Abstract
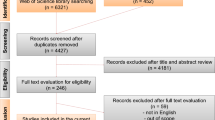
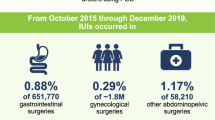
Iatrogenic ureteral injury (IUI) during colorectal surgery is a rare complication but related to a serious burden of morbidity. This comprehensive and systematic review aims to provide a critical overview of the most recent literature about IUI prevention techniques in colorectal surgery. We performed a comprehensive and systematic review of studies published from 2000 to 2022 and assessed the use of techniques for ureteral injury prevention and intraoperative localization. 26 publications were included, divided into stent-based (prophylactic/lighted ureteral stent and near-infrared fluorescent ureteral catheter [PUS/LUS/NIRFUC]) and fluorescent dye (FD) groups. Costs, the percentage and number of IUIs detected, reported limitations, complication rates and other outcome points were compared. The IUI incidence rate ranged from 0 to 1.9% (mean 0.5%) and 0 to 1.2% (mean 0.3%) in the PUS/LUS/NIRFUC and FD groups, respectively. The acute kidney injury (AKI) and urinary tact infection (UTI) incidence rate ranged from 0.4 to 32.6% and 0 to 17.3%, respectively, in the PUS/LUS/NIRFUC group and 0–15% and 0–6.3%, respectively, in the FD group. Many other complications were also compared and descriptively analyzed (length-of-stay, mortality, etc.). These techniques appear to be feasible and safe in select patients with a high risk of IUI, but the delineation of reliable guidelines for preventing IUI will require more randomized controlled trials.



Similar content being viewed by others
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Palaniappa NC, Telem DA, Ranasinghe NE, Divino CM. Incidence of iatrogenic ureteral injury after laparoscopic colectomy. Arch Surg. 2012;147(3):267–71. https://doi.org/10.1001/ARCHSURG.2011.2029.
Andersen P, Andersen LM, Iversen LH. Iatrogenic ureteral injury in colorectal cancer surgery: a nationwide study comparing laparoscopic and open approaches. Surg Endosc. 2015;29(6):1406–12. https://doi.org/10.1007/S00464-014-3814-1.
Halabi WJ, Jafari MD, Nguyen VQ, Carmichael JC, Mills S, Pigazzi A, et al. Ureteral injuries in colorectal surgery: an analysis of trends, outcomes, and risk factors over a 10-year period in the United States. Dis Colon Rectum. 2014;57(2):179–86. https://doi.org/10.1097/DCR.0000000000000033.
Marcelissen TAT, den Hollander PP, Tuytten TRAH, Sosef MN. Incidence of iatrogenic ureteral injury during open and laparoscopic colorectal surgery: a single center experience and review of the literature. Surg Laparosc Endosc Percutan Tech. 2016;26(6):513–5. https://doi.org/10.1097/SLE.0000000000000335.
Mayo JS, Brazer ML, Bogenberger KJ, Tavares KB, Conrad RJ, Lustik MB, et al. Ureteral injuries in colorectal surgery and the impact of laparoscopic and robotic-assisted approaches. Surg Endosc. 2021;35(6):2805–16. https://doi.org/10.1007/S00464-020-07714-1.
Riss S, Mittlböck M, Riss K, Chitsabesan P, Stift A. Intraoperative complications have a negative impact on postoperative outcomes after rectal cancer surgery. Int J Surg. 2014;12(8):833–6. https://doi.org/10.1016/J.IJSU.2014.07.003.
Eswara JR, Raup VT, Potretzke AM, Hunt SR, Brandes SB. Outcomes of iatrogenic genitourinary injuries during colorectal surgery. Urology. 2015;86(6):1228–34. https://doi.org/10.1016/J.UROLOGY.2015.06.065.
Summerton DJ, Kitrey ND, Lumen N, Serafetinidis E, Djakovic N. EAU guidelines on iatrogenic trauma. Eur Urol. 2012;62(4):628–39. https://doi.org/10.1016/J.EURURO.2012.05.058.
Gild P, Kluth LA, Vetterlein MW, Engel O, Chun FKH, Fisch M. Adult iatrogenic ureteral injury and stricture-incidence and treatment strategies. Asian J Urol. 2018;5(2):101–6. https://doi.org/10.1016/J.AJUR.2018.02.003.
