Abstract
Purpose
Subsequent to the publication of “Guidelines for cadaver dissection in education and research of clinical medicine” in 2012, cadaver surgical training (CST) was implemented in various surgical fields across Japan. This article summarizes the recent progress made in the implementation of CST using donated cadavers, and its associated research, focusing on the field of surgery, and discusses its future direction.
Methods
All reports from 2012 to 2021 registered with the CST Promotion Committee of the Japan Surgical Society were analyzed. There were 292 (24.9%) programs in the field of surgery, including acute care surgery, out of a total of 1173 programs overall. Data were classified by the purpose of implementations and fields of surgery, with subclassification by organ, costs and participation fees.
Results
CST and its research were introduced in 27 (33.3%) of a total 81 universities. The total number of participants was 5564 and the major (80%) purpose of the program was to advance surgical techniques. When classified by objectives, 65, 59 and 11% were for mastering operations for malignant disease, minimally invasive surgery, and transplantation surgery, respectively.
Conclusion
CST in the field of surgery is increasing progressively in Japan, but still with disproportionate dissemination. Further efforts are needed to achieve full adoption.
Similar content being viewed by others
Introduction
In 2012, the “Guidelines for cadaver dissection in education and research of clinical medicine” was published [1, 2]. By complying with the rules stipulated in these guidelines and the preexisting laws, it has become possible to legally implement cadaver surgical training (CST) and use donated cadavers for clinical research and development (R&D) in medical and dental universities and colleges throughout Japan. According to the guidelines, all CST and R&D programs implemented in Japan must be reported to the CST Promotion Committee (CST-PC) of the Japan Surgical Society (JSS). Based on these data, the number of CST and R&D programs was aggregated to 1173 [3]. The highest number of programs was conducted by departments of orthopedic surgery (314 programs: 27%), followed by departments of surgery (249 programs: 21%), then by departments of neurosurgery and otorhinolaryngology.
The present report gives an overview of the CST and R&D programs in the field of surgery in Japan, as their details have not been published in any other scientific report. Thus, we share with readers information on the current state of CST and R&D in the field of surgery and discuss the future direction of CST in Japan.
Materials and methods
Based on the guidelines and requirements, the CST-PC receives annual reports of all CST and R&D programs. As of July, 2021, 1173 cases had been reported, 249 of which were from departments of surgery and 51 were from departments of emergency medicine and ICU [3]. For this study, all 1173 programs were examined and the those that involved training in operative procedures and research, as listed in the curriculum of the Board Certification of Surgery of the JSS, were extracted and classified further [4]. Thus, the number of programs aggregated as procedures in the field of surgery in this study differed from the number in previous studies based on categorization by the name of the implementing department [3].
Extraction and classification of the data
When we extracted all CST and R&D programs listed in the training curriculum of operations on the Board Certification of Surgery of the JSS, including acute care surgery, implemented by the departments of surgery, emergency medicine, and ICU, 292 programs were included. Data were summarized by year and included classification of the field of surgery and organs, classification of the purpose of implementation, number of times each program was implemented, number of cadavers used and the methods of embalming, total costs, participation fees, and cooperation by companies. The deadlines for submission of the reports were in July of each year, and the implementations in the previous fiscal years (April to next March) were reported. Therefore, the data shown in 2021 were aggregate results from January to March, 2021.
Classification of the program by purpose
The reporting system requires default answers on the purpose of the implementation of CST and R&D. CSTs were further subdivided into three categories based on the level of education: basic medical, standard surgical, and advanced surgical techniques. R&D programs were also subdivided into the following three categories according to purpose: research of clinical anatomy, R&D of novel surgical procedures, and R&D of medical devices. Duplicate counts were allowed in the aggregation.
Classification by fields of surgery and subclassification by organ
In accordance with the curriculum of the Board Certification of Surgery of JSS, the fields of CST and R&D were classified into the following eight categories: 1. digestive and abdominal organs; 2. mammary glands; 3. thoracic; 4. heart, aorta, and vena cava; 5. peripheral blood vessels; 6. head and neck, body surface, and endocrine; 7. pediatric; and 8. trauma. The subclassification of each field was done by organ.
