative DVT, based on a previous report on the diagnosis of DVT by Di Nisio [22]. However, using only ultrasonography might have affected the diagnostic accuracy of detecting postoperative DVT. Therefore, preoperative ultrasonography and examinations using other modalities should be considered in future studies for accurate evaluation of the development of postoperative DVT.
In conclusion, measuring the D-dimer concentration on POD 3 is a simple, convenient, cost-effective, and useful tool for the early prediction of DVT after HBP surgery. Moreover, high D-dimer concentrations on POD 3 could be predicted by albumin levels or D-dimer preoperatively. Patients with a high D-dimer concentration, especially those with both a high D-dimer concentration on POD 3 and extended hepatectomy with extrahepatic bile duct resection or hepatopancreatoduodenectomy, should receive early postoperative thromboprophylaxis to prevent postoperative DVT.
Data availability
All authors are available for the data of this study.
References
Hata TIM, Miyata H, Nomura M, Gotoh M, Sakon M, Yamamoto K, et al. Frequency and risk factors for venous thromboembolism after gastroenterological surgery based on the Japanese national clinical database (516 217 cases). Ann Gastroenterol Surg. 2019;3(5):534–43.
Merkow RP, Bilimoria KY, McCarter MD, Cohen ME, Barnett CC, Raval MV, et al. Post-discharge venous thromboembolism after cancer surgery: extending the case for extended prophylaxis. Ann Surg. 2011;254(1):131–7.
Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349(13):1227–35.
Sugimachi K, Tajiri H, Kinjo N, Ikebe M, Wang H, Tanaka K, et al. Incidence and predictors of deep venous thrombosis after abdominal oncologic surgery: prospective Doppler ultrasound screening. J Surg Res. 2012;178(2):657–61.
Hayashi H, Shimizu A, Kubota K, Notake T, Sugenoya S, Masuo H, et al. Asymptomatic venous thromboembolism after hepatobiliary-pancreatic surgery: early detection using d-dimer and soluble fibrin monomer complex levels. Ann Gastroenterol Surg. 2022;6(1):109–18.
Guidelines for the diagnosis. Treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS 2009). Circ J. 2011;75(5):1258–81.
Wells PS, Brill-Edwards P, Stevens P, Panju A, Patel A, Douketis J, et al. A novel and rapid whole-blood assay for D-dimer in patients with clinically suspected deep vein thrombosis. Circulation. 1995;91(8):2184–7.
Shi A, Huang J, Wang X, Li M, Zhang J, Chen Y, et al. Postoperative D-dimer predicts venous thromboembolism in patients undergoing urologic tumor surgery. Urol Oncol. 2018;36(6):307.
Yamaguchi T, Wada H, Miyazaki S, Hasegawa M, Wakabayashi H, Asanuma K, et al. Fibrin-related markers for diagnosing acute-, subclinical-, and pre-venous thromboembolism in patients with major orthopedic surgery. Int J Hematol. 2016;103(5):560–6.
Inoue H, Watanabe H, Okami H, Kimura A, Seichi A, Takeshita K. D-dimer predicts pulmonary embolism after low-risk spine surgery. Spine Surg Relat Res. 2018;2(2):113–20.
Nomura H, Wada H, Mizuno T, Katayama N, Abe Y, Noda M, et al. Negative predictive value of D-dimer for diagnosis of venous thromboembolism. Int J Hematol. 2008;87(3):250–5.
van der Putten RF, Glatz JF, Hermens WT. Plasma markers of activated hemostasis in the early diagnosis of acute coronary syndromes. Clin Chim Acta. 2006;371(1–2):37–54.
Yang Y, Zan P, Gong J, Cai M. D-dimer as a screening marker for venous thromboembolism after surgery among patients younger than 50 with lower limb fractures. Clin Appl Thromb Hemost. 2017;23(1):78–83.
Tian B, Song C, Li H, Zhang W, Chen Q, Chen S, et al. The significance of perioperative coagulation and fibrinolysis related parameters after lung surgery for predicting venous thromboembolism: a prospective, single center study. J Thorac Dis. 2018;10(4):2223–30.
Barton JS, Riha GM, Differding JA, Underwood SJ, Curren JL, Sheppard BC, et al. Coagulopathy after a liver resection: is it over diagnosed and over treated? HPB (Oxford). 2013;15(11):865–71.
Turley RS, Reddy SK, Shortell CK, Clary BM, Scarborough JE. Venous thromboembolism after hepatic resection: analysis of 5,706 patients. J Gastrointest Surg. 2012;16(9):1705–14.
Onda S, Furukawa K, Haruki K, Hamura R, Shirai Y, Yasuda J, et al. D-dimer-based screening for early diagnosis of venous thromboembolism after hepatectomy. Langenbecks Arch Surg. 2021;406(3):883–92.
Hue JJ, Katayama E, Markt SC, Rothermel LD, Hardacre JM, Ammori JB, et al. Association between operative approach and venous thromboembolism rate following hepatectomy: a propensity-matched analysis. J Gastrointest Surg. 2021;25(11):2778–87.
Ejaz A, Spolverato G, Kim Y, Lucas DL, Lau B, Weiss M, et al. Defining incidence and risk factors of venous thromboembolism after hepatectomy. J Gastrointest Surg. 2014;18(6):1116–24.
Beal EW, Tumin D, Chakedis J, Porter E, Moris D, Zhang XF, et al. Identification of patients at high risk for post-discharge venous thromboembolism after hepato-pancreato-biliary surgery: which patients benefit from extended thromboprophylaxis? HPB (Oxford). 2018;20(7):621–30.
Hue JJ, Elshami M, Beckman MJ, Driedger MR, Rothermel LD, Hardacre JM, et al. A propensity-matched analysis of the postoperative venous thromboembolism rate after pancreatoduodenectomy based on operative approach. J Gastrointest Surg. 2022;26(3):623–34.
Di Nisio M, van Es N, Büller HR. Deep vein thrombosis and pulmonary embolism. Lancet. 2016;388(10063):3060–73.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: TS; data acquisition: YM and TH; data analysis and interpretation: TS, SF, and TM; statistical analysis: TS, MY, and ST; manuscript preparation: TS; manuscript editing: NT and TH; manuscript review: YF; final approval of the article: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakamoto, T., Murakami, Y., Hanaki, T. et al. Evaluation of perioperative D-dimer concentration for predicting postoperative deep vein thrombosis following hepatobiliary-pancreatic surgery. Surg Today 53, 773–781 (2023). https://doi.org/10.1007/s00595-023-02645-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02645-5