Engel O, Rink M, Fisch M. Management of iatrogenic ureteral injury and techniques for ureteral reconstruction. Curr Opin Urol. 2015;25(4):331–5. https://doi.org/10.1097/MOU.0000000000000175.
da Silva G, Boutros M, Wexner SD. Role of prophylactic ureteric stents in colorectal surgery. Asian J Endosc Surg. 2012;5(3):105–10. https://doi.org/10.1111/J.1758-5910.2012.00134.X.
Hird AE, Nica A, Coburn NG, Kulkarni GS, Nam RK, Gien LT. Does prophylactic ureteric stenting at the time of colorectal surgery reduce the risk of ureteric injury? A systematic review and meta-analysis. Colorectal Dis. 2021;23(5):1060–70. https://doi.org/10.1111/CODI.15498.
Croghan SM, Zaborowski A, Mohan HM, Mulvin D, McGuire BB, Murphy M, et al. The sentinel stent? A systematic review of the role of prophylactic ureteric stenting prior to colorectal resections. Int J Colorectal Dis. 2019. https://doi.org/10.1007/S00384-019-03314-1.
Kanabur P, Chai C, Taylor J. Use of indocyanine green for intraoperative ureteral identification in nonurologic surgery. JAMA Surg. 2020;155(6):520–1. https://doi.org/10.1001/JAMASURG.2020.0094.
Mazzarella G, Muttillo EM, Picardi B, Rossi S, Rossi Del Monte S, Muttillo IA. Real-time intraoperative ureteral identification in minimally invasive colorectal surgery: a systematic review. J Laparoendosc Adv Surg Tech A. 2022;32(6):627–33. https://doi.org/10.1089/LAP.2021.0292.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. https://doi.org/10.1136/BMJ.N71.
Chahin F, Dwivedi AJ, Paramesh A, Chau W, Agrawal S, Chahin C, et al. The implications of lighted ureteral stenting in laparoscopic colectomy. JSLS. 2002;6(1):49–52.
Nam YS, Wexner SD. Clinical value of prophylactic ureteral stent indwelling during laparoscopic colorectal surgery. J Korean Med Sci. 2002;17(5):633–5. https://doi.org/10.3346/JKMS.2002.17.5.633.
Pokala N, Delaney CP, Kiran RP, Bast J, Angermeier K, Fazio VW. A randomized controlled trial comparing simultaneous intra-operative vs sequential prophylactic ureteric catheter insertion in re-operative and complicated colorectal surgery. Int J Colorectal Dis. 2007;22(6):683–7. https://doi.org/10.1007/S00384-006-0219-1.
Tsujinaka S, Wexner SD, DaSilva G, Sands DR, Weiss EG, Nogueras JJ, et al. Prophylactic ureteric catheters in laparoscopic colorectal surgery. Tech Coloproctol. 2008;12(1):45–50. https://doi.org/10.1007/S10151-008-0397-7.
Borowiec AM, Gill RS, Birch DW, Karmali S. The utility of lighted ureteral stents in laparoscopic colorectal resection: a survey of Canadian surgeons. Gastroenterology Res. 2011. https://doi.org/10.4021/GR344W.
Beraldo S, Neubeck K, von Friderici E, Steinmüller L. The prophylactic use of a ureteral stent in laparoscopic colorectal surgery. Scand J Surg. 2013;102(2):87–9. https://doi.org/10.1177/1457496913482247.
Speicher PJ, Goldsmith ZG, Nussbaum DP, Turley RS, Peterson AC, Mantyh CR. Ureteral stenting in laparoscopic colorectal surgery. J Surg Res. 2014;190(1):98–103. https://doi.org/10.1016/J.JSS.2014.02.025.
Pathak RA, Taylor AS, Alford S, Broderick GA, Igel TC, Petrou SP, et al. Urologic-induced complications of prophylactic ureteral localization stent placement for colorectal surgery cases. J Laparoendosc Adv Surg Tech A. 2015;25(12):966–70. https://doi.org/10.1089/LAP.2015.0345.
Boyan WP Jr, Lavy D, Dinallo A, Otero J, Roding A, Hanos D, et al. Lighted ureteral stents in laparoscopic colorectal surgery; a five-year experience. Ann Transl Med. 2017. https://doi.org/10.21037/ATM.2017.02.01.