Distinctive programs
Categories of common surgical purposes and procedures were set across the fields and included transplantation surgery, trauma surgery, surgical oncology (operations of malignant disease), endoscopic and minimum invasive surgery, including robot-assisted surgery, and the number of corresponding programs were counted. As an example of advanced medical technologies, mediastinoscopic radical esophagectomy for esophageal cancer [5,6,7], transanal minimally invasive surgery (TAMIS) and transanal total mesorectal excision (TaTME) for rectal cancer [8, 9], laparoscopic pancreaticoduodenectomy (Lap-PD) for pancreatic lesions [10], and minimally invasive cardiac surgery (MICS) for cardiovascular lesions [11] were selected, and their numbers were counted.
Total costs and participation fees
The total costs listed in the reports, divided by the number of implementations, were obtained as the implementation costs per session. Data on the participation fee for CSTs were extracted from the descriptions in the reports, and the median and mode of the fees were calculated.
Disclosure of conflict of interest (COI)
The guidelines stipulate that in order to ensure transparency in CST and R&D supported by human body donations, COIs of support by companies (including donations, lending of paid or unpaid goods, and labor offerings) for each program must be disclosed. The accumulated COI data were summarized in accordance with the description in each report.
Ethical considerations
All programs conducted at the universities were approved by their respective ethical boards. In addition, anonymized data reported to the JSS, in accordance with the guidelines, were used for the current study.
Results
Outline of the programs
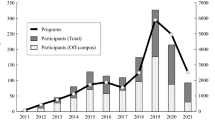
The total number of programs applicable to the field of surgery was 292, in which 577 sessions of CST and R&D were implemented (Table 1). The total number of participants, including trainers and trainees, was 5564, and the number of participants from outside the host universities (off-campus) accounted for approximately half of the total number of participants (2503). The guidelines not only limit the implementation of CST to medical and dental universities and colleges, but also encourage off-campus participants. In line with the principles of the guidelines, many off-campus surgeons participated in the programs and sessions. Since 2019, the number of participating medical schools has expanded significantly because of an increase in the budget from the Ministry of Health, Labour and Welfare (Fig. 1). As of 2021, 27 universities in 21 prefectures had implemented CST in the field of surgery (Fig. 2). This represents approximately one-third of the 81 medical schools in Japan. Moreover, even though 38 medical schools have implemented CST [3], 11 of them have not initiated it in their surgical departments.
Annual trends in the number of programs and participants of cadaver surgical training and research and development in the field of surgery. The annual breakdown of the number of sessions is shown in the bar graph. The data for 2021 are cumulative from January to the end of March. The breakdown of the total number of participants and the number of off-campus participants by year are shown in the line graphs. Total: total number of participating surgeons; off-campus: number of participating surgeons who do not belong to a university; CST cadaver surgical training, R&D research and development
Nationwide distribution of universities implementing cadaver surgical training in Japan. Twenty-seven (33%) of the 81 medical schools, in 21 of the total 47 prefectures in Japan, have been implementing CST in the field of surgery. All prefectures in Japan have at least one medical school. Gray one university in the prefecture, black two or more universities in the prefecture, CST cadaver surgical training
The number of cadavers used was 879 (Table 1). The embalming methods applied were Thiel fixation in 242 [12], formalin fixation in 22, SSS methods in 20 [13], and a preservation method in 1. Unfixed cadavers were used in 28 cases. Thiel fixation, which allows cadavers to be stored at room temperature, using a solution containing formalin, is associated with less risk of infection by pathogens. This embalming method is most commonly used as the standard.
Purpose of the programs
The guidelines classify the objectives into two categories: CST and R&D, which are further subdivided. The CST objectives included basic medical techniques (n = 43; 14%), standard surgical techniques (n = 177; 40%), and advanced surgical techniques (n = 233; 80%). The purposes of R&D were for clinical anatomy (n = 84; 29%), for novel surgical procedures (n = 28; 10%), and for medical devices (n = 16; 5%). The most common reason for implementing CST was to acquire advanced surgical techniques, whereas the use of cadavers for developing medical devices was rare (Fig. 3).
Scale and budget of the programs
The average number of participating surgeons in one session was 11.2, among whom 4.7 were from off-campus. The median cost per session was 98,910 yen, and the average cost was 274,313 yen. The median cost per session in the surgical field was lower than the value obtained from the entire medical field (153,180 yen) [3]. The minimum amount was 0 yen for 41 programs, whereas the cost for five programs exceeded 2 million yen, the maximum cost being 2,749,373 yen. Four of these programs were the North American trauma surgery training courses “Advanced Surgical Skills for Exposure in Trauma” (ASSET) [14] introduced in Japan, and one was a live surgery session conducted as an event at an academic congress. The costs of 128 (43.8%) programs were covered by public funds, donations from academic societies and NPOs, and 99 programs were supported by grants from the Ministry of Health, Labour, and Welfare.