Chiu AS, Jean RA, Gorecka J, Davis KA, Pei KY. Trends of ureteral stent usage in surgery for diverticulitis. J Surg Res. 2018;222:203-211.e3. https://doi.org/10.1016/J.JSS.2017.09.050.
Chong JT, Kan KM, Phillips CK, Greenstein A. Ureteral catheters for colorectal surgery: influence on operative times and complication outcomes: an observational study. Investig Clin Urol. 2018;59(2):119–25. https://doi.org/10.4111/ICU.2018.59.2.119.
Coakley KM, Kasten KR, Sims SM, Prasad T, Heniford BT, Davis BR. Prophylactic ureteral catheters for colectomy: a national surgical quality improvement program-based analysis. Dis Colon Rectum. 2018;61(1):84–8. https://doi.org/10.1097/DCR.0000000000000976.
Hassinger TE, Mehaffey JH, Mullen MG, Michaels AD, Elwood NR, Levi ST, et al. Ureteral stents increase risk of postoperative acute kidney injury following colorectal surgery. Surg Endosc. 2018;32(7):3342–8. https://doi.org/10.1007/S00464-018-6054-Y.
Merola J, Arnold B, Luks V, Ibarra C, Resio B, Davis KA, et al. Prophylactic ureteral stent placement vs no ureteral stent placement during open colectomy. JAMA Surg. 2018;153(1):87–90. https://doi.org/10.1001/JAMASURG.2017.3477.
Luks VL, Merola J, Arnold BN, Ibarra C, Pei KY. Prophylactic ureteral stenting in laparoscopic colectomy: revisiting traditional practice. J Surg Res. 2019;234:161–6. https://doi.org/10.1016/J.JSS.2018.09.041.
Shahait AD, Mesquita-Neto JWB, Girten K, Weaver D, Gruber SA, Gamal M. Iatrogenic ureteral injury and prophylactic stent use in veterans undergoing colorectal surgery. J Surg Res. 2021;265:272–7. https://doi.org/10.1016/J.JSS.2021.03.054.
Ryu S, Okamoto A, Nakashima K, Hara K, Ishida K, Ito R, et al. Ureteral navigation using a fluorescent ureteral catheter during laparoscopic colorectal surgery. Surg Endosc. 2021;35(8):4882–9. https://doi.org/10.1007/S00464-021-08538-3.
Dolejs SC, Nicolas M, Maun DC, Lane FR, Waters JA, Tsai BM. Localizing ureteral catheters for left-sided colectomy and proctectomy: do the risks justify the benefits? Am J Surg. 2022;223(3):505–8. https://doi.org/10.1016/J.AMJSURG.2021.12.025.
Ryu S, Hara K, Okamoto A, Kitagawa T, Marukuchi R, Ito R, et al. Fluorescence ureteral navigation during laparoscopic surgery for clinically suspected stage T4 colorectal cancer: a cohort study. Surg Oncol. 2022. https://doi.org/10.1016/J.SURONC.2021.101672.
Al-Taher M, van den Bos J, Schols RM, Bouvy ND, Stassen LPS. Fluorescence ureteral visualization in human laparoscopic colorectal surgery using methylene blue. J Laparoendosc Adv Surg Tech A. 2016;26(11):870–5. https://doi.org/10.1089/LAP.2016.0264.
Yeung TM, Volpi D, Tullis ID, Nicholson GA, Buchs N, Cunningham C, et al. Identifying ureters in situ under fluorescence during laparoscopic and open colorectal surgery. Ann Surg. 2016;263(1):e1–2. https://doi.org/10.1097/SLA.0000000000001513.
Barnes TG, Hompes R, Birks J, Mortensen NJ, Jones O, Lindsey I, et al. Methylene blue fluorescence of the ureter during colorectal surgery. Surg Endosc. 2018;32(9):4036–43. https://doi.org/10.1007/S00464-018-6219-8.
Mandovra P, Kalikar V, Patankar R. Real-time visualization of ureters using indocyanine green during laparoscopic surgeries: can we make surgery safer? Surg Innov. 2019;26(4):464–8. https://doi.org/10.1177/1553350619827152.