More than half of the programs (186: 63.7%) were free of charge (Fig. 4). Among the 106 programs that were charged, the average fee was 28,702 yen, (range, 1,000–160,000 yen), and the median and mode were 20,000 and 10,000 yen (16 programs), respectively. The highest fee was 160,000 yen for the ASSET course.
A COI was identified in 177 cases (60.6%) within the program, because of donations (n = 8), provision of equipment (n = 149), or provision of labor (n = 115).
Details of the implementations in each field and organ
A total 292 programs were implemented. Table 2 summarizes the objectives and fields in surgery in order of the number of implementations. When classified by objectives, 189 programs were training programs for surgical oncology, accounting for 65% of the total. There were 172 (59%) cases of training and R&D for minimally invasive procedures, such as laparoscopic surgery and robotic surgery, although only 8 were for robotic surgery. There were 31 for training in transplant surgery (11%), consisting of 18 for lung transplants, 13 for liver transplants, and 9 for pancreas transplants, but only 2 for heart transplants (data contain duplicates).
Digestive surgery
The most common subjects involved the digestive tract and abdominal organs, accounting for 172 cases (59%). The colon, rectum, and anus were the most frequent subjects (n = 65). It is noteworthy that workshops for TaTME or TAMIS, as recent advanced medical technology, have been held across the country, with 16 programs reported. The second most common was CST for esophageal operations (n = 58). Nineteen CST programs for mediastinoscopic radical esophagectomy have been performed nationwide recently, to promote a better understanding of the mediastinal anatomy and perform a safe procedure. Pancreatic surgery was the next most frequent (n = 46). Laparoscopic pancreatic surgery for pancreatic tumors, including Lap-PD, is one of the most difficult minimally invasive surgeries, and there were 16 CST programs for that.
Trauma surgery
The second most common area of CST was trauma surgery, with 53 programs reported. Several comprehensive programs for systemic trauma operations had already been developed, and these programs have been implemented throughout the country. As a program developed in Japan, the “cadaver-based educational seminar for trauma surgery (CESTS)” was registered as 19 programs from four universities [15], and the ASSET was registered as 8 programs from three universities [14].
Thoracic surgery
The third most common area of CST was in the field of thoracic surgery, with 52 programs reported, 50 of which focused on surgery for lung malignancy. They included 22 training programs of high-difficulty surgical techniques. such as those requiring resection and reconstruction of the trachea and bronchi. There were 18 programs for lung transplantation reported.
Cardiovascular surgery
Seventeen programs targeted the heart, aorta, and vena cava. Sixteen of the projects were for the simulation of MICS, which requires an advanced surgical technique. Programs for heart transplantation were not applied widely, with only two counted.
Discussion
CST and R&D in the field of surgery is currently implemented in 27 of 81 medical schools in Japan (Fig. 2). From the fiscal year of 2012, the Ministry of Health, Labour and Welfare allocated approximately 45 million yen for competitive budgets to medical and dental schools that have implemented CST. From the fiscal year of 2018, these budgets were increased significantly to approximately 300 million yen. As a result, from the fiscal year of 2018 to 2019, the number of medical schools in Japan that implemented CST in the field of surgery increased significantly from 12 to 22 (Table 1). Moreover, the impact of the COVID-19 pandemic, which began in 2020, was primarily observed as a decline in the acceptance of off-campus participants (611 in 2019 to 364 in 2020), and whether this decline is temporary warrants further investigation.
The most common objective of CST and R&D was to master advanced surgical techniques, accounting for 80% of the programs. For the safe dissemination of minimally invasive surgery, programs such as TaTME and Lap-PD in gastroenterological surgery and MICS in cardiovascular surgery are being implemented nationwide. Although endoscopic surgery programs are performed widely, robotic surgery training has been conducted only five times, with just 27 participants, revealing that no platform has been established in Japan for conducting cadaver training for competence in robotic surgery.
In Japan, there is at least one medical school in each prefecture, but there is a disproportionate distribution of the implementation of CST (Fig. 2). What should be done to promote the implementation of CST in every prefecture in the future? According to the guidelines, CST should be conducted under the supervision of the department of anatomy of each medical school; however, some medical schools cannot implement CST because of the heavy burden imposed on the department of anatomy. The lack of knowledge necessary for the implementation of CST in the surgical department responsible for programs can also hinder its implementation. Possible actions to help solve these problems are as follows: A new organization to promote the implementation of CST should be formed within each university, in cooperation with the clinical departments and anatomy department that will support the implementation through equipment management, schedule coordination, and assignment of the use of cadavers. By establishing such organization, anatomy departments of universities can be devoted to the education of anatomy for medical students and management of the cadavers. Since the barriers to implementing CST programs in the surgical field are the establishment and management of programs and the preparation of devices, sharing the programs may be effective for their promotion. For example, CESTS, a trauma surgery training course that deploys a common program at multiple universities, could be an ideal model to promote the future implementation of CST [15]. If CST programs are established and carried out under the leadership of academic societies and organizations, this may further reduce the pressure on surgeons in charge of the program and the costs of equipment provision by sharing preestablished educational programs and equipment. This approach would not only facilitate the implementation of CST, but also make it easier to receive financial support from companies. Moreover, it may be ideal to shift the government’s funds from supporting individual universities to supporting cross-regional programs implemented by academic societies and organizations.
In this study, the classification of surgical procedures by the JSS’s Board Certification was applied. The credits for the certification are based on the On-JT, and a certain number of experiences of a “real operation” are required in various surgical specialties other than trauma surgery. The opportunity to encounter an operation for trauma is rare; thus, simulation programs on animals and cadavers, including ASSET [14], can be credited as a certification. Although On-JT is an essential and effective educational method, time constraints and imbalances in the opportunities for its implementation exist. The disadvantages of patients who receive treatment as part of training should also be considered. Thus, we believe that CST should be included in the requirements for qualification, including the Board Certification of Surgery and other advanced certifications in various fields.
Conclusion
CST in the field of surgery in Japan has been increasing with the aim of safely disseminating advanced surgical techniques. However, only 27 (33.3%) of 81 medical universities have implemented the program and it is necessary to change the status quo to promote its implementation in all universities.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Shichinohe T, Kondo T, Date H, Hiramatsu M, Hirano S, Ide C, et al. Guidelines for cadaver dissection in education and research of clinical medicine (The Japan Surgical Society and The Japanese Association of Anatomists). Surg Today. 2022;52:989–94. https://doi.org/10.1007/s00595-022-02525-4.
Shichinohe T, Kondo T, Date H, Hiramatsu M, Hirano S, Ide C, et al. Guidelines for cadaver dissection in education and research of clinical medicine (The Japan Surgical Society and The Japanese association of anatomists). Anat Sci Int. 2022;97:235–40. https://doi.org/10.1007/s12565-022-00665-8.
Shichinohe T, Date H, Hirano S, Kobayashi E, Izawa Y, Shirakawa Y, et al. Usage of cadavers in surgical training and research in Japan over the past decade. Anat Sci Int. 2022;97:241–50. https://doi.org/10.1007/s12565-022-00659-6.
Japan Surgical Society. Reference: list of surgical procedures (goals of experiences); 2022 (in Japanese). https://jp.jssoc.or.jp/uploads/files/specialist/curriculum-new_02.pdf. Accessed 11 Sep
Tokairin Y, Nagai K, Fujiwara H, Ogo T, Okuda M, Nakajima Y, et al. Mediastinoscopic subaortic and tracheobronchial lymph node dissection with a new cervico-hiatal crossover approach in Thiel-embalmed cadavers. Int Surg. 2015;100:580–8. https://doi.org/10.9738/INTSURG-D-14.00305.1.
Mori K, Aikou S, Yagi K, Nishida M, Mitsui T, Yamagata Y, et al. Technical details of video-assisted transcervical mediastinal dissection for esophageal cancer and its perioperative outcome. Ann Gastroenterol Surg. 2017;1:232–7. https://doi.org/10.1002/ags3.12022.
Fujiwara H, Shiozaki A, Konishi H, Kosuga T, Komatsu S, Ichikawa D, et al. Perioperative outcomes of single-port mediastinoscope-assisted transhiatal esophagectomy for thoracic esophageal cancer. Dis Esophagus. 2017;30:1–8. https://doi.org/10.1093/dote/dox047.