White LA, Joseph JP, Yang DY, Kelley SR, Mathis KL, Behm K, et al. Intraureteral indocyanine green augments ureteral identification and avoidance during complex robotic-assisted colorectal surgery. Colorectal Dis. 2021;23(3):718–23. https://doi.org/10.1111/CODI.15407.
Polom W, Migaczewski M, Skokowski J, Swierblewski M, Cwalinski T, Kalinowski L, et al. Multispectral imaging using fluorescent properties of indocyanine green and methylene blue in colorectal surgery-initial experience. J Clin Med. 2022. https://doi.org/10.3390/JCM11020368.
Soriano CR, Cheng RR, Corman JM, Moonka R, Simianu V, Kaplan JA. Feasibility of injected indocyanine green for ureteral identification during robotic left-sided colorectal resections. Am J Surg. 2022;223(1):14–20. https://doi.org/10.1016/J.AMJSURG.2021.07.012.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016. https://doi.org/10.1136/BMJ.I4919PHIPPS.
Phipps JH, Tyrrell NJ. Transilluminating ureteric stents for preventing operative ureteric damage. Br J Obstet Gynaecol. 1992;99(1):81. https://doi.org/10.1111/j.1471-0528.1992.tb14400.x. (PMID: 1547181).
Senagore AJ, Luchtefeld M. An initial experience with lighted ureteral catheters during laparoscopic colectomy. J Laparoendosc Surg. 1994;4(6):399–403. https://doi.org/10.1089/LPS.1994.4.399.
Pedro RN, Kishore TA, Hinck BD, Akornor JW, Dickinson L, Roychowdhury M, et al. Comparative analysis of lighted ureteral stents: lumination and tissue effects. J Endourol. 2008;22(11):2555–8. https://doi.org/10.1089/end.2008.0278. (PMID: 19046095).
van den Bos J, Al-Taher M, Bouvy ND, Stassen LPS. Near-infrared fluorescence laparoscopy of the ureter with three preclinical dyes in a pig model. Surg Endosc. 2019;33(3):986–91. https://doi.org/10.1007/S00464-018-6596-Z.
Friedman-Levi Y, Larush L, Diana M, Marchegiani F, Marescaux J, Goder N, et al. Optimization of liposomal indocyanine green for imaging of the urinary pathways and a proof of concept in a pig model. Surg Endosc. 2018;32(2):963–70. https://doi.org/10.1007/S00464-017-5773-9.
Verbeek FP, van der Vorst JR, Tummers QR, Boonstra MC, de Rooij KE, Löwik CW, et al. Near-infrared fluorescence imaging of both colorectal cancer and ureters using a low-dose integrin targeted probe. Ann Surg Oncol. 2014;21:528–37. https://doi.org/10.1245/S10434-014-3524-X.
Teranishi K. A near-infrared fluorescent probe coated with β-Cyclodextrin molecules for real-time imaging-guided intraoperative ureteral identification and diagnosis. Mol Pharm. 2020;17(7):2672–81. https://doi.org/10.1021/ACS.MOLPHARMACEUT.0C00364.
de Valk KS, Handgraaf HJ, Deken MM, Sibinga Mulder BG, Valentijn AR, Terwisscha van Scheltinga AG, et al. A zwitterionic near-infrared fluorophore for real-time ureter identification during laparoscopic abdominopelvic surgery. Nat Commun. 2019. https://doi.org/10.1038/S41467-019-11014-1.
Schols RM, Alic L, Beets GL, Breukink SO, Wieringa FP, Stassen LPS. Automated spectroscopic tissue classification in colorectal surgery. Surg Innov. 2015;22(6):557–67. https://doi.org/10.1177/1553350615569076.
Acknowledgements
The authors have no acknowledgments to report.
Author information
Authors and Affiliations
Contributions
PPB, AP, FT, AC and VB: equally contributed to the conceptualization and design of the study; PPB, CB and AP: analyzed the data. PPB and AP: wrote the first and final drafts of the review; VB, VC, AC and FC: supervised the manuscript; VB, CB and VC: offered significant intellectual contributions. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Pier Paolo Brollo and the other co-authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brollo, P.P., Puggioni, A., Tumminelli, F. et al. Preventing iatrogenic ureteral injury in colorectal surgery: a comprehensive and systematic review of the last 2 decades of literature and future perspectives. Surg Today 54, 291–309 (2024). https://doi.org/10.1007/s00595-022-02639-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02639-9