Atallah S, Albert M, Larach S. Transanal minimally invasive surgery: a giant leap forward. Surg Endosc. 2010;24:2200–5. https://doi.org/10.1007/s00464-010-0927-z.
de Lacy AM, Rattner DW, Adelsdorfer C, Tasende MM, Fernández M, Delgado S, et al. Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to-up” total mesorectal excision (TME)–short-term outcomes in the first 20 cases. Surg Endosc. 2013;27:3165–72. https://doi.org/10.1007/s00464-013-2872-0.
Kuroki T, Fujioka H. Training for laparoscopic pancreaticoduodenectomy. Surg Today. 2019;49:103–7. https://doi.org/10.1007/s00595-018-1668-1.
Okamoto K. Minimally invasive cardiac surgery in Japan: history and current status. Gen Thorac Cardiovasc Surg. 2018;66:504–8. https://doi.org/10.1007/s11748-018-0971-5.
Thiel W. The preservation of the whole corpse with natural color. Ann Anat. 1992;174:185–95. https://doi.org/10.1016/S0940-9602(11)80346-8.
Hayashi S, Naito M, Kawata S, Qu N, Hatayama N, Hirai S, et al. History and future of human cadaver preservation for surgical training: from formalin to saturated salt solution method. Anat Sci Int. 2016;91:1–7. https://doi.org/10.1007/s12565-015-0299-5.
Kuhls DA, Risucci DA, Bowyer MW, Luchette FA. Advanced surgical skills for exposure in trauma: a new surgical skills cadaver course for surgery residents and fellows. J Trauma Acute Care Surg. 2013;74:664–70. https://doi.org/10.1097/TA.0b013e31827d5e20.
Homma H, Oda J, Sano H, Kawai K, Koizumi N, Uramoto H, et al. Advanced cadaver-based educational seminar for trauma surgery using saturated salt solution-embalmed cadavers. Acute Med Surg. 2019;6:123–30. https://doi.org/10.1002/ams2.390.
Acknowledgements
Since the publication of the guidelines, all reports from universities have been compiled as CST data through the efforts of the Guideline Review Committee, which has now become the CST Promotion Committee of the JSS. 2012 Guideline Review Committee: Takashi Kondo, Yoshiro Matsui, Yoshimitsu Izawa, Chizuka Ide, Toshihiko Iwanaga, Yasuo Uchiyama, Akio Kikuta, Eiji Kobayashi, Toshiaki Shichinohe, Yutaka Nohara, and Kazunari Yoshida. 2018 CST Promotion Committee: Hiroshi Date, Satoshi Hirano, Yoshimitsu Izawa, Eiji Kobayashi, Toshiaki Shichinohe, Yasuhiro Shirakawa, Masako Hiramatsu, Kazunari Yoshida, Hiroshi Taneichi, Hiroyuki Yaginuma, Yasuo Uchiyama, Toshiyuki Tsurumoto, Masahiko Watanabe, Takanori Shibata, Haruo Takahashi, Takane Suzuki, and Kumiko Yamaguchi. 2022 CST Promotion Committee: Etsuro Hatano, Masako Hiramatsu, Eiji Kobayashi, Yoshimitsu Izawa, Toshiaki Shichinohe, Yasuhiro Shirakawa, Takane Suzuki, Kumiko Yamaguchi, Toshiyuki Tsurumoto, Toyoshi Fujimoto, Hiroyuki Yaginuma, Masahiko Watanabe, Hiroshi Taneichi, Hiroshi Kurita, Naohito Hato, Tomoyasu Kato, Mitsuhito Mase, Hiroomi Kanayama, and Yoshimasa Takeda. Finally, we thank Takahiro Uesawa and Kentaro Kaneko of the Japan Surgical Society secretariat for their years of work in the CST reporting office.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Toshiaki Shichinohe, Hiroshi Date, Eiji Kobayashi, Masako Hiramatsu, Satoshi Hirano, Yoshimitsu Izawa and Yasuhiro Shirakawa: 2018 CST Promotion Committee of the Japan Surgical Society, affiliated member of the Japan Surgical Society.
Toshiaki Shichinohe, Etsuro Hatano, Eiji Kobayashi, Masako Hiramatsu, Yoshimitsu Izawa and Yasuhiro Shirakawa: 2022 CST Promotion Committee of the Japan Surgical Society, affiliated member of the Japan Surgical Society.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shichinohe, T., Date, H., Hatano, E. et al. Cadaver surgical training and research using donated cadavers in the field of surgery in Japan: an overview of reports from 2012 to 2021. Surg Today 53, 984–991 (2023). https://doi.org/10.1007/s00595-023-02642-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02642